DIC syndrome is one of the most common and most severe, life-threatening disorders of the hemostatic system (hemostasis is a complex of body reactions aimed at preventing and stopping bleeding).
Synonyms for DIC syndrome are thrombohemorrhagic syndrome, consumption coagulopathy, hypercoagulability syndrome, defibration syndrome.
DIC syndrome (disseminated intravascular coagulation syndrome) is:
- a secondary pathological process that occurs with constant and prolonged stimulation of the hemostatic system;
- a pathological process that has a phase course, with initial activation and subsequent deep, increasing depletion of all parts of the hemostatic system up to the complete loss of the ability of blood to clot with the development of catastrophic uncontrolled bleeding and severe generalized hemorrhagic syndrome;
- a pathological process in which progressive diffuse intravascular coagulation is noted with multiple and widespread formation of blood microclots and aggregates of its formed elements, which worsens its rheological characteristics, blocks microcirculation in tissues and organs, causes ischemic damage in them and leads to multiple organ lesions.
Causes
The triggering factors for DIC syndrome can be a wide variety of intense or prolonged stimuli, one way or another fitting into Virchow's triad - disturbances in blood circulation, its properties or the vascular wall.
DIC syndrome occurs:
1. In case of violation of the rheological characteristics of blood and hemodynamics
- any kind of shock
- blood loss,
- intoxication,
- sepsis,
- Rhesus conflict pregnancy,
- circulatory arrest and subsequent resuscitation,
- gestosis,
- uterine atony,
- placenta previa,
- uterine massage
2. When blood comes into contact with damaged cells and tissues
- atherosclerosis,
- antenatal fetal death,
- oncological diseases
3. When the properties of the blood change and when thromboplastic substances enter the blood massively
- leukemia,
- amniotic fluid embolism,
- transfusion of incompatible blood,
- septic abortion,
- abruption of a normally located placenta with hemorrhage into the uterus,
- placenta accreta,
- uterine rupture,
- operations on parenchymal organs: uterus, liver, lungs, prostate, kidneys;
- acute radiation sickness,
- long-term compartment syndrome,
- gangrene,
- organ transplantation, chemotherapy, pancreatic necrosis, myocardial infarction, etc.).
Progression of disseminated intravascular coagulation
Deseminated intravascular coagulation begins with overactivity of the blood clotting system and excessive clotting in your body. Excessive blood clotting is usually stimulated by substances that enter the blood, with possible causes listed above.
As clotting factors and platelets are used up, there are fewer clotting factors available for use at the actual bleeding sites, resulting in severe bleeding.
The results of this process (ie, abnormal small blood clots (microthrombi) and/or bleeding) are found in many organs and tissues. Significant changes may occur in some organs in your body, such as the kidneys, lungs, brain, adrenal glands, or placenta.
Complications
Complications of DIC syndrome are as follows:
- acute renal failure (ARF);
- change in mental status;
- respiratory dysfunction;
- liver dysfunction;
- life-threatening thrombosis and hemorrhage (in patients with moderate to severe DIC);
- cardiac tamponade (fluid accumulates between the layers of the pericardium);
- hemothorax (accumulation of blood in the pleural cavity);
- intracerebral hematoma;
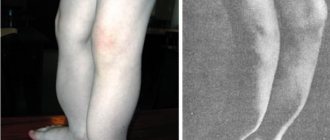
- gangrene and loss of limbs;
- shock;
- death.
Symptoms of DIC syndrome
During DIC syndrome there are 4 stages:
Stage 1 – phase of hypercoagulation and platelet hyperaggregation;
Stage 2 – transitional phase (multidirectional shifts in blood clotting both towards hyper- and hypocoagulation);
Stage 3 – deep hypocoagulation phase (blood does not clot at all);
Stage 4 – resolving phase (either hemostasis parameters are normalized, or complications develop that lead to death).
The symptoms of disseminated intravascular coagulation depend on many factors (the cause that caused it, the clinical picture of shock, disorders of all parts of hemostasis, thrombosis, reduced volume of the vascular bed, bleeding, anemia, dysfunction and dystrophy of target organs, metabolic disorders).
In the first phase, there is increased blood clotting, immediate formation of clots in large vessels and blood clots in small ones (during surgery). It is impossible to take blood from a patient for analysis, as it immediately clots. As a rule, the first phase proceeds very quickly and goes unnoticed by doctors. There is a sharp decrease in blood pressure, the skin is pale, covered with cold sticky sweat, the pulse is weak (thready). Then respiratory failure develops due to lung damage, a wet cough and crepitus in the lungs, cyanosis of the skin, cold feet and hands.
In the second phase, the same symptoms persist as in the first stage of DIC, plus the kidneys (renal failure), adrenal glands, and digestive tract are involved in the process (nausea, vomiting, abdominal pain, diarrhea). Microthrombi form in the brain (headache, dizziness, convulsions, loss of consciousness up to coma, paresis and paralysis, strokes).
The third phase (hypocoagulation stage) is characterized by massive bleeding, both from the original focus and from other organs (intestinal and gastric bleeding due to ulceration of the mucous membrane, blood in the urine - kidney damage, sputum mixed with blood when coughing).
The development of hemorrhagic syndrome is also characteristic (the appearance of massive hemorrhages, hematomas, petechiae, unstoppable bleeding at injection sites and during surgery, bleeding gums, nosebleeds, etc.).
The fourth phase, with timely and adequate treatment, leads to the restoration of hemostasis and stopping bleeding, but often ends in death with massive damage to internal organs and bleeding.
Thrombosis: normal or pathological?
In order to understand what the cause is and what are the mechanisms of occurrence of such a severe disorder as DIC syndrome, you need to know the main stages of blood coagulation.
A person is constantly faced with the risk of possible injuries, from minor scratches or cuts to serious wounds, so nature provides a special protective mechanism - thrombosis, that is, the formation of a blood clot at the site of vessel damage.
There are two oppositely directed systems in the body - coagulation
and
anticoagulant , the correct interaction of which promotes thrombus formation if necessary, as well as the liquid state of blood in the vessels in the absence of any damage.
These hemostatic systems play a very important protective role. Blood clot formation
When the integrity of the vascular wall is violated, the coagulation system is activated, a whole cascade of reactions of which leads to the formation of a thrombus (a clot in the lumen of a vessel or chamber of the heart). Plasma proteins, in particular fibrinogen, as well as platelets, coagulation factors produced in the liver, and various enzymes are directly involved in this. The result is the formation of a blood clot that closes the defect in the vascular wall and prevents further bleeding.
To maintain the fluid state of the blood and prevent the uncontrolled formation of blood clots, there are specific antithrombotic mechanisms
, realized by the action of so-called
anticoagulants
- substances that prevent the occurrence of massive thrombosis (plasma proteins, proteolytic enzymes, endogenous heparin). In addition, an obstacle to thrombosis is rapid blood flow and so-called fibrinolysis, that is, the dissolution of the fibrin protein and its removal from the vascular bed with the help of enzymes circulating in the blood plasma and secreted by leukocytes, platelets and other cells. The remains of fibrin after its destruction are absorbed by leukocytes and macrophages.
When the interaction of the components of the hemostatic system changes in various diseases and injuries, discoordination occurs in the work of the coagulation and anticoagulation systems , which contributes to massive uncontrolled thrombus formation along with bleeding. These mechanisms form the basis of the pathogenesis of DIC syndrome, which is a life-threatening complication.
Diagnostics
Basic laboratory tests:
- determination of platelets (with DIC syndrome there is a decrease in platelets in phases 2, 3 and 4);
- blood clotting time (the norm is 5 – 9 minutes, in the 1st stage the indicator is shortened, in subsequent stages the time is lengthened);
- bleeding time (normal 1 – 3 minutes);
- APTT (activated partial thromboplastic time - increase in phases 2 and 3 of DIC syndrome);
- prothrombin time, thrombin time, determination of activated plasma recalcification time - AVR (increase in the second and third stages of DIC syndrome);
- clot lysis (normally not, in phase 3 lysis is rapid, and in phase 4 a clot does not form);
- fibrinogen (normal 2 – 4 g/l, decreases in stages 2, 3 and 4);
- study of the phenomenon of fragmentation of erythrocytes due to damage to them by fibrin threads (normally the test is negative, a positive test indicates disseminated intravascular coagulation syndrome);
- decreased red blood cells (anemia, decreased blood volume);
- decreased hematocrit (hypovolemia);
- determination of acid-base and electrolyte balance.
Appendix B. Patient management algorithms
Appendix B1. Algorithm for diagnosis and correction of DIC syndrome
Appendix B2. Algorithm for correction of coagulopathic bleeding (DIC syndrome)a
Appendix B3. Algorithm for the use of factor VII and prothrombin complex concentrate for coagulopathic bleeding (DIC syndrome)
Treatment of DIC syndrome
Therapy for DIC syndrome is carried out by a doctor who has encountered this pathology (that is, the attending physician) together with a resuscitator. In the chronic course of DIC syndrome, its treatment is carried out by a therapist and a hematologist.
First of all, it is necessary to eliminate the cause of DIC syndrome. For example, for sepsis, antibacterial and transufusion (intravenous infusion of blood products) therapy is prescribed, for traumatic shock - adequate pain relief, immobilization, oxygenation and early surgical intervention. Or for tumor diseases - chemotherapy and radiotherapy, for myocardial infarction - relief of pain, restoration of heart rhythm and hemodynamics, for obstetric and gynecological pathologies, radical measures (hysterectomy, cesarean section).
Restoration of hemodynamics and rheological properties of blood is carried out through infusion-transfusion infusions.
An infusion of fresh frozen plasma is indicated, which not only restores the volume of circulating blood, but also contains all coagulation factors.
Crystalloid (saline, glucose) and colloid solutions (polyglucin, rheopolyglucin) in a 4/1 ratio and protein blood products (albumin, protein) are also administered.
A direct anticoagulant is prescribed - heparin. The dose of heparin depends on the stage of DIC syndrome (in phases 1–2 it is significant). In case of significant anemia, fresh (no more than 3 days) red blood cells are transfused.
In the treatment of severe generalized DIC, fibrinogen and blood clotting factor concentrates (cryoprecipetate) are used. Proteolysis inhibitors - antiproteases - are used to suppress tissue proteases that are released when cells are damaged (contrical, trasylol, gordox). Corticosteroids (hydrocortisone, dexamethasone) are also prescribed, as they increase blood clotting.
In parallel, the fight against multiple organ failure is being carried out (supporting the functions of the lungs, kidneys, gastrointestinal tract, adrenal glands). In phases 2–4 of DIC, a mixture of aminocaproic acid, dry thrombin, sodium ethamsylate and adroxon is used to restore local hemostasis. This mixture is introduced into the abdominal cavity through drainages, orally, in the form of tampons into the uterine and vaginal cavity, and wipes moistened with the solution are applied to the wound.
The entire process of intensive therapy takes 1–5 days (depending on the severity of DIC), and subsequent treatment continues until complete or almost complete recovery of all multiple organ disorders.
Home / Publisher / DIC syndrome as one of the manifestations of the systemic inflammatory response
2.2.2. DIC syndrome as one of the manifestations of the systemic inflammatory response
Disseminated intravascular coagulation is a dynamic pathological process characterized by a sequential change of generalized hypercoagulation with intravascular coagulation, platelet aggregation, blockade of microcirculation and hypocoagulation with hypofibrinogenemia and consumption thrombocytopenia.
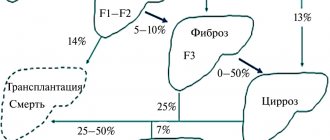
DIC syndrome is a nonspecific process that aggravates the most diverse forms of pathology: myocardial infarction complicated by cardiogenic shock, various types of malignant neoplasms, extensive surgical interventions, severe hypoxia, transfusion of incompatible blood, systemic lupus erythematosus, immune complex diseases, cirrhosis liver, obstetric pathology (premature placental abruption, amniotic fluid embolism, intrauterine fetal death) (Baluda V.P., 1979; Gavrilov O.K., 1981; Barkagan Z.S., 1983).
Disseminated intravascular coagulation often occurs in such critical conditions as severe infections, septicemia, sepsis, septic shock, being a manifestation of the systemic inflammatory response syndrome.
According to summary statistics from large multidisciplinary clinical centers, the first place among the causes of DIC is occupied by generalized bacterial and viral infections and septicemia. They account for up to 50% of pathology (Barkagan Z.S., 1981). The development of DIC syndrome during septic infection is largely a cytokine-mediated process (St.schon RC., Dorinsky PM, 1993; A. Gullo, 1997).
Regarding the pathogenesis of disseminated intravascular coagulation, which in some cases is a manifestation of a systemic inflammatory response during massive traumatic tissue damage, surgical interventions, birth injuries, septic infections, it should be noted the general patterns of development of disseminated intravascular coagulation, including the following initiating mechanisms of development:
1. Primary damage to the vascular wall, desquamation of the endothelium, exposure of subendothelial proteins: collagen, thrombospodin, fibronectin, von Willebrand factor, which have the ability to activate the processes of platelet adhesion and aggregation, activate Hageman factor XII with subsequent activation of the internal mechanism of formation of pro- thrombinase activity, complement system, fibrinolysis, kallikrein-kinin systems. Thus, the platelet component of the hemostasis system and coagulation hemostasis are simultaneously activated, combined with further destruction of the vascular wall under the influence of vasoactive complement components and the kallikrein-kinin system.
It should be noted that damage to endothelial cells invariably entails the release of tissue thromboplastin (III factor of blood coagulation, the source of formation is the endothelium and smooth muscle elements of blood vessels) and, accordingly, activation of the external mechanism of prothrombinase formation with the participation of plasma factor VII and Ca ions . And in this case, the induction of the external mechanism of prothrombinase formation, as with the activation of the internal mechanism, increases fibrinolytic reactions due to the fact that the damaged endothelium is a source of tissue-type plasminogen activators.
These mechanisms of simultaneous activation of the platelet-vascular link of the hemostasis system, coagulation hemostasis and fibrinolysis can be initiated in various areas of the microcirculation, very remote from the zone of alterative-destructive processes, both under the influence of bacteria, viruses, toxins, especially endotoxin of gram-negative bacteria, immune complexes, as well as various mediators of inflammation of humoral and cellular origin (Bakhdarchyan E.A., Palchikova E.I., 1984; Pak S.G., Sinelnikova M.N., Tsukerman D.B. et al ., 1987; Orlov V.A., Yakunin G.A., 1987; Grachev S.V., Yakunin G.A., Novachadov V.V., Yaroshenko I.F., 1992).
2. The primary preferential effect of the pathogenic factor on platelets, induction of adhesion processes, platelet aggregation, release of biogenic amines from platelets, platelet coagulation factors, in particular 3 and 4, initiating the formation of thrombin with possible subsequent activation under the influence of thrombin of a number of factors in the formation of prothrombinase, the development of a cascade of reactions of secondary activation of coagulation hemostasis.
Bacterial endotoxins, immune complexes, and antibodies have the ability to be intensively accepted by platelets. In this regard, pronounced activation of the platelet component of the hemostasis system is observed during inflammatory processes of a bacterial and immuno-allergic nature.
3. Combined almost simultaneous effect of bacterial toxic, immunoallergic factors on the platelet-vascular and coagulation parts of the hemostasis system.
4. Development of alternative mechanisms of hemocoagulation due to activation of the monocyte-macrophage and erythrocyte components of the hemostasis system.
As is known, the cellular elements of the mononuclear phagocytic system play an extremely important role in endocytosis, processing of antigens and presenting them to T helper cells in complex with the Ia protein. However, it should be noted that antigen-stimulated mononuclear phagocytes can synthesize about 100 different biologically active compounds - monokines, and among the monokines there is a group of highly active compounds that regulate the processes of hemostasis and fibrinolysis in the event of the development of nonspecific pathological reactions, the syndrome of systemic action of inflammation on organism (Dinarello CA, Cannon JG, Wolff SM, 1988; Yacobs RF, Tabor DR, 1989; Shalaby MR, Waage A., Aarden L. et al., 1989; Cotran RS, Pober JS, 1990).
Under physiological conditions, monocytes and tissue macrophages practically do not produce hemocoagulation and fibrinolysis factors.
In the area of inflammation, monocytes, tissue macrophages, activated by endotoxin, tissue breakdown products, begin to synthesize and secrete into the environment various regulators of the hemostatic potential of the blood, in particular, tissue thromboplastin, K-dependent blood coagulation factors and some K-independent (V, VII, IX, X), and X factor is synthesized by macrophages in a partially activated form.
Macrophage cytokines also include fibronectin, thrombospondin, proteoglycans, which ensure the processes of platelet adhesion and aggregation, that is, the initial mechanisms of activation of the platelet component of the hemostasis system.
Macrophages can also provide alternative regulation of fibrinolysis activity in the inflammatory zone and beyond in the event of the development of systemic inflammatory response syndrome due to the secretion of plasminogen activator, as well as plasminogen and plasmin inhibitors.
Unlike macrophages, other types of leukocytes lack the ability to produce thromboplastin and other clotting activators.
With the development of a number of bacterial infections and intoxications, characterized by intensive release into the bloodstream of endotoxins, exotoxins with hemolyzing activity, pathogenicity enzymes, as well as in cases of secondary excessive accumulation of lipid peroxidation products in erythrocytes, leading to destabilization of erythrocyte membranes and increased hemolysis of erythrocytes , certain shifts in the hemostatic potential of the blood caused by hemolyzed erythrocytes are possible.
As is known, when erythrocyte membranes are damaged, hemostasis is activated due to the release of ADP and membrane phospholipid matrices. At the same time, factors of the coagulation and fibrinolytic systems are intensively sorbed on the membrane phospholipid matrices of erythrocytes. Micromembranes of erythrocytes are capable of acting as matrices in the mechanisms of formation of prothrombinase activity along the internal pathway of activation of the coagulation system (Ashkinazi I.Ya., 1977).
Thus, pathogenic factors that are different in nature, causing the development of a local inflammatory process and systemic inflammatory response syndrome, cause activation of the procoagulant blood system due to massive generalized damage to the vascular wall, increasing its adhesive properties, and activation of the platelet component of the hemostasis system , and in some cases, monocyte-macrophage and erythrocyte alternative pathways of hemocoagulation.
Naturally, in each specific case of pathology, it is possible to identify certain specifics of the initiating mechanisms of activation of the coagulation, platelet-vascular components of the hemostasis system, but very quickly in the dynamics of the pathology, due to the cascade of mutually modulating reactions of hemostasis, the specific features of coagulation disorders are lost -on potential of the blood, a hypercoagulation phase occurs, followed by hypocoagulation of consumption.
The following phases should be distinguished in the development of DIC syndrome:
I. Hypercoagulation and aggregation of blood cells.
II. Transition from hypercoagulation to hypocoagulation.
III. The stage of deep hypocoagulation, up to complete non-coagulation of blood, is caused by the consumption, blockade and breakdown of a number of blood coagulation factors, the accumulation and circulation of their breakdown products, which have anticoagulant activity, as well as thrombocytopenia of consumption.
IV. The recovery stage with a favorable course of the disease, or the stage of formation of multiple organ failure in the case of the predominance of mechanisms of decompensation and damage.
DIC syndrome can be acute, subacute, chronic and recurrent in nature (Gavrilov O.K., 1981).
The acute form occurs with septic infections, extensive surgical interventions, blood loss, burns, transfusion of incompatible blood, as well as placental abruption, amniotic fluid embolism, intrauterine fetal death, uterine atony, septic abortion, traumatic, hemorrhagic, cardiogenic, anaphylactic shock.
In the case of acute DIC syndrome, the hypercoagulation phase is extremely short-lived.
The subacute course of DIC occurs in renal failure, malignant neoplasms, and leukemia.
Recurrent and chronic forms can occur in cancer, systemic inflammatory autoimmune diseases and other forms of pathology.
The possibility of local damage to the microcirculation during disseminated intravascular coagulation within a particular organ and generalized disorders is noted. (Ma-chabeli M.S., 1970; Baluda V.P., 1979).
Regarding the clinical picture of DIC, it should be noted that it primarily consists of the symptoms of the underlying disease inducing the development of DIC, as well as the phenomena of hemocoagulation shock, phase shifts in hemostasis and fibrinolysis.
DIC syndrome, which began with shock, always has a more severe outcome than non-shock forms (Barkagan Z.S., 1988).
In the clinical picture, it is extremely difficult to monitor the transformation of septic, traumatic, hemorrhagic, cardiogenic shock into hemocoagulative shock, since the characteristic nonspecific signs of shock of various etiologies are the initial development of peripheral vascular spasm, centralization of blood flow, which is combined with normal or elevated blood pressure levels , cyanosis, shortness of breath, oligoanuria, cold extremities (hyperdynamic phase of shock).
However, as the pathology progresses, decentralization of blood flow occurs, pathological blood deposition, microvascular paresis, sludge syndrome, a progressive drop in blood pressure up to critical values, severe microcirculation disorders in peripheral organs and tissues, multiple organ failure (renal, liver, adrenal insufficiency, shock lung).
In the diagnosis of DIC syndrome, important importance is given to the dynamics of such laboratory parameters of hemostasis as the number of platelets, fibrinogen level, thrombin time, prothrombin time, partial thromboplastin time, antithrombin III level, fibrinogen level, ethanol and protamine sulfate tests.
It should be noted that laboratory studies of hemostasis can reveal both a tendency to thrombus formation, hypercoagulation shifts, and hypocoagulation disorders.
In acute DIC, rapid development of thrombocytopenia and hypofibrinogenemia is possible. True afibrinogenemia practically never occurs in DIC; increased binding of fibrinogen to fibrin monomers and the formation of soluble fibrin are often observed. In protracted and chronic forms of DIC, hypofibrinogenemia is extremely rare, since this form of DIC often occurs against the background of initial hyperfibrinogenemia, characteristic of many protracted forms of infectious and inflammatory processes (Barkagan Z.S., 1988), initiating the development of DIC syndrome.
Thrombocytopenia of consumption almost always accompanies acute and subacute DIC syndrome.
In the initial phase of DIC, a large number of platelet aggregates are detected in the peripheral blood, combined with a decrease in the aggregation function of the cells remaining in the bloodstream. The latter is due to the toxic effect on platelets of tissue breakdown products, bacterial, toxic and enzymatic factors of pathogenicity, free radicals, the inhibitory effect on the process of aggregation of fibrin degradation products, the return of part of platelets from microthrombi to the circulation, already subjected to exhaustion (Barkagan Z.S., 1988).
With slowly progressing DIC, the platelet count may be normal or even elevated.
An important diagnostic sign of DIC syndrome is damage, fragmentation of erythrocytes, the appearance of their fragments, up to the formation of clinical and laboratory signs of erythrocyte hemolysis.
In acute and subacute forms of DIC, prothrombin time is increased due to a decrease in the activity of factor V and fibrinogen levels; Thrombin time is usually increased, which is due to hypofibrinemia and the inhibitory effect of fibrinogen degradation products (FDP).
FDPs inhibit the coagulating activity of platelets and the process of fibrin clot polymerization.
In DIC syndrome, as a rule, the paracoagulation reaction is positive using the protamine sulfate and ethanol test to determine the soluble fibrin monomer (Gavrilov O.K., 1981)
Direct confirmation of DIC is the detection of blood clots in the microcirculation system, as well as the detection of fibrinopeptides A and B.
An important diagnostic test for DIC syndrome is the level of antithrombin III in the blood. At stage I of DIC - hypercoagulation, when there is pronounced activation of serine proteases - thrombin and factor Xa, heparin in combination with antithrombin III inactivates these proteases. Subsequently, heparin is inhibited by platelet factor 4, and in the process of inactivation of serine proteases, antithrombin III is intensively consumed, which leads to its rapid depletion. The level of antithrombin III in the blood decreases rapidly. As a rule, in the hypercoagulation phase, another anticoagulant, protein C, is also intensively consumed.
A decrease in antithrombin III and protein C in acute forms of DIC outpaces the depression of blood coagulation factors. If antithrombin III decreases to 75%, heparin resistance and thrombogenicity occur, since antithrombin III is a cofactor of heparin.
Relatively early in DIC, the plasma levels of some plasminogen activators (prekallikrein, a high-molecular kinin gene) also decrease. With deep damage to the endothelium, the level of von Willebrand factor in the blood increases.
It should be noted that in phase II of DIC syndrome (transition from hyper- to hypocoagulation), multidirectional shifts in many indicators occur, when some tests still indicate hypercoagulation, while others indicate hypocoagulation.
In contrast to the above-described shifts in hemostasis parameters characteristic of acute and subacute forms of DIC, diagnosis is often difficult in chronic DIC.
In the hypercoagulation phase of the chronic form of DIC, an increase in the activity of procoagulant factors, hyperfibrinogenemia, thrombocytosis, and a decrease in partial thromboplastin time were noted. In chronic forms of DIC, both the development of thrombocytosis and the development of thrombocytopenia and hypofibrinogenemia can occur.
One of the frequent and dangerous manifestations of DIC is the development of hemorrhagic syndrome, which occurs in the acute form of DIC in the hypocoagulation phase. However, in a number of cases, already in the early phase of hyper-coagulation or in the transition phase from hyper- to hypo-coagulation, multiple hemorrhages occur against the background of normal or reduced fibrinogen content in the blood. An increase in bleeding is characterized by the appearance of bruises, hematomas, hemorrhages in various organs, diffuse sweating of blood into the abdominal and pleural cavities, the development of nasal, gastrointestinal, pulmonary, renal, and uterine bleeding.
Increased bleeding in DIC leads to the development of posthemorrhagic anemia, and in severe cases to hemorrhagic shock.
A characteristic feature of DIC syndrome is the blockade of microcirculation in various organs and tissues with subsequent disruption of their trophism and functional activity.
The shock organs in DIC syndrome are the lungs, kidneys, stomach and intestines; the liver is less commonly affected.
Blockage of pulmonary vessels by fibrin microclots, blood cell aggregates, and excessive accumulation of vasoactive compounds in the lungs lead to the development of pulmonary edema, the appearance of pulmonary infarctions, and respiratory distress syndrome. The latter is characterized by the appearance of shortness of breath, cyanosis, hypoxemia and hypercapnia.
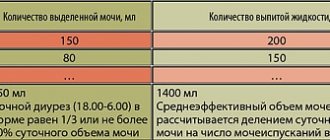
Disorders of systemic hemodynamics and microcirculation in DIC lead to the development of prerenal and renal forms of renal failure, the characteristic signs of which are oligoanuria, the appearance of protein, casts, and red blood cells in the urine, an increase in residual non-protein nitrogen in the blood, disorders of electrolyte balance and acid-base balance. condition.
Severe combined complications of DIC syndrome are often observed in the form of shock lung and acute renal failure, or renal and liver failure. Often, with renal failure, hemolytic-uremic syndrome develops.
Microthrombosis and stasis in the vessels of the mucous membrane of the duodenum and stomach, the appearance of many hemorrhages lead to profound dystrophic changes in the mucosa, disruption of the reparative regeneration of the mucosa, and the appearance of acute erosions and bleeding.
Secondary liver damage in DIC syndrome is much less common and is manifested by the development of parenchymal jaundice. More often, disturbances in the structure and function of the liver precede the development of DIC, being one of its causes.
With disseminated intravascular coagulation syndrome of septic origin, as well as complicating various types of shock, the development of adrenal insufficiency and centrogenic diabetes insipidus is possible.
previous section | content| next section