Vaginal mycosis is one of the most common intimate infections in women. Candida albicans infection, also called thrush or candidiasis, is a common result of antibiotic treatment and a complication of pregnancy, hormone therapy, and diabetes. It causes a number of unpleasant symptoms, and over time begins to cause pain and contribute to serious complications. Below is information about the possible causes and consequences of vaginal mycosis, as well as methods of treating and preventing the development of infection.
What is vaginal candidiasis? Causes of the disease
Vaginal candidiasis is an inflammatory disease of the genitourinary tract caused by yeast-like fungi of the genus Candida.
In most cases, the cause of vaginal candidiasis is Candida Albicans. It can reproduce successfully in an oxygen-free environment and grows especially well on tissues that contain large amounts of glycogen, including the mucous membrane of the female genitalia. Recently, doctors are increasingly discovering other pathogens of the Candida genus, but the overall frequency of their occurrence does not exceed 15-30%.
Internal risk factors for the development of vaginal candidiasis include endocrine diseases (diabetes mellitus, obesity, thyroid pathology, etc.), underlying gynecological diseases, disorders of local immunity; to external risk factors - taking antibacterial, glucocorticosteroid, cytostatic drugs, immunosuppressants, radiation therapy; wearing tight clothing, underwear made of synthetic fabrics, regular use of sanitary pads, prolonged use of intrauterine devices, vaginal diaphragms, douching, use of spermicides.
Symptoms of vaginal candidiasis
Classic signs of vaginal candidiasis are:
- itching and burning in the vagina and in the external genital area;
- specific discharge resembling cottage cheese;
- pain and burning when urinating;
- discomfort and pain during sexual intercourse.
As a rule, discomfort intensifies in the afternoon, and in some women before menstruation. During a gynecological examination, the doctor detects swelling and redness of the mucous membrane of the genital tract, as well as specific white or yellowish-white cheesy thick vaginal discharge.
With a complicated course of the disease, cracks appear on the skin of the vulva and mucous membranes, posterior commissure and peranal area; with recurrent candidal vulvovaginitis, dryness, atrophy, lichenification in the affected area, and scanty whitish vaginal discharge are expressed.
Make an appointment
Contraindications
There are several contraindications for the disease, and most of them relate to restrictions on the use of certain foods. In case of vulvovaginitis, it is strictly prohibited:
- consumption of alcoholic beverages, fatty, salty, spicy, smoked and sweet foods, foods with any food additives;
- Fast food, semi-finished products, instant food are prohibited;
- If you have an allergic predisposition, you should exclude foods that provoke allergy attacks.
Classification
There are several types of classification of vaginal candidiasis. Depending on the characteristics of the course, acute and chronic (recurrent) forms of the disease are distinguished. In the first case, the pathology is characterized by vivid symptoms and occurs no more than four times a year. With chronicity, the symptoms are usually less pronounced, and the disease itself recurs 4 times a year or more often.
Depending on the presence of complications, uncomplicated and complicated vaginal candidiasis is distinguished. In the first case, the process is relatively easy and can be stopped quite quickly with the selection of adequate therapy. As a rule, it occurs in women who do not have additional risk factors (diabetes mellitus, immunodeficiency states of various origins).
The complicated form of vaginal candidiasis is characterized by pronounced symptoms that negatively affect the patient’s daily life. As a rule, inflammation spreads to the external genitalia, causing the appearance of ulcers and cracks. This form often recurs.
Localization of the pathological process allows us to distinguish three forms of the disease:
- vaginitis: inflammation affects only the vaginal mucosa;
- vulvovaginitis: the external genitalia and vagina are affected;
- cervicitis: the cervix is involved in the process.
Indications for the disease
A number of doctor's indications for this disease will help alleviate symptoms and recover faster.
If you have vulvovaginitis in childhood, you should not ignore the testimony of specialists. They relate to general health measures, elimination of foci of chronic infection, and personal hygiene.
In older women, vulvovaginitis develops against the background of physiological changes in the vaginal mucosa. To relieve the symptoms of vulvovaginitis, they are shown sitz baths and douching with herbal decoctions, antiseptic solutions, and the use of vaginal suppositories. Treatment of underlying pathological conditions is required to reduce allergic mood, correct glycemic levels in diabetes mellitus, sanitize infectious foci, etc.
If specific vulvovaginitis is detected, treatment of the sexual partner is required. Sexual rest is required until the end of treatment.
Correction of nutrition, normalization of weight, and changes in hygiene habits are also important. In certain cases, the elimination of provoking factors leads to a permanent cure of vulvovaginitis without subsequent relapses. To monitor the situation after a course of therapy, a control bacterioscopic and microbiological analysis of discharge from the genital tract is performed.
Complications
Most complications of vaginal candidiasis are associated with the spread of the inflammatory process to nearby organs and tissues and the addition of bacterial inflammation. It occurs against the background of a sharp decrease in local immunity. Most often, patients encounter the following problems:
- salpingitis and salpingo-oophoritis (adnexitis): inflammation of the uterine appendages: tubes and ovaries; the process can be unilateral or bilateral, accompanied by pain in the lower abdomen, weakness, fever; without treatment, it can cause infertility due to the development of adhesions;
- urethritis: inflammation of the urethra; classic symptoms are a burning sensation when urinating, changes in the appearance and color of urine, redness and swelling in the area of the external urethral meatus;
- cystitis: inflammation of the bladder that develops as a result of the passage of the pathogen from the urethra; Symptoms of urethritis include frequent urination with a small amount of urine, pain and cramping at the end of the process, increased temperature and pain in the lower abdomen.
In addition to the spread of infection, vaginal candidiasis can threaten the development of stenosis (narrowing) of the vagina. This condition occurs due to chronic inflammation, which leads to the growth of scar tissue and narrowing of the lumen of the organ. This leads to significant difficulty in sexual life.
Vaginal candidiasis is very dangerous for pregnant women, since without treatment, infection of the fetus is possible, which can lead to its death.
In the postpartum period, women may develop candidal endometritis.
Diagnostics
Diagnosis of vaginal candidiasis begins with collecting complaints. The gynecologist clarifies what worries the patient, when and under what circumstances specific problems appeared, as well as what measures were taken to eliminate them and with what effect. Attention is paid to the medical history: previous diseases (inflammation of the urogenital tract, STDs are especially important), the number of pregnancies and births, the number of sexual partners, etc.
The next diagnostic stage is an examination in a gynecological chair, during which the doctor identifies characteristic changes: swelling, redness, discharge and plaque. When Lugol's solution is applied to tissues, white dots resembling semolina are visualized on them, which is a characteristic sign of the disease. To confirm the diagnosis, the doctor prescribes:
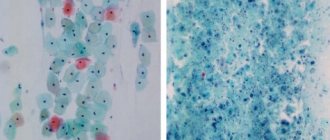
- microscopy of vaginal smears (during the process, spores and fungal cells are identified);
- culture of vaginal discharge;
- PCR and ELISA of the excreted to detect pathogen antigens;
- blood test: general (signs of an inflammatory process are detected), tests to detect antibodies to Candida - remove!
If necessary (for example, during a recurrent course of the disease), tests are carried out to identify risk factors: elevated blood glucose levels, immunodeficiency, etc.
Treatment of vaginal candidiasis
Specific treatment aimed at eliminating vaginal candidiasis is carried out only after identifying the pathogen and if the patient has signs of the disease. The basis of therapy is specific antifungal agents: nystatin, clotrimazole, ketoconazole, fluconazole, nitrofungin and others. The specific drug, its dose, frequency of administration and course duration are selected individually depending on the characteristics of the course of the disease, the presence of concomitant pathologies and other factors.
If we are talking about an acute uncomplicated process, the drugs are prescribed in local form in the form of suppositories, vaginal tablets or creams. They are introduced directly into the genital tract, where they stop the active reproduction of the pathogen.
In the presence of complications, as well as in the chronic course of the disease, systemic drugs are used in the form of tablets for oral administration. The application regimen is selected on an individual basis.
Until the manifestations of vaginal candidiasis are completely eliminated, it is necessary to maintain sexual rest in order to minimize injury to the inflamed walls of the genital tract. In chronic cases, condoms must be used. The effectiveness of therapy is assessed 14 days after the start of treatment.
Make an appointment
Cost of initial appointment
The cost of treatment for vulvovaginitis at JSC Meditsina (Moscow) is presented in the table below. Please note that prices are listed by category to make it easier to find the service you need. The price of the primary appointment differs from the secondary one. From the table below, you will learn about prices for consultations, examinations, and medical procedures for both adults and children. If you have any questions, you can call our help desk and find out the prices for treatment or the cost of the examinations you need.
Prognosis and prevention
To completely cure vaginal candidiasis, it is necessary to both consult a doctor in a timely manner and follow all his recommendations. Antifungal drugs are sold in pharmacies without a prescription, but DIY in this case is not only ineffective, but also dangerous. Only a specialist can correctly select the necessary medications, determine the characteristics of their use, and also monitor the effect of the medications.
It is important to understand that it is much easier to prevent vaginal candidiasis than to treat it. To minimize the risk of developing the disease, you must adhere to the following rules:
- give preference to cotton underwear;
- stop using panty liners;
- use specialized products for genital hygiene;
- do not use douching without a doctor’s prescription;
- monitor the condition of the body, promptly treat pathologies of the genitourinary and digestive systems, endocrine glands;
- avoid casual sex and infection with sexually transmitted diseases;
- do not use antibiotics without a doctor’s prescription and do not change the dose and regimen without permission;
- if long-term antibiotic therapy is necessary, take antifungal agents.
Vaginal candidiasis is an unpleasant disease that can be prevented and, if necessary, quickly cured. The main thing is to consult a doctor in a timely manner and follow all his recommendations.
Advantages of treatment at the clinic of JSC "Medicine"
JSC "Medicine" is a modern multidisciplinary medical institution that provides a full range of medical services in accordance with the highest international standards. We offer emergency medical care, service in a clinic, a comfortable hospital, high-precision laboratory and instrumental diagnostics, and an ultra-modern Sofia Oncology Center.
The clinic of JSC "Medicine" uses the latest achievements in global healthcare. Among our advantages are the following:
- We are pleased to offer our patients a full range of medical services. We employ more than 300 specialists from 67 medical specialties. Our clinic provides a full range of medical services in various medical areas. There are 69 of them in total.
- We operate on the principle of continuity of stages of medical care: a physician-supervisor treats a patient as a family doctor, internist or pediatrician, coordinates treatment prescribed by specialists, and also participates in the treatment of his patients in a hospital.
- We work according to the best Russian and international standards. JSC "Medicine" is the first Russian medical center that is accredited according to the most reliable international standards for the quality of medical care, Joint Commission International.
- We provide guarantees of the quality of medical care. The Medicine Clinic is responsible for the quality of the services provided. If the complaint is justified, compensation may be paid.
- The best specialists work with us. We are proud of our doctors. Patients are advised by academicians of the Russian Academy of Sciences, professors, and famous foreign specialists. JSC Meditsina has developed a system for training doctors and exchanging experience with the most prestigious clinics in the world. Many areas of the clinic, including the sleep laboratory, traumatology and orthopedics center, chemotherapy and radiation therapy departments, were created in collaboration with foreign colleagues.
- JSC "Medicine" is a multidisciplinary university clinic. At our clinical and educational laboratory bases, scientific and clinical developments are carried out in many medical areas. We are advised by academicians and corresponding members of the Russian Academy of Sciences, professors and leading experts in various fields of medicine. The educational and laboratory base of the department is located in the building of the Medicine clinic.
- Exchange of experience with the best medical centers in the world, accredited by JCI, advanced training of doctors and partnerships with leading medical institutions in the USA, Europe and Israel put the Medicina clinic in a leading position. You can learn about our doctors, their work experience, education and experience on the resource of our medical center.
- We use an advanced IT infrastructure, using an electronic medical record (EHR) of our own design with a system for checking drug prescriptions. We have implemented digital archive solutions that allow storing the results of medical research obtained from various medical equipment (computer tomograph, MRI, X-ray machines, ultrasound equipment, endoscopic equipment). JSC Meditsina implemented a smart clinic project, which took into account high requirements for reliability, safety and fault tolerance.
For the convenience of our patients and their relatives, we have created a convenient client-oriented service. Making an appointment with a doctor and viewing your medical data is possible through a mobile application, a personal account on the website, or a Telegram bot. Test results come to hand on disk if you need to get a “second opinion” from specialists at other clinics. With the consent of hospital patients, their relatives can receive SMS notifications about the stages of surgical intervention and observe the hospital and ward online, making sure of the unsurpassed quality of the treatment methods provided in our clinic.
Bibliography
- Gynecology textbook. IV edition ed. Academician of the Russian Academy of Medical Sciences, Professor G.M. Savelyeva; prof. V.G. Breusenko 2012
- Urogenital candidiasis. Clinical recommendations. Moscow, 2016 – 22 p.
- Vulvovaginal candidiasis: pathogenesis, diagnosis and treatment tactics. Bayramova G.R., Amirkhanyan A.S., Chernova V.F. //Doctor.Ru 2018. No. 10 (154). pp. 32-36
- Sherry L., Kean R., McKloud E., O'Donnell LE, Metcalfe R., Jones BL et al. Biofilms formed by isolates from recurrent vulvovaginal candidiasis patients are heterogeneous and insensitive to fluconazole. Antimicrob. Agents. Chemother. 2017; 61(9): e01065-17
- Prilepskaya V.N. Vulvovaginal candidiasis. Clinic, diagnosis, principles of therapy: manual / V.N. Prilepskaya, G.R. Bayramova - M 2008 - 50s
- Atlas of pathogens of fungal infections/E.N. Moskvitina and others - Moscow GEOTAR-Media, 2022 208p
- Zordan R., Cormack B. Adgesis on opportunistic fungal pathogens In: Calderone RA, Clancy CJ, ed Candada and candidiasis/ Washington: ASM press; 2012: 243-259)
- Zhang Y., Li W., Chu M., Chen H., Yu H., Fang C. et al. The AAA AT Pase Vps4 plays important roles in Candida albicans hyphal formation and is inhibited by DBeQ. Mycopathology 2016; (5-6) 329-39
- Murciano C., Moyes DL, Runglall M., Yobouti P., Islam A., Hoyer LL et al. Evaluation of the role of Candida albicans agglutinin-like sequence (Als) proteins in human oral epithelial cell interactions. Plos one 2012.
- Center for Disease Control (CDC) Sexually Transmitted Disease Treatment Guidelines, 2015.
- Donders GG, Bellen G., Mendling W. Management of recurrent vulvovaginal candidosis as a chronic illness. Gynecol. Obstet. Invest 2010 70(4):306-21
- Ankirskaya A.S. Muravyova V.V. Microbiological characteristics of vaginal infections caused by fungi of the genus Candida // sexually transmitted diseases 2001. pp. 12-14
- Eschenbach DA Chronic vulvovaginal candidosis N Engl. J Med 2004; 351(9)
- Tikhomirov A.L. Oleinik Ch.G. Optimization of treatment of recurrent vulvovaginal candidiasis // effective therapy in obstetrics and gynecology. 2007 No. 3 from 22-27
- Bayramova G.R. Recurrent vaginal candidiasis. Clinic, diagnosis, treatment. dis. Doctor of Medical Sciences M. 2013 (46s)
- Prilepskaya V.N. Bayramova G.R. Vulvovaginal candidiasis, modern ways to solve the problem. Difficult patient 2006 (from 33-36)
Vulvovaginal candidiasis: pathogenesis, clinical picture, diagnosis, modern principles of therapy
Vulvovaginal candidiasis is an infection of the vulvar and vaginal mucosa caused by yeast-like fungi of the genus Candida. As a rule, it affects women of reproductive age; it is less common in girls and women in the peri- and postmenopausal period.
In recent years, the prevalence of vulvovaginal candidiasis has been steadily increasing; the share of this disease in the structure of infectious lesions of the vulva and vagina is 30 - 45%. Currently, vulvovaginal candidiasis ranks second among all vaginal infections and is one of the most common reasons for women seeking medical help. In the United States, 13 million cases of this disease are recorded annually. During pregnancy, the prevalence of this infection reaches 40 - 46% (Horowitz BJ, 1991), it is one of the reasons for the development of pregnancy complications (the number of spontaneous miscarriages in early pregnancy, the threat of miscarriage increases by 1.5 times, the risk of infection of the fetus and newborn - 2.4 times). Vulvovaginal candidiasis is found in 30% of cancer patients and in 64% of patients with various endocrine disorders. According to JS Bingham (1999), 75% of women of reproductive age have at least one episode of vulvovaginal candidiasis during their lifetime, and 50% have a repeated episode. 5% of women on the planet suffer from recurrent vulvovaginal candidiasis.
The causative agent of vulvovaginal candidiasis is yeast-like fungi of the genus Candida. Fungi of the genus Candida are opportunistic microorganisms that live as saprophytes on the skin and mucous membranes of healthy people.
Currently, more than 170 biological species of yeast-like fungi have been described, among which in the vast majority of cases (85 - 90%) the causative agent is C. albicans (Sobel JD, 1998). Among other Candida species, C. glabrata (according to the old classification - C. torulopsis), C. tropicalis, C. parapsilosis, C. krusei, C. guilliermondi are of clinical importance, much less often - C. pseudotropicalis and Saccharomyces cerevisiae.
A significant increase in cases of vulvovaginal candidiasis is due to a number of predisposing factors.
When prescribing broad-spectrum antibiotics, it is necessary to take into account that they suppress not only pathogenic bacteria, but also lactobacilli located in the vagina, which are physiological antagonists of yeast-like fungi (lactobacillus suppresses the attachment of Candida to epithelial cells and their reproduction). As a result, the pH of the vaginal contents increases (shifts to the alkaline side), and the process of self-cleaning of the vagina is disrupted. Additionally, Candida has the ability to use antibiotics as food sources. This creates favorable conditions for the active reproduction of Candida in the woman’s genitals.
The facts of the development of vulvovaginal candidiasis during pregnancy are also well known. The first episode of vulvovaginal candidiasis occurs in many women during pregnancy. The frequency of vulvovaginal candidiasis in pregnant women reaches 40 - 46% (Horowitz BJ, 1991). Such high rates are due to changes in hormonal balance during pregnancy. The highest degree of colonization is observed in the last trimester and in first-time mothers.
Vulvovaginal candidiasis is one of the diseases of modern civilization. The development of vulvovaginal candidiasis is facilitated by wearing underwear made of synthetic fabrics that tightly fits the body, resulting in a microclimate with high humidity and temperature, which leads to maceration of the stratum corneum of the skin, the emergence of thermostatic conditions for the development of local microflora, including intestinal, where among fungi C. albicans accounts for over 95% (Antonyev A. A., 1985). The virulence of C. albicans increases under conditions of high humidity (sweating). Therefore, wearing tight synthetic underwear, washing with a pressure shower, using sprays, or using pads is a trigger for the development of a hypersensitivity reaction and predisposes to Candida colonization.
Fungi of the genus Candida can be isolated from the vagina of practically healthy women in the absence of clinical signs of vulvovaginal candidiasis (carriage). Under certain conditions, under the influence of exogenous and/or endogenous factors, these fungi become pathogenic, causing disease.
Despite the existence of numerous studies, the modes of infection and the route of transmission of the pathogen in vulvovaginal candidiasis remain the subject of debate. Yeast-like fungi enter the woman’s genital tract from the intestines, upon contact with exogenous sources of infection, through household objects. There is evidence that in recurrent vulvovaginal candidiasis, the gastrointestinal tract serves as a permanent reservoir of fungi and a source of reinfection of the vagina. In cases where fungi are sown from the vagina, they are almost always found in feces, and in most women both vaginal and intestinal strains are identical.
Typically, candidiasis occurs endogenously, as a consequence of dysmetabolic disorders and dysfunction of the immune system. Sexual transmission is also possible, although this point of view is still controversial (despite the fact that partners may be carriers of the same strain of the pathogen).
The pathogenesis of vulvovaginal candidiasis is complex and not well understood. Considering the fact that C. albicans strains isolated from patients with vulvovaginal candidiasis and from carriers do not differ significantly in a number of biochemical characteristics, we can conclude that the state of the macroorganism plays a leading role in the development of vulvovaginal candidiasis, and not the properties of the pathogen. The trigger for the development of the disease is not a change in the properties of the fungus, but a decrease in the resistance of the host organism.
The following stages are distinguished in the development of candidal infection:
- adhesion of fungi to the surface of the mucous membrane;
- colonization of the mucous membrane by fungi;
- invasion into the epithelium, overcoming the epithelial barrier of the mucous membrane, entering the connective tissue of the lamina propria, overcoming tissue and cellular protective mechanisms;
- penetration into blood vessels and hematogenous dissemination with damage to various organs and systems.
This sequence reflects all stages of the development of severe candidiasis, however, in milder cases, the infection may stabilize at one of these stages.
With vulvovaginal candidiasis, the infectious process often affects only the superficial layers of the vaginal epithelium. Due to the dynamic balance existing at this level between microorganisms (fungi), which strive but cannot penetrate the deeper layers of the mucous membrane, and the macroorganism, which tries, but is not able to completely eliminate the pathogen, the infection can persist for decades. And loss of balance can lead either to an exacerbation of the disease, or, conversely, to remission or recovery.
Currently, there are three clinical forms of vulvovaginal candidiasis:
- candidiasis;
- acute form of vulvovaginal candidiasis;
- chronic (recurrent) vulvovaginal candidiasis.
Candidiasis is characterized by the absence of symptoms of the disease. However, during microbiological examination in vaginal discharge, yeast-like fungi of the genus Candida are present in small quantities (<104 CFU/ml). Asymptomatic carriage of Candida is observed in 15 - 20% of non-pregnant women of reproductive age.
The acute form of vulvovaginal candidiasis is characterized by a pronounced clinical picture: hyperemia, swelling, abundant or moderate curdled discharge from the genital tract, rashes in the form of vesicles on the skin and mucous membranes of the vulva and vagina. During microbiological examination in vaginal discharge, yeast-like fungi of the genus Candida are present in high titer (<104 CFU/ml). The duration of the disease with the acute form of candidiasis does not exceed 2 months.
Chronic vulvovaginal candidiasis is characterized by a disease duration of more than 2 months. And on the skin and mucous membranes of the vulva and vagina, secondary elements predominate in the form of infiltration, lichenification and tissue atrophy.
After completion of the course of treatment, despite negative culture results, eradication of the microorganism may be incomplete. This can lead to relapses, and the same strain usually plays an etiological role in their development. Recurrent vulvovaginal candidiasis is diagnosed if four or more mycologically proven exacerbations of the disease occur within 12 months. Develops in approximately 5% of patients with vulvovaginal candidiasis. Moreover, in 50% of women with recurrent vulvovaginal candidiasis, symptoms of the disease appear in the range from several days to 3 months after successful treatment of the acute form.
Clinical manifestations of candidiasis are varied and depend on the nature of previous diseases, the stage of the pathological process, accompanying microbial flora, etc. The following clinical symptoms are characteristic of genital candidiasis: copious or moderate curdled vaginal discharge, itching and burning in the external genital area, increased itching in the afternoon, during sleep, after water procedures, sexual intercourse, long walking, during menstruation, an unpleasant odor that increases after sexual intercourse.
There are situations when invasion of parenchymal organs by pseudohyphae occurs with the development of microabscesses in them. In this case, disseminated or generalized candidiasis occurs, which is characterized by a torpid course and is characterized by a pronounced reaction from all body systems involved in the process.
Diagnosis of vulvovaginal candidiasis should be comprehensive.
The leading role in the diagnosis of vulvovaginal candidiasis, along with clinical symptoms, belongs to microbiological research methods (microscopy of smears of vaginal discharge and cultural method of examination), the diagnostic value of which reaches 95% (Ankirskaya A. S., 1995).
Microscopic examination is one of the most accessible and simple diagnostic methods. The study is carried out in native and Gram-stained preparations.
The cultural method - sowing material on a nutrient medium - allows you to determine the number, genus and species of fungi, their sensitivity to antifungal drugs, as well as identify the nature and degree of microbial contamination with other opportunistic bacteria.
In recent years, express diagnostic methods have been used, which in the shortest possible time with fairly high accuracy make it possible to identify fungal strains using ready-made test systems with favorable environments for fungal growth. The use of express diagnostics is very promising, it does not take much time and is easy to use, but the test results do not allow us to judge the presence of accompanying flora.
In severe, recurrent forms of vulvovaginal candidiasis, accompanied by disorders in the immune system, it is possible to determine the titers of antibodies to fungi of the genus Candida in the blood serum. But this research method is practically not used due to the high frequency of false negative and false positive results.
The colposcopic diagnostic method is not specific. It reveals changes in the epithelium characteristic of the inflammatory process, but does not allow determining the etiology of the disease.
Depending on the concentration of yeast-like fungi of the genus Candida and the nature of the accompanying microflora in the vaginal biotope, three forms of Candida infection of the vagina are distinguished:
- asymptomatic carriage;
- true candidiasis (a high concentration of fungi is combined with a high concentration of lactobacilli);
- a combined form of bacterial vaginosis with candidal vulvovaginitis (fungi grow with an overwhelming predominance of obligate anaerobes).
Such nosological differentiation is appropriate from the point of view of choosing rational etiotropic therapy.
Despite the rapid development of the pharmacological industry and a huge selection of antimycotic drugs, the problem of treating vulvovaginal candidiasis does not lose its relevance. Considering the high frequency of the disease, long course, as well as frequent recurrence of the process, it can be assumed that, most likely, we are talking about an unjustified approach to the diagnosis and treatment of this disease. Thus, the need to develop new treatment regimens for vulvovaginal candidiasis using already known antimycotic drugs with an adequate spectrum of action, with simultaneous action directly on the pathogen and on all possible systemic reservoirs of yeast-like fungi, is an important task to exclude possible relapses.
Therapy for vulvovaginal candidiasis depends on the clinical form of the disease.
The main goal of treatment for vulvovaginal candidiasis is primarily eradication of the pathogen.
In accordance with the classification of L. S. Strachunsky (1994), the following main antifungal drugs are currently used for the treatment of vulvovaginal candidiasis:
- polyene series: natamycin, nystatin, levorin, amphotericin B;
- imidazole series: ketoconazole, omoconazole (Micogal), clotrimazole, miconazole (Ginezol-7), bifonazole;
- triazole series: fluconazole (flucostat), itraconazole;
- others: griseofulvin, flucyzine, nitrofungin, decamine, iodine preparations, etc.
Usually, the diagnosis of vulvovaginal candidiasis is established quite easily, and for the most part, patients are cured thanks to the local use of antifungal drugs. But traditional intravaginal treatment often turns out to be irregular and is associated with side effects such as irritation and a burning sensation in the vagina, and frequent urination. These factors are responsible for poor treatment adherence. Women often stop treatment immediately after the symptoms of the disease disappear, while eradication of the pathogen does not occur. At the same time, it must be taken into account that during the development of clinical manifestations of vulvovaginal candidiasis, the rates of intestinal candida colonization are significantly higher. Non-absorbable oral antimycotics can be used to eradicate the intestinal reservoir.
A general recommendation for the treatment of complicated forms of vulvovaginal candidiasis is to lengthen the therapeutic regimen (when using local forms, the duration of treatment doubles; when using drugs for systemic exposure, it is recommended to re-take the same dose every other week for a single dose, etc.).
Thus, to reduce the likelihood of relapses, the doctor must always take a systematic approach to diagnosing and treating the disease, simultaneously targeting both the pathogen and all possible reservoirs of yeast-like fungi.
Considering that pregnancy is the main predisposing factor in the development of vulvovaginal candidiasis, its treatment for this condition is a particular problem. The main requirement in this situation is the safety of treatment. According to various authors, during pregnancy the need for longer courses of treatment has not been established. Preference should be given to local treatment.
Of the entire arsenal of antimycotics that exist today, drugs belonging to a new class of triazole compounds and containing fluconazole, for example mycomax, have found widespread use in the treatment of vulvovaginal candidiasis.
Fluconazole (Flucostat) 150 mg is highly active against Candida albicans and only about 3 - 5% of Candida albicans strains are resistant to fluconazole or have intermediate sensitivity. Candida krusei and certain strains of Candida glabrata are resistant to fluconazole. Saccharomyces cerevisiae may also be resistant to fluconazole.
Fluconazole inhibits the synthesis of sterols (an important component of the fungal cell wall), has a highly specific effect on fungal enzymes dependent on cytochrome P450, as a result of which fungal growth is inhibited. After oral administration, fluconazole is well absorbed, with plasma levels (and relative bioavailability) exceeding 90% of plasma levels when administered intravenously. Plasma concentrations reach a peak 0.5–1.5 hours after administration on an empty stomach, and the half-life of fluconazole is approximately 30 hours. Plasma concentrations are directly proportional to dose. The maximum concentration of fluconazole 2 hours after oral administration of 150 mg is 2.44–3.8 mg/l. The drug dissolves well in water. Unlike other antifungal drugs of the azole group, fluconazole is characterized by a low degree of binding to plasma proteins (about 11%), so its main amount is in free form. Fluconazole penetrates well into all biological fluids of the body, into the tissues of the reproductive system in an amount comparable to its content in blood serum. The drug also quickly penetrates from the blood into the tissues. Its concentration in blood plasma and tissues of the reproductive system, even 50 hours after administration, exceeds the minimum inhibitory concentration (MIC) for pathogenic yeast fungi. Thus, fluconazole enters the tissues of the female reproductive system in an amount sufficient to treat not only systemic fungal infections, but also vulvovaginal candidiasis. Fluconazole is excreted mainly by the kidneys. Approximately 80% of the administered dose is excreted unchanged in the urine. Fluconazole clearance is proportional to creatinine clearance. Unlike other antimycotic drugs, fluconazole selectively acts on the fungal cell, does not affect the metabolism of hormones, and does not change the concentration of steroids in the blood of women. No fluconazole metabolites were detected in peripheral blood. The long plasma half-life (30 hours) makes it possible to practice a single dose of the drug for vaginal candidiasis. After a single oral dose of 150 mg, a therapeutic concentration is created in the vaginal secretion, which persists for a long time, allowing a therapeutic effect to be obtained for vulvovaginal candidiasis.
It should be noted that the effectiveness of treatment of vulvovaginal candidiasis increases by approximately 10 - 12% after double use of fluconazole (one dose of 150 mg 1 time every 5 - 6 days) compared to a single dose (efficacy reaches 94 - 95%).
Fluconazole has a good preventive effect against recurrent candidiasis. The drug is well tolerated. A possible complication is mild, quickly passing gastrointestinal discomfort (less than 2%), headache and skin rashes are even less common.
The use of fluconazole in pregnant and lactating women for the treatment of vulvovaginal candidiasis is inappropriate, since the possible risk to the fetus exceeds the indications.
Among the polyene antibiotics used to treat vulvovaginal candidiasis, the drug pimafucin is well known - a fungicidal polyene antibiotic from the group of broad-spectrum macrolides for topical and oral use, containing natamycin as an active substance.
Pimafucin is available in various dosage forms: enteric tablets 100 mg, vaginal suppositories 100 mg, 2% cream.
Most pathogenic yeast-like fungi, especially C. albicans, are sensitive to natamycin.
Natamycin binds sterols of cell membranes, disrupting their integrity and function, which leads to the death of microorganisms. The drug is practically not absorbed from the gastrointestinal tract. It is non-toxic and does not have an allergenic effect. Natamycin tablets, due to their enteric coating, act only in the intestines. There are no cases of resistance to natamycin in clinical practice.
Pimafucin does not have a teratogenic effect (when prescribed to pregnant women at a dose of 100 mg per day), and therefore its use during pregnancy (even in the first trimester) and lactation is justified.
Another drug from the imidazole group used in the treatment of vulvovaginal candidiasis is gyno-travogen, a topical drug containing isoconazole nitrate (600 mg). The drug has a fungistatic effect on yeast-like fungi. The drug is also active against gram-positive microorganisms (staphylococci, streptococci), and therefore it can be used for vaginal infections of fungal and mixed origin. Gyno-travogen is produced in the form of vaginal suppositories.
For the treatment of candidal vulvovaginitis or vulvovaginitis of mixed origin in both non-pregnant and pregnant and lactating women, we can recommend a combination drug for topical use with low systemic absorption - terzhinan. The composition of this drug includes: ternidazole - an imidazole derivative, acts on the anaerobic component of the vaginal microflora; neomycin sulfate is a broad-spectrum antibiotic from the group of aminoglycosides, the action of which is aimed at gram-positive and gram-negative bacteria; nystatin is an antifungal antibiotic from the polyene group, highly active against fungi of the genus Candida; prednisolone is a glucocorticoid that has a pronounced anti-inflammatory effect (allows you to quickly stop signs of inflammation in the acute stage - hyperemia, pain, itching, etc.).
Today, terzhinan is one of the few local drugs that have a wide spectrum of action due to a well-chosen combination of components.
Taking into account the characteristics of candidiasis infection, as well as the pharmacodynamics and pharmacokinetics of the above antimycotics, we have developed the following treatment regimen for vulvovaginal candidiasis and assessed its clinical effectiveness. We conducted a clinical and microbiological examination of 56 patients aged 18 to 49 years with vulvovaginal candidiasis, confirmed by microscopic and cultural methods. Most patients noted an improvement in their condition already on the 3rd - 4th day of treatment. Mycological sanitation and complete clinical recovery were achieved in 53 (94.6%) patients.
The proposed scheme includes drugs with different points of application, simultaneously affecting various stages of the life activity and metabolism of the pathogen, as well as all possible systemic reservoirs of yeast-like fungi.
Mycomax (per os) 150 mg twice (first dose on day 1, second dose on day 6).
Gyno-travogen - 1 vaginal suppository deep into the vagina at night, day 1.
Pimafucin (per os) 100 mg 4 times a day - 10 days from the 2nd day of treatment.
In this scheme, mycomax affects the causative agent of candidal vulvovaginitis, as well as all possible systemic reservoirs of yeast-like fungi, pimafucin - thanks to the enteric coating, acts only in the intestine (the main reservoir and trigger for the recurrence of candidal vulvovaginitis), gyno-travogen - a drug for topical use, affecting yeast-like fungi and gram-positive microorganisms (for vaginal infections of fungal and mixed origin).
The proposed treatment regimen for vulvovaginal candidiasis is highly effective, quickly relieves symptoms, reduces the rate of relapse, and helps to increase the effectiveness of therapy for this widespread gynecological disease. Frequent recurrence of the disease after antimycotic treatment with various drugs allows us to recommend this complex therapy for the treatment of both acute and chronic recurrent vulvovaginal candidiasis in non-pregnant and non-lactating women.
For the treatment of vulvovaginal candidiasis in pregnant women, the above-mentioned drugs can be used:
- pimafucin - 1 vaginal suppository 1 time per day at night for 6 days or
- terzhinan - 1 vaginal tablet 1 time per day at night for 6 - 10 days.
If a sexual partner has balanitis, pain before and after coitus, treatment with the drug mifungar in the form of a cream is recommended, which is applied in a thin layer 2 - 3 times a day.
We are faced with great difficulties in the treatment of genital candidiasis also due to the fact that most often candidiasis is not a sexually transmitted disease, but a marker of trouble in the body (immunodeficiency conditions, dyshormonal disorders, etc.). In this regard, in parallel with antimycotic therapy, it is necessary to correct conditions leading to the development of vulvovaginal candidiasis.
Despite the fact that there are certain treatment regimens for vulvovaginal candidiasis, the choice of drug in each specific case should depend on the severity of the clinical course of the disease, the presence of mixed infection and concomitant diseases. Only such an integrated approach to this problem will improve the effectiveness of treatment of vulvovaginal candidiasis and reduce the frequency and percentage of recurrence of this disease.
Literature
- Bayramova G.R. Candida infection. Polyene antibiotics in the treatment of vaginal candidiasis // Gynecology. 2001. vol. 3. No. 6. P. 212 - 14.
- Burova S. A. Complex treatment of patients with vulvovaginal candidiasis using Diflucan // Proc. report scientific-practical conf. "New in the diagnosis and treatment of sexually transmitted diseases and skin diseases." Moscow, 22 - 23 October. 1997.
- Bykov V. L. Etiology, epidemiology and pathogenesis of vulvovaginal candidiasis // Obstetrics and gynecology. 1986. No. 9. P. 5 - 7.
- Kisina V.I., Stepanova Zh.V., Mirzabekova M.A., Kurchavov V.A. Dependence of the clinical picture of vulvovaginal candidiasis on the species composition of Candida fungi and the effectiveness of fluconazole in primary and recurrent candida infections // Gynecology. 2000. No. 6. t. 2. P. 193 - 195.
- Muravyova V.V., Ankirskaya A.S. Features of vaginal microecology in bacterial vaginosis and vaginal candidiasis // Obstetrics and Gynecology 1996. No. 6. P. 27 - 30.
- Prilepskaya V.N. Clinic, diagnosis and treatment of vulvovaginal candidiasis (clinical lecture) // Gynecology. 2001. No. 6. T. 3. P. 201 - 205.
- Prilepskaya V.N., Bayramova G.R. Modern ideas about vaginal candidiasis // Russian Medical Journal. 1998. No. 5. T. 6. P. 301 - 308.
- Bingham JS What to do with the patient with recurrent vulvovaginal candidiasis // Sex. Transm. Inf. 1999. 75. 225 - 227.
- Granger SE The etiology and pathogenesis of vaginal candidosis: an update // Br. J. Clin. Bact. 1992. V. 46. No. 4. 258 - 259.
- Horowitz BJ Mycotic vulvovaginitis: a broad overview // Am. J. Obstet. Gynecol. 1991. V. 165. No. 4. 1188 - 1192.
- Mikamo H., Kawazoe K., Sato Y., Izumi K., Ito T. Penetration of Oral Fluconazole into Gynecological Tissues // Antimicrobial Agents and Chemotherapy. 1999. Vol. 43. No. 1. 148 - 151.
- Perry CM, Whittington R. Fluconazole // Drugs. 1995. Jun. 49(6). 984 - 1006. Ref. 111.
A. L. Tikhomirov, Doctor of Medical Sciences, Professor Ch. G. Oleinik, MGMSU, Moscow
Note!
- Currently, vulvovaginal candidiasis ranks second among all vaginal infections and is one of the most common reasons for women seeking medical help.
- The causative agent of vulvovaginal candidiasis is yeast-like fungi of the genus Candida. Fungi of the genus Candida are opportunistic microorganisms that live as saprophytes on the skin and mucous membranes of healthy people.