People often call this disease a cold, although in fact it is caused by various pathogens. Hypothermia itself is not a direct cause; it only creates favorable conditions for the development of infection.
Rhinopharyngitis occurs in both adults and children. Usually it is tolerated quite easily, without complications and goes away within 7 days. For this to happen, you don’t need to wait for the situation to worsen. Contact your doctor when the first symptoms appear. He will prescribe adequate treatment and help cope with the disease in a short time.
Reasons for the development of the disease
According to the etiology of occurrence, the disease is divided into several types: chronic or acute, infectious or non-infectious (most often allergic). Accordingly, there are a number of reasons that can lead to the development of the disease. The main list includes:
- infection with various infections. In most cases, we are talking about viral infections (rhinoviruses, coronaviruses, adenoviruses, ECHO virus, influenza viruses, etc.). And only 20–30% are due to other infections - bacterial and fungal;
- the occurrence of allergic reactions to pollen, animal hair, mites, taking any medications, etc.;
- untreated rhinitis, against the background of which similar complications developed;
- neuroendocrine and autoimmune disorders, mechanical and chemical effects - such etymology is extremely rare, but also possible.
In practice, rhinopharyngitis most often occurs of a mixed nature (for example, polymicrobial or infectious-allergic).
In addition to the direct etymology, there is a set of factors that contribute to infection. These are weakened immunity, frequent hypothermia, stressful situations, the presence of chronic diseases of the respiratory system, anatomical features that make breathing difficult (deviated nasal septum, enlarged adenoids, etc.).
The transition of the disease to a chronic form can be caused by incorrect or untimely treatment, therefore, even with a mild form, it is important not to treat yourself, but to consult a specialist.
Rhinopharyngitis (nasopharyngitis)
Terminology
First of all, we note that the terms “rhinopharyngitis” and “nasopharyngitis” mean the same thing - both in translation and in essence.
The only difference is that in the first case the nose is Greek, and in the second it is Roman (not the nose itself, of course, but the first root in the word). The suffix “-itis” immediately sets the inflammatory register, and as a result we get “inflammation of the nose and pharynx.” But no one says that. In medicine, this zone of the human body - and it is a system of cavities and passages covered with mucous membranes, complex in form, function, innervation, vasculature - is divided into three sections: the nasopharynx, oropharynx and laryngopharynx. Therefore, inflammation of the nasopharynx. Not just a “runny nose” (rhinitis) as inflammation of the mucous membrane in the nasal (nasal) cavity, but inflammation of the entire nasopharynx as a whole; in the simplest terms, a runny nose plus a sore throat.
There are various synonyms in the literature - for example, the very strange “rhinonasopharyngitis” (inflammation of the nasopharynx) or the more understandable “epipharyngitis” (inflammation of everything that is located above and/or around the pharynx). In addition, one cannot help but recall the fantastic word “cold” - the people’s favorite diagnosis with zero content. On the other hand, one might not judge so harshly - there is, after all, a semi-official term “colds”, and a cold in everyday speech probably means an acute respiratory infection caused by hypothermia - if not for frequent dialogues like this: “This is Do you have an acute respiratory infection or allergies? - Neither one nor the other. I just caught a cold." These issues are discussed in a little more detail in the material “ORZ. ARVI. Flu". After all, equivalents of the word “cold” have existed since ancient times in all languages of the world, while the true etiopathogenesis of the diseases denoted by this word became known literally yesterday - from the mid-twentieth century; Let's make allowances for this and focus on the essence.
Rhinopharyngitis is mentioned in the oldest known medical document (the so-called Ebers papyrus, c. 1600 BC, represents a body of much older knowledge) and to this day remains the most common human disease. By virtue of this fact alone, nasopharyngitis constitutes a global medical and social problem. Temporary disability caused by a “common cold” costs fabulous sums of money every year, and therefore nasopharyngitis remains the focus of attention of researchers, clinicians, epidemiologists, sanitary and hygienic services and insurance companies. It’s high time for humanity to get rid of and forget this seemingly trivial disease. But it doesn't work. According to average epidemiological data, every adult on the globe suffers 2-3 rhinopharyngitis per year; each child – 6-10 episodes; every school-age child – up to 12 nasopharyngitis per year. During periods of seasonal epidemics, only a fifth of the population remains healthy. In the United States alone, rhinopharyngitis eliminates 128 million workdays annually due to the fact that parents (mothers, especially) are forced to stay with sick children; Another 150 million “person-days” are lost due to nasopharyngitis in adults themselves. Such accounting meticulousness does not cause a smile, but respect: 20 billion dollars a year is serious money not only for “poor but clean” America, but also for any other state (regarding Russia, unfortunately, no such data can be found managed).
Symptoms of the disease
Infectious nasopharyngitis has a fairly short incubation period (16–24 hours), during which you may experience primary, mild and almost imperceptible symptoms. After infection, a person feels increased fatigue, a mild headache, sneezes more, and a feeling of cold appears (when it seems to be warm, but the patient feels chills).
Further, the symptoms become more pronounced and noticeable. The classic list for the acute course of the disease includes:
- general malaise and drowsiness;
- chills and increased body temperature (usually no more than 38.5 degrees);
- difficulty breathing, runny nose and nasal congestion;
- slight sore throat and redness;
- dry cough;
- a feeling of discomfort, itching and burning in the nasopharynx (itching and sneezing are especially evident with allergic etiology of rhinopharyngitis);
- headache, sleep and appetite disturbances;
- ear pain and hearing loss;
- enlarged cervical and occipital lymph nodes.
With proper treatment and strong immunity, all these manifestations disappear after 6–8 days. In other cases, the disease can last much longer, spreading to the larynx, bronchi, and hearing organs.
As for the symptoms of a chronic disease, they appear a little milder, but create constant discomfort due to difficulty breathing all the time and a sore throat.
What is sinusitis?
Sinusitis is an inflammation of the paranasal sinuses (closed air cavities in the facial bones lined with mucous membrane). The infection may be bacterial or viral in nature. In acute cases, sinusitis most often occurs in conjunction with inflammation of the nasal mucosa, i.e. there is a condition better known as rhinosinusitis. With sinusitis, there may be copious purulent discharge from the nose with mucus, which also ends up in the throat, which is a sign of a bacterial infection. Patients are concerned about pain in the forehead or face at the level of the frontal or maxillary sinuses, decreased or loss of smell, and increased temperature.
Every day we inhale up to 15,000 liters of air, which is normally filtered, heated and humidified before entering the paranasal sinuses through a small opening. With chronic swelling of the nasal mucosa, displacement of the nasal septum and other anatomical defects of the nose, a favorable environment is created for the development of bacteria and, consequently, for the development of infection.
How is diagnosis carried out?
The first rule of any disease is not to self-medicate, but to consult a doctor. For nasopharyngitis, as a rule, a visit to a therapist is sufficient. He listens to the patient, conducts a clinical examination and immediately makes a diagnosis. When the disease occurs, a fairly clear picture of the mucous membranes appears, which allows for an accurate diagnosis without additional examinations.
If the disease is advanced, there are risks of complications, chronic diseases and similar reasons, the therapist will refer you to an ENT specialist for a comprehensive diagnosis, prescribing specialized treatment and physiotherapeutic procedures.
Bacteriological studies are most often not carried out due to the sufficiency of clinical examination and symptoms, but can be prescribed if the etymology of the disease and the identification of its causative agent plays a decisive role in the choice of therapy.
Complications
If acute nasopharyngitis is not treated, it can become chronic.
There is also a risk of developing the following complications:
- addition of a bacterial infection;
- laryngitis;
- sinusitis;
- sinusitis;
- tracheitis;
- inflammation of the middle ear (which can lead to hearing loss);
- bronchitis;
- pneumonia.
Respiratory infections can cause exacerbation of existing chronic diseases, such as bronchial asthma.
Treatment of the disease: physiotherapy and medication
In the majority of cases, nasopharyngitis goes away on its own, that is, the body overcomes it on its own. Therapy in this situation is aimed more at helping him, mitigating the symptoms and preventing the development of complications.
The main thing that is prescribed to the patient is bed rest or home rest, plenty of fluids and a fortified diet. You should avoid contact with other people, because the infectious disease is transmitted by airborne droplets.
Depending on the severity of symptoms, the following measures may be prescribed:
- rinsing the nose (nasal spray, sea or thermal water, saline);
- antiseptic gargling (with physiotherapeutic infusions and herbal decoctions), inhalations;
- use of vasoconstrictors and decongestants;
- taking antihistamines (if the disease is allergic);
- taking painkillers (for severe pain) and antipyretics (for fever);
- the use of dry cough syrups, which facilitate expectoration and help remove pathogens (if the cough is already wet, such drugs are not prescribed);
- lozenges to relieve sore throat;
- taking antimicrobial or antiviral drugs.
In mild cases, the last group of medications is not used at all, but if treatment requires more stringent measures, most likely, the specialist will prescribe antiviral drugs, because the most common pathogen is viruses. Antibiotics are prescribed when bacterial etiology is confirmed. Using them on your own will not only not help therapy, but can also harm it.
Hypertrophic pharyngitis
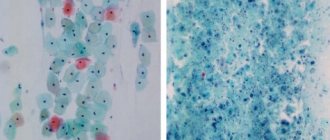
For hypertrophic pharyngitis
The patient's complaints are similar to those with the catarrhal form of the disease, but in this case
there is more mucous discharge and it is more viscous
, which causes discomfort, since it is necessary to constantly cough up, which can provoke an attack of vomiting.
With this type of pharyngitis, there are lymphoid accumulations (groups of follicles) on the mucous membrane of the pharynx, which are pronounced.
In case of large accumulation and increase in size, these follicles turn into granules, and the disease is designated as granulosa chronic pharyngitis.
For hypertrophic pharyngitis, alkaline gargling is also recommended; inhalations with essential oils of medicinal herbs (sage, chamomile and eucalyptus) are also useful.
Hypertrophic granulosa pharyngitis
has a characteristic symptom - a tickling sensation in the throat, its other symptoms are similar to those of hypertrophic pharyngitis.
Treatment of granulosa pharyngitis
can be therapeutic and surgical
Therapeutic
– similar to the treatment of catarrhal chronic pharyngitis.
Surgical
the intervention is carried out using a radio wave or laser beam. During surgery, the granules themselves are removed, but to completely cure the pathology, therefore, after removal of the granules, drug treatment is still required.
The patient should stop smoking.
Is prevention possible?
Preventive measures to prevent nasopharyngitis are general. Since a person who has had the disease remains contagious for up to 20 days, it is advisable to avoid close contact with him. Make sure that each household member has their own towels, mugs and other personal items.
Wash your hands regularly, not only after visiting public places, but also after blowing your nose, so that microorganisms are not transferred from one organ to another. Use hand sanitizer.
When coughing or sneezing, cover your mouth with a disposable tissue folded several times. If there is no tissue nearby, it is better to sneeze and cough not into your palm, as everyone is used to, but into the crease of your elbow. In this way, we also reduce the likelihood of becoming carriers of infection to ourselves.
Ventilate the room you are in well, do not overheat it, and maintain normal air humidity. Follow the treatment prescribed by your doctor exactly and do not interrupt it until the prescribed course is completed.
Is it possible to get nasopharyngitis from a sick person?
When the disease is caused by a viral infection, it is contagious and is transmitted from an infected person to an uninfected person through particles of fluid (saliva or nasal secretions) when coughing or sneezing or when breathing, since viruses can be in the exhaled air of an infected person. Thus, the main mechanism of infection with nasopharyngitis is airborne.
The lifespan of nasopharyngitis pathogens outside the human body can vary from several minutes to several hours.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 10 | 25 | 25 | 25 | 25 | 0 | 0 | 10 | 25 | 25 | 25 | 25 |
Traditional treatment
Treatment with folk remedies will help improve your condition and maintain your health.
- Using a humidifier. To thin out secretions, it is recommended to humidify the surrounding air and maintain the room temperature to 19 degrees.
- Inhalation of eucalyptus essential oils.
It is necessary to do inhalations so that it has a decongestant effect, helping to clear a stuffy nose. Essential oils can also be used in chest massage. But remember that treating colds with essential oils is contraindicated for children, pregnant or lactating women, patients with asthma or epilepsy. Consult your doctor before use. - Elder. Has antipyretic and anti-edematous effects. This plant can be used as an herbal tea (let steep for at least 10 minutes) or as a gargle (with cooled herbal tea) several times a day.
- Chamomile. For children, a runny nose can be very uncomfortable because it prevents them from breathing, causing them to be irritable and may lose their appetite. In these cases, it is best to resort to homemade solutions prepared with the addition of salt or chamomile.
Rhinopharyngitis can be treated well with folk remedies if you follow the above steps and know how to treat it.
Popular questions about Nasopharyngitis
What happens if the disease is not treated?
Inflammation can spread from the nasopharynx to other tissues and cause the following complications: sinusitis, sinusitis, otitis media, laryngitis, tracheitis, bronchitis, pneumonia.
What herbal preparations are there?
Herbal-based products have a less pronounced vasoconstrictor effect than decongestants, but they are not addictive. Pinosol oil drops show good effectiveness.
Which doctor should I contact?
An otolaryngologist specializes in diseases of the ENT organs.