Dermatomyositis is an inflammatory diffuse disease of connective tissues, smooth and skeletal muscle fibers, skin and internal organs. If there is no skin symptom, they speak of polymyositis. Dermatomyositis manifests itself in the form of the following symptoms: muscle weakness, fever, migraines, polyarthralgia. The basis for diagnosing pathology is biochemical and laboratory results. An effective way to alleviate or eliminate problems is hormonal; the course of the disease is wavy.
Dermatomyositis: symptoms and treatment
There is a connection between dermatomyositis with viral infection and genetic factors. The chronic survival of microbes in muscle tissue, the similarity of viral and muscle systems leads to the appearance of autoantibodies to muscles. The starting point for the formation of dermatomyositis can be an exacerbation of an infectious virus, severe depression, hypothermia, allergies, vaccination, hyperthermia.
In the article we will consider the following: dermatomyositis: symptoms and treatment of this pathology, diagnosis and reasons for its development.
Types of dermatomyositis
Dermatomyositis is a systemic, intensifying pathology, due to which muscle tissue and skin are primarily affected, the functioning of organs is disrupted, which can be accompanied by a purulent infection. A quarter of patients do not have skin diseases. In this case, polymyositis is implied. Dermatomyositis belongs to a class of inflammatory neuromuscular diseases. In 25% of cases, secondary tumor pathology is observed. The disease can be acute, subacute or chronic.
Polymyositis is a type of pathology in which no skin diseases are observed.
The development of dermatomyositis is accompanied by a prodromal stage, clinical symptoms and a period of exacerbation. The disease can occur with different manifestations of inflammatory activity (from 1 to 3).
Diagnostics
The doctor interviews the patient, conducts a physical examination, collects a complete history of the disease, and gives directions for the necessary studies.
The diagnosis of amyopathic dermatomyositis is established for patients in whom skin lesions characteristic of dermatomyositis are confirmed by biopsy results. However, laboratory and instrumental diagnostic methods did not reveal clinical signs of muscle tissue damage.
Additionally, such patients may be tested for the presence of malignant neoplasms (dermatomyositis is associated with cancer) or interstitial lung disease.
Causes of pathology
To date, the reason is undisclosed. It is believed that the main prerequisite for the appearance of pathology is viral infection, but no clinical or laboratory studies can yet prove this with 100% probability. An important component is the autoimmune process. 15% of the considered myopathies are associated with oncological pathologies, in which most often we are talking about dermatomyositis.
The disease begins to manifest itself as mild weakness, malaise, elevated body temperature, loss of weight and appetite, skin disease with a subsequent increase in the disease in the hips and shoulders. Dermatomyositis can occur slowly over several months, or immediately take an acute form, which most often occurs in the younger generation.
2. Reasons
Dermatomyositis is a polyetiological process, i.e. occurs (like rheumatic diseases, to the group of which it is often classified) under the influence of one of many possible causes, or a combination of them, or without any apparent reason at all. Typically, such a statement is alarming, meaning that either the real cause has not yet been established, or the disease is triggered by a rare combination of some unfavorable factors and/or conditions. In the case of EBM, both are true to a certain extent. Today, the theoretical understanding of the etiopathogenesis of dermatomyositis is dominated by infectious-toxic hypotheses, and the role of both viral and bacterial agents is statistically confirmed. In turn, pathogenic viruses and bacteria that cause (or can cause) the development of DM are also very numerous and heterogeneous. In addition, researchers have repeatedly drawn attention to the regional and seasonal dependence of the frequency of occurrence of DM, suggesting a provoking effect of direct intense sunlight.
Visit our Dermatology page
Risk factors
Dermatomyositis more often affects women than men.
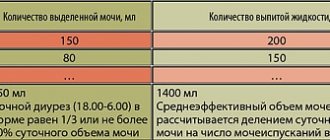
Table. Distribution of 150 patients with dermatomyositis (polymyositis) by clinical groups and gender.
| Diagnosis | Percentage of patients | Percentage of women |
| Polymyositis | 34 | 69 |
| Dermatomyositis | 29 | 58 |
| Dermatomyositis or polymyositis in children | 7 | 36 |
| Dermatomyositis or polymyositis in combination with a neoplasm (benign or malignant) | 8.5 | 57 |
| Dermatomyositis or polymyositis in combination with other diffuse connective tissue pathologies | 21 | 90 |
Classification
In approximately 25-30% of cases, there are no skin symptoms and then they speak of a special case of this systemic disease - polymyositis .
Depending on the origin and course, the following are distinguished:
- primary idiopathic dermatopolymyositis;
- the secondary paraneoplastic or tumor type occurs in individuals over 55 years of age against the background of cancer of the breast , lungs , ovaries , prostate , uterus , stomach , colon , hemoblastosis and other malignant neoplasms;
- juvenile - children's;
- polymyositis , combined with other diffuse connective tissue diseases.
Juvenile dermatomyositis: features of the course
It is distinguished by focal calcification of soft tissues such as muscles, epidermis and subcutaneous fat. Deposits of calcium salts - hydroxyapatites - can be deposited on the surface and deep, forming limited single or diffusely located nodules and pseudotumors. Superficial plaques with calcifications cause inflammatory reactions of surrounding tissues; they rot and are rejected in the form of a crumbly mass.
Subcutaneous calcifications
As in adults, classic rashes and Gottron's sign are observed. Gradually increasing muscle weakness begins with a bizarre gait of the child, which further constrains movement even more, preventing the child from playing, running and caring for himself.
Juvenile dermatomyositis
Symptoms of pathology
The clinical picture of the disease is gradually developing. At the onset of dermatomyositis, one can detect increasing weakness of muscle tissue, which can worsen over several years. Acute development is not particularly characteristic of dermatomyositis. The main symptoms may be accompanied by skin irritation and Raynaud's syndrome.
Raynaud's syndrome
There is weakness in the neck and arms, which can interfere with daily work. In more advanced forms of the disease, patients find it difficult to get out of bed, hold their head up, and find it difficult to walk independently.
Damage to the muscles of the throat and upper digestive canals leads to unclear speech, difficulties during swallowing and passing food. Violation of the diaphragm and intercostal tissues leads to malfunction of the lungs and the development of pneumonia. A characteristic feature of dermatomyositis is infection of the skin. Swelling of the face, a rash on the cheeks, in the area of the nasolabial folds, chest, and shoulder blades appear.
Symptoms of dermatomyositis
Wagner's disease is a whole sympathocomplex, caused primarily by generalized disorders of the microcirculatory bloodstream and manifested in various organs and systems, most of all in the epidermis and muscles.
Skin manifestations of dermatomyositis
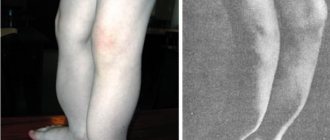
Gottron's symptom is the presence of pink and bright red scaly papules, plaques localized on the extensor surfaces of the joints, such as: interphalangeal and metacarpophalangeal folds, elbow and knee bends. Mild redness may spontaneously regress and be completely reversible.
An unusual heliotrope rash also characterizes dermatomyositis, the skin manifestations are purple or red in color, are located mainly on the upper mobile eyelids and are combined with periorbital swelling, also often called the symptom of “purple dermatomyositis glasses”. The location of the rash may also resemble a shawl, affecting the V-shaped area of the chest, neck, abdomen, upper back and arms, thighs and buttocks. In appearance it can resemble tree branches of a burgundy-bluish color such as telangiectasia and livedo .
Skin manifestations of dermatomyositis: A - purple glasses, B, C - heliotrope rash, D - erythematous changes in the “hand of the craftsman”
Patients develop photodermatitis - increased sensitivity to sunlight on the exposed surface of the skin.
An early symptom of dermatomyositis is considered to be changes in the nails - redness and growth of the skin around the nail plate.
Manifestations of systemic muscle damage
The main symptoms of polymyositis are atrophy and muscle weakness , which is usually symmetrical and involves the shoulder and pelvic girdle, neck flexors and abdominal muscles in the pathological process, manifested by the difficulty of climbing stairs, getting up from a chair, and holding the head.
The most dangerous thing is when the respiratory, oculomotor and swallowing muscles are affected, because this provokes respiratory failure , disorientation and diplopia , difficulties during the act of swallowing ( dysphagia ), hoarseness and voice changes. The inflammatory process in the muscles can be accompanied by a pain syndrome - myalgia. Impaired blood supply and trophism causes a decrease in muscle mass, the development of severe necrotizing myositis , which results in the proliferation of connective tissue in muscle fibers and the formation of compactions, as well as tendon-muscular contractures .
The effect on the cardiovascular system causes not only pathology of the myocardium - myocarditis , but also of the coronary vessels and all three linings of the heart, provoking tachycardia , arterial hypotension , muffled tones, dilated cardiopathy , heart rhythm disturbances, up to AV block and heart attack .
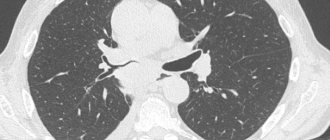
Changes in the lungs
Usually these are secondary complications caused by hypoventilation as a result of weakness of the respiratory muscles and diaphragm, the development of infection, and aspiration during swallowing. Most often they lead to fibrosing alveolitis , basal pulmonary fibrosis , interstitial pneumonia and even metastatic neoplasms. The main manifestations are symptoms such as:
- dyspnea;
- wheezing;
- nonproductive cough ;
- cyanosis;
- crepitation - a crunching sound detected during auscultation;
- reduction in lung volumes and diffusion characteristics.
Other manifestations of dermatopolymyositis
- stiffness of movement - due to damage to the joints (arthralgia and arthritis), which may be accompanied by swelling and pain;
- low-grade fever – up to 38° in acute phases;
- the development of gastritis , colitis , erosive and ulcerative lesions and hemorrhage in almost 50% of cases lead to weight loss and are provoked by changes in blood vessels and disturbances in the nutrition of the gastrointestinal mucosa, the patency of nerve impulses and peristalsis ;
- Raynaud's syndrome - numbness of the hands and cold fingers after exposure to cold, emotional stress , or without obvious reasons, which ultimately causes pain and swelling, purplish-red color of the skin;
- conjunctivitis , stomatitis and other mucosal lesions;
- moderate hepatomegaly and minor liver dysfunction;
- lymphadenopathy - the presence of dense widespread edema;
- sensitivity disorders - hyperesthesia , hyperalgesia , areflexia , most often caused by polyneuritis ;
- hormonal imbalance , accompanied by functional disorders of the gonads and the pituitary-adrenal system.
Diagnosis of dermatomyositis
- laboratory factors;
- muscle biopsy.
Polymyositis should be suspected when proximal muscle weakness is detected in a patient, without underlying pain in the muscles. The accuracy of diagnosing the disease becomes higher if the presence of the following problems can be confirmed:
- proximal muscle weakness;
- skin rash;
- excessive work of muscle enzymes. In the absence of excessive amounts of creatine kinase, it is worth testing for increased aldolase or aminotransferase, which are not as specific as compared to creatine kinase;
- disorders in muscle tissue, which can be detected by doing MRI and electromyography;
- abnormalities found on muscle biopsy.
A muscle biopsy is recommended to make a diagnosis.
Muscle biopsy will help eliminate clinically similar manifestations, including myositis and rhabdomyolysis, which is caused by viral infection. The existing disorders detected during histological examination can be of a different nature, but what they have in common are: places of degeneration and regeneration of muscle tissue, inflammatory reactions. Before starting treatment, you should make sure the diagnosis is accurate. This can be done using histological verification. They are carried out in order to exclude even the slightest possibility of the presence of other muscle pathologies. To increase the degree of awareness of histological examination, a biopsy specimen should be taken from a muscle that corresponds to as many of the following features as possible:
Publications in the media
Dermatomyositis (DM) and polymyositis are idiopathic inflammatory myopathies characterized by systemic damage to striated and smooth muscles with impaired motor function, and in DM also skin damage in the form of erythema and edema, mainly in open areas of the body. The following types of idiopathic inflammatory myopathies are distinguished: • polymyositis • dermatomyositis • polymyositis as part of systemic connective tissue diseases • paraneoplastic polymyositis and DM • polymyositis with intracellular inclusions. Statistical data. The incidence is 0.2–0.8 per 100,000 population. Predominant age: two peaks of incidence are determined - at the age of 5–15 and 40–60 years. The predominant gender is female (2:1). The etiology is unknown • The possible etiological role of viral factors, primarily picornaviruses, is discussed • The presence of a connection between oncopathology and DM suggests an autoimmune reaction caused by antigenic mimicry of tumor tissue and muscle tissue.
Pathogenesis. It is assumed that in the pathogenesis of DM the main role belongs to humoral reactions that occur with activation of complement and lead to the development of vasculopathies, while in polymyositis the main role is given to cellular cytotoxic reactions. Differences in pathogenesis are reflected in the histological picture. In DM, CD4+ T-lymphocytes, B-lymphocytes and macrophages are found in perivascular infiltrates. With polymyositis, mononuclear infiltrates containing cytotoxic CD4+ T lymphocytes are found in the endomysium (the result of cytotoxic reactions is myofibril necrosis). In polymyositis and DM, myositis-specific antibodies are detected, but their pathogenetic significance is disputed. Clinical picture • Proximal muscle weakness: difficulty combing your hair, brushing your teeth, getting up from a low chair, getting into a vehicle • Skin damage •• photodermatitis and “heliotropic” edema of the paraorbital region •• erythema of the skin of the face and in the “décolleté” area •• erythematous scaly rashes over the small joints of the hands (Gotron's symptom) •• redness and peeling of the skin of the palms (mechanic's hand) • Dysphagia • Sjögren's syndrome • Raynaud's phenomenon, especially with cross syndromes and with antisynthetase syndrome, including, in addition to Raynaud's syndrome, fever, development of “mechanic's hand” ", interstitial pulmonary fibrosis and rheumatoid-like arthritis • Lung damage: acute diffuse alveolitis, interstitial pulmonary fibrosis • Myocardial damage •• complex rhythm and conduction disturbances up to complete AV block (rare) •• possible development of dilated cardiomyopathy (rare) • Symmetrical polyarthritis without deformations, most often affecting the small joints of the hands; often develops at the onset of the disease • Carpal tunnel syndrome: swelling of the hands, pain and decreased sensitivity in the I-III fingers and the radial side of the IV finger • Calcinosis of the skin (in children) • Kidney damage (rarely): proteinuria, nephrotic syndrome, myoglobinuria with development OPN.
Laboratory data • Increased CPK content, with the exception of the onset of the disease, late stages with severe muscle atrophy and paraneoplastic myositis • Serum aldolase is increased • Increased creatinine concentration (in less than 50% of patients) • Myoglobinuria • Increased ESR - with the development of systemic manifestations • High titers of RF (less than 50% of patients) • Presence of ANAT (more than 50% of patients) • Among the many myositis-specific antibodies, antibodies to tRNA aminoacyl synthetases, namely anti-Jo-1, a marker of antisynthetase syndrome, have diagnostic value. Instrumental data • ECG - arrhythmias, conduction disturbances • Electromyography - increased muscle excitability, action potentials with low amplitude, polyphasic action potentials, fibrillations • Muscle biopsy (deltoid or quadriceps femoris): characteristic inflammatory changes are found in 75% of cases • X-ray changes in the joints not typical (in children, the formation of calcifications in soft tissues is possible) • For radiological diagnosis of interstitial fibrosis of the lungs, chest radiography and (to increase sensitivity) CT are used. Differential diagnosis • Diseases of the rheumatic circle • Neurological pathology accompanied by myopathic syndromes (myasthenia gravis, Lambert-Eaton syndrome, Duchenne, Becker muscular dystrophy • Endocrine pathology (hyperthyroidism, hypoparathyroidism, hyperaldosteronism) • Infectious myositis (viral, bacterial, parasitic) • Drug-induced myopathies ( may be caused by the use of lipid-lowering drugs, colchicine, GC, ethanol, delagil, zidovudine) • Electrolyte disturbances (magnesium, calcium, potassium).
Diagnostic criteria In the presence of at least one type of skin lesion and at least 4 signs, the diagnosis of DM is reliable (sensitivity 94.1%, specificity 90.3%). The presence of at least 4 signs is consistent with the diagnosis of polymyositis (sensitivity 98.9%, specificity 95.2%) • Skin lesions •• Heliotrope rash - red-purple erythematous rash on the eyelids •• Gottron's sign - red-purple scaly atrophic erythema or spots on the extensor surface of the hands over the joints •• Erythema on the extensor surface of the extremities over the elbow and knee joints • Proximal muscle weakness (upper and lower extremities, trunk) • Increased activity of CPK and/or aldolase in the blood serum • Muscle pain on palpation or myalgia • Changes in electromyography (short polyphasic motor unit potentials with spontaneous fibrillation potentials) • Detection of Jo-1 AT (Ab to histidyl-tRNA synthetase) • Non-destructive arthritis or arthralgia • Signs of systemic inflammation (fever more than 37 ° C, increased concentration of CRP or increased ESR more than 20 mm/h) • Histological changes: inflammatory infiltrates in skeletal muscles with degeneration or necrosis of muscle fibrils; active phagocytosis or signs of active regeneration.
TREATMENT General tactics : the basis of treatment is active anti-inflammatory therapy to induce and then maintain remission. Drug treatment • GCs •• Serve as the drug of choice (for example, prednisolone) •• In the acute stage of the disease, the initial dose of prednisolone is 1 mg/kg/day •• If there is no improvement within 4 weeks, the dose should be increased by 0.25 mg/kg/day months to 2 mg/kg/day with an adequate assessment of clinical and laboratory effectiveness •• After achieving clinical and laboratory remission (but not earlier than 4-6 weeks from the start of treatment), the dose of prednisolone is gradually reduced (about 1/4 of the daily dose in every month under clinical and laboratory control, with negative dynamics the dose is increased again) •• The total duration of treatment is approximately 2–3 years •• Pulse therapy is used for juvenile polymyositis or for adult polymyositis/dermatomyositis with progression of dysphagia and systemic manifestations •• If there is no increase in muscle strength after taking prednisolone at a dose of 80 mg/day or more for 4 months, steroid myopathy, inclusion body myositis, and muscle pathology not related to inflammatory myopathies should be excluded. • Immunosuppressive drugs for the purpose of “steroid-sparing” effect •• Methotrexate ••• When taken orally, the initial dose is 7.5 mg/week with an increase of 0.25 mg/week until the effect is obtained (no more than 25 mg/week) ••• When IV administration initial dose of 0.2 mg/kg/week with an increase by 0.2 mg/kg/week (not more than 25 mg/week) until a clinical effect is obtained ••• For this pathology, methotrexate is not administered intramuscularly! ••• The clinical effect of the drug usually develops after 6 weeks, the maximum effect - after 5 months ••• Upon achieving remission, methotrexate is discontinued, gradually reducing the dose (by 1/4 per week) ••• During treatment, general blood and urine tests are necessary , as well as liver function tests ••• Methotrexate is contraindicated in pregnancy, diseases of the liver, kidneys, bone marrow; incompatible with anticoagulants, salicylates and drugs that inhibit hematopoiesis •• Azathioprine (less effective than methotrexate) ••• Dose 2–3 mg/kg/day. The maximum effect usually develops after 6–9 months ••• Then the daily dose is reduced by 0.5 mg/kg every 4–8 weeks to the minimum effective ••• Azathioprine is contraindicated in cases of severe inhibition of hematopoiesis, severe liver diseases, pregnancy ••• Allopurinol increases the toxicity of azathioprine. Azathioprine is incompatible with drugs that cause leuko- or thrombocytopenia •• Cyclosporine may have an effect in GC-resistant forms of dermatomyositis/polymyositis ••• initial dose 2.5–3.5 mg/kg ••• maintenance dose 2–2.5 mg /kg •• Cyclophosphamide is used for the development of interstitial pulmonary fibrosis at 2 mg/kg/day. • Aminoquinoline derivatives (hydroxychloroquine 200 mg/day) allow you to control the skin manifestations of DM. • Immunoglobulin •• Immunoglobulin IV at a dose of 0.4–0.5 g/kg (long-term treatment, high cost). Non-drug therapy • Plasmapheresis, lymphocytopheresis are indicated for patients with manifestations of vasculitis or cross syndromes in combination with severe muscle pathology, resistant to other types of treatment. Complications • Recurrent infections during long-term immunosuppressive therapy • Respiratory failure due to severe muscle weakness, interstitial lung damage • Aspiration pneumonia. Concomitant pathology • Malignant neoplasms (with DM - most often nasopharyngeal localization of neoplasms) • Systemic scleroderma • Vasculitis • SLE. Forecast. Factors aggravating the prognosis: elderly patients, inadequate therapy at the onset of the disease, severe myositis, paraneoplastic myositis, antisynthetase syndrome. Synonyms • Wagner's disease • Wagner–Unferricht–Hepp syndrome. Abbreviations • DM—dermatomyositis.
ICD-10 • M33 Dermatopolymyositis
Possible complications
- Difficulty in swallowing. Damage to the gastric muscles.
- Disease of the respiratory tract, shortness of breath due to damage to the pectoral muscles, which in the worst case can lead to respiratory arrest.
- Aspiration pneumonia. Due to the fact that the swallowing process is disrupted, what is contained in the stomach can enter the respiratory organs when inhaling, which will provoke the appearance of pneumonia.
- Calcium deposits. Calcium can be deposited in the skin, muscle and connective tissues.
- Cardiovascular diseases. Myocarditis, arrhythmia and heart failure.
- Vascular diseases. White skin on the fingers and nose during cold weather indicates Raynaud's syndrome.
- Kidney problem. The appearance of renal failure.
- High probability of oncological pathology.
3. Symptoms, diagnosis
Many causes - many consequences; in other words, the clinical picture of dermatomyositis is very diverse. On the skin side, the most typical changes are the so-called. Gottron's symptom and heliotrope rash: various spots of a reddish or purple hue, plaques on the outer side of the finger phalanges and other joints, rashes in various areas (neck, back, abdomen, etc.), branching purple-bluish spots, in the early stages - changes in the nails cuticle
Another characteristic symptom of DM is progressive muscle weakness in the limbs, fatigue from less and less exercise, and sometimes muscle pain. As the disease progresses, the muscles of the respiratory system and upper gastrointestinal tract may be involved in the process, which leads to difficulties in breathing, swallowing, and speech. At certain stages, contractures (joint blocking), pneumonia and other areas of inflammation may appear.
In addition to skin and muscle disorders (as axial symptoms), the development of DM with varying frequency is accompanied by damage to the digestive, endocrine, genitourinary, cardiovascular, musculoskeletal systems, calcification (calcification) of soft tissues and other severe, even severe disabilities or death - complications.
There are several types of dermatomyositis: idiopathic (this is the case when the disease has to be explained by a combination of purely individual unfavorable characteristics of the body), tumor, juvenile (childhood and adolescence), combined.
The diagnosis of “dermatomyositis” is established mainly clinically (i.e., by direct examination, study of anamnesis, complaints and dynamics), sometimes only after a series of additional consultations with specialized specialists. In some cases, laboratory analysis methods (usually quite complex), biopsy, and electromyography as a way to study muscle status are also informative and indicated.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of the disease
In many cases, immunosuppressants are prescribed. Motor processes should be moderate until the inflammatory process slows down. In the initial stages of treatment, it is recommended to use glucocorticoids. Adults with acute disease are prescribed 50 mg of prednisone orally once a day. Constant monitoring of creatine kinase activity is considered an effective indicator of treatment: in a larger number of patients, after 2-3 months, it is observed to decrease or reach acceptable levels with a further increase in muscle strength.
Immunosuppressants and glucocorticoids are prescribed to treat dermatomyositis.
When the enzyme activity has stabilized, the amount of prednisone used is reduced. If the action of the enzymes increases, the dose is increased again. If complete recovery is achieved, the drug is gradually withdrawn from the patient's regimen under the strictest supervision of his further condition. But in most cases, adult patients require long-term treatment with prednisone. For children, a dose of 40-50 mg per day is intended. Discontinuation of the drug in children is allowed after remission.
There are cases when in patients who have been using a large dosage of glucocorticoid for a long time, weakness increases as a result of the appearance of steroid myopathy.
If there is an inappropriate response to therapy with this drug and if hormonal myopathy or other problems occur, the amount of medication used should be reduced or prednisolone should be discontinued. In this case, it is worth considering treatment with immunosuppressants. Many specialists prescribe combination treatment in the initial stages of therapy. Some patients take methotrexate alone for 5 years or more. Intravenous drug therapy may be beneficial for patients who are refractory to drug treatment. But their considerable price does not make it possible to organize comparative studies. Myositis, similar to a malignant formation, is most often more refractory to corticosteroids. Myositis, similar to a tumor, may subside if it is removed.
Important! Patients with an autoimmune disease are more likely to develop atherosclerosis and should therefore be monitored regularly. Constant and long-term treatment requires patients to prevent osteoporosis.
4.Treatment
Currently, anti-inflammatory hormonal therapy using glucocorticosteroids is considered the most effective therapeutic strategy for the treatment of dermatomyositis. Means of normalizing metabolism (metabolism), stimulating blood circulation and tissue nutrition are also used. In some cases, physical therapy and massage are indicated for the prevention of joint mobility disorders. If there is no effect from these regimens, rheumatology-specific cytostatics are prescribed. Developing complications are treated symptomatically (for example, when muscle deficiency increases, anabolic hormones can be prescribed; in the case of a tumor, appropriate surgical intervention is performed). An important role is played by vitamin complexes.
In most cases, it is possible to achieve high-quality remission or significant improvement.
Necessary patient care
- The sleeping place of a person with dermatomyositis should be comfortable, soft and keep warm. Affected joints should be protected from possible microtraumas.
- If prescribed by a doctor, apply a warm compress to the joints.
- It is necessary to constantly monitor the patient’s medications, remind them of the need to take them, and monitor compliance with the dosage. Monitor possible deviations from the usual state and emerging complications during treatment.
- Monitoring the patient's hygiene. If necessary, provide assistance during changing bed and personal linen, and taking a bath. If there is pain in the joints and muscles, excessive weakness, the patient is unable to perform these simple actions alone.
- The patient's diet should contain essential vitamins, especially vitamins B, C and D, and not contain many fatty acids. It is worth reducing the use of table salt. Food should be sufficiently high in calories and well digestible by the stomach, the diet should be balanced.
- Regular performance of therapeutic exercises. Physical exercises should be aimed at working with affected muscles and joints, individual muscle groups. If dermatomyositis is detected, it is worth performing special gymnastic exercises for the facial muscles. During exercise, active and passive loads occur on all joints. Treatment procedures should occur at a time of low activity of immunoinflammatory processes with full monitoring of the patient’s condition.
- Taking into account the fact that treatment requires a lot of time, there is a possibility of various complications arising from the medications used (especially when using cytostatics and glucocorticosteroids). It is worth paying special attention to constant conversations with the patient, during which it is worth conveying the necessary meaning of the therapy being carried out, convincing the patient to show more tolerance and restraint, directing him to positive thoughts and charging him with good emotions. It is equally important to talk to the patient's family. It is worth bringing them up to date and highlighting the essence and nuances of the disease, the established course of treatment, familiarizing them with possible complications and convincing them to be tolerant when providing the patient with the necessary help and support.
- It is worth helping the patient with the optimal organization of his day, thinking about his working hours and rest periods. It is better to refuse night work, minimize physical activity and protect from emotional outbursts.
Patients with dermatomyositis require constant care and monitoring.
Treatment of amyopathic dermatomyositis
Treatment of amyopathic dermatomyositis is aimed at controlling skin manifestations. The first line of therapy includes protection from sun exposure (use of sunscreens), as well as the use of topical steroids and antihistamines aimed at reducing erythema and itching. If treatment fails, oral corticosteroids and antihistamines are prescribed.
If there is no positive effect, the patient may be prescribed injections of corticosteroids, antimalarial (hydroxychloroquine) or cytostatic (methotrexate) drugs, immunosuppressants (mycophenolate), and intravenous immunoglobulin.
Patients diagnosed with amyopathic dermatomyositis require constant medical supervision and health monitoring to promptly identify signs of muscle tissue inflammation.
Features and advantages of treatment of amyopathic dermatomyositis at the Rassvet clinic
The Rassvet clinic employs a multidisciplinary team of highly qualified specialists in all areas. All our doctors are well trained and have extensive practical experience necessary to diagnose and treat not only typical diseases, but also rare diseases and syndromes.
Patients with suspected amyopathic dermatomyositis undergo all necessary studies, are prescribed therapy aimed at reducing the symptoms of the disease and improving the patient’s quality of life, and provide maximum support at all stages of treatment.
Author:
Amelicheva Alena Aleksandrovna medical editor
Prevention and prognosis of dermatomyositis
In severe and advanced forms of the disease, the risk of death in the first couple of years of development of the pathology is close to 30-40% of all cases, especially as a result of respiratory tract disease and gastric hemorrhage. Despite the severity of the disease, contractures appear and limbs are gradually lost, which later ends with the patient becoming disabled. Timely provision of assistance and establishment of a therapeutic course will help prevent the development of the disease and improve the further prognosis.
If the patient received timely assistance, complications will not arise
No special preventive recommendations for the treatment of pathology have been developed.
Diet for dermatomyositis
Vitamin-protein diet
- Efficiency: 5 kg in 7-10 days
- Terms: up to 14 days
- Cost of products: 1700-1800 rubles. in Week
Since the pathology can affect the muscles of the pharynx and cause dysphagia, patients are recommended to eat pureed and liquid food. The diet should contain:
- fresh juices;
- vegetable cream soups and purees;
- light dietary protein in sufficient quantities.
Moreover, it is important to maintain normal proportions of BJU and use natural products, as well as healthy methods of processing them.
Let's sum it up
Dermatomyositis is an extremely unpleasant disease, which is not very easy to get rid of. However, the sooner the patient seeks help and begins therapy, the easier this disease will pass for him and the faster he will be able to live life to the fullest again.
Unfortunately, it is difficult to prevent such a pathology, since the exact cause of the development of the disease has not yet been discovered. However, if a person leads a healthy lifestyle, the risk of developing such a disease will be minimized.
Causes
The pathology is polyetiological, it is preceded by many factors:
- latent infectious agents: influenza viruses , parainfluenza , hepatitis B , picornaviruses , parvovirus infection , bacteriological pathogens of Lyme disease and group A beta-hemolytic streptococci , protozoa, for example, toxoplasma ;
- malignant neoplasms;
- vaccination against typhoid, measles, mumps, cholera, rubella ;
- therapy with D-penicillamine , growth hormones .
Etiology of dermatomyositis
The etiology of dermatomyositis is associated with viruses, genetic disorders, and pathology of the immune system. The possibility of the occurrence of dermatomyositis due to excessive sun exposure, exposure to low temperatures, etc. is also not excluded. Of the viral agents, there is a high probability of involvement of the virus group, parainfluenza, hepatitis viruses, etc. Borrelia, streptococci are putative bacterial pathogens. The theory of genetic predisposition is not rejected.
In any case, the above factors lead to the formation of antibodies in the blood that attack muscle fibers. The following factors contribute to the transition to the active form of the disease:
- Stressful situations;
- Infectious diseases;
- Hypothermia;
- Medication load, etc.