Furagin
A broad-spectrum antimicrobial agent belonging to the nitrofuran group. Under the influence of nitrofurans, the respiratory chain and the tricarboxylic acid cycle (Krebs cycle) are suppressed, as well as other biochemical processes of microorganisms are suppressed, resulting in the destruction of their shell or cytoplasmic membrane.
Active against gram-positive cocci: Streptococcus spp., Staphylococcus spp.; gram-negative rods: Escherichia coli, Salmonella spp., Shigella spp., Proteus spp., Klebsiella spp., Enterobacter spp.; protozoa: Lamblia intestinalis and other microorganisms resistant to antibiotics.
Furazidin is more active against Staphylococcus spp., Escherichia coli, Aerobacter aerogenes, Bacterium citrovorum, Proteus mirabilis, Proteus morganii, compared to other nitrofurans.
For most bacteria, the bacteriostatic concentration ranges from 1:100,000 to 1:200,000. The bactericidal concentration is approximately 2 times higher.
As a result of the action of nitrofurans, microorganisms produce fewer toxins, and therefore an improvement in the patient’s general condition is possible even before a pronounced suppression of the growth of microflora. Nitrofurans activate the body's immune system: they increase the complement titer and the ability of leukocytes to phagocytose microorganisms. Furazidine in therapeutic doses stimulates leukopoiesis.
Resistance to furazidine develops slowly and does not reach a high degree.
Pharmacokinetics
After oral administration, furazidine is absorbed from the small intestine by passive diffusion. Absorption of nitrofurans from the distal segment of the small intestine exceeds absorption from the proximal and medial segments by 2 and 4 times, respectively (should be taken into account during the simultaneous treatment of urogenital infections and gastrointestinal diseases, in particular chronic enteritis). Nitrofurans are poorly absorbed from the colon.
Cmax in blood plasma lasts from 3 to 7 or 8 hours; furazidine is detected in urine after 3-4 hours.
Furazidin is distributed evenly in the body. The high content of the drug in the lymph is clinically important (it delays the spread of infection through the lymphatic tract). In bile its concentration is several times higher than in serum, and in cerebrospinal fluid it is several times lower than in serum. In saliva, the content of furazidin is 30% of its concentration in serum. The concentration of furazidin in the blood and tissues is relatively small, which is associated with its rapid release, while the concentration in the urine is much higher than in the blood.
Metabolized to a small extent (<10%).
Excreted by the kidneys by glomerular filtration and tubular secretion (85%), partially undergoes reverse reabsorption in the tubules. At low concentrations of furazidin in the urine, the process of filtration and secretion predominates; at high concentrations, secretion decreases and reabsorption increases. Furazidine, being a weak acid, does not dissociate in acidic urine and undergoes intense reabsorption, which can enhance the development of systemic side effects. With an alkaline reaction of urine, the excretion of furazidine increases.
As the excretory function of the kidneys decreases, the metabolic rate increases.
Instructions for use FURAGIN
The drug is usually well tolerated, but side effects are possible.
The incidence of adverse drug reactions is the percentage of the number of patients who experienced an adverse reaction to a drug at a given time to the total number of patients who used that drug at a certain time.
Adverse reactions are listed according to systemic organ classes, in descending order of frequency. Criteria for the incidence of adverse reactions:
- over 10% - very frequent;
- 1-10% - frequent;
- 0.1-1% - infrequent;
- 0.01-0.1% - rare;
- less than 0.01% - very rare.
Blood and lymphatic system disorders:
very rare - hematopoietic disorders (agranulocytosis, thrombocytopenia, aplastic anemia).
Nervous system disorders:
Uncommon: dizziness, drowsiness, blurred vision;
- rare - peripheral neuropathy;
- very rare - mild intracranial hypertension.
- rare - vomiting, diarrhea;
- very rare - pancreatitis (inflammation of the pancreas).
- very rare - angioedema, urticaria, dermatitis, Erythemamultiforme.
Disorders of the respiratory system, chest and mediastinal organs:
rare - acute and chronic pulmonary reactions. An acute pulmonary reaction develops rapidly. It is manifested by severe shortness of breath, fever, chest pain, cough with or without sputum, eosinophilia (increased number of eosinophilic granulocytes in the blood). There is information about the simultaneous appearance of skin rashes, itching, urticaria, myalgia (muscle pain), and angioedema (swelling of the face, neck, oral tissues and larynx) with an acute pulmonary reaction. The basis of an acute pulmonary reaction is a hypersensitivity reaction that can develop over several hours, less often within minutes. The acute pulmonary reaction is reversible and disappears when the drug is stopped. A chronic pulmonary reaction can develop over a long period of time after stopping treatment with nitrofurans (including furagin). Characterized by a gradual increase in dyspnea, tachypnea, unstable fever, eosinophilia, progressive cough and interstitial pneumonitis and/or pulmonary fibrosis.
Gastrointestinal disorders:
infrequently - loss of appetite, nausea;
Disorders of the skin and subcutaneous tissues:
rare - papular rash, itching, transient hair loss;
Musculoskeletal and connective tissue disorders:
very rare - arthralgia (joint pain).
General violations:
rare - weakness, increased body temperature.
Disorders of the liver and biliary tract:
very rare - cholestatic jaundice, hepatitis.
Furagin turns urine brown.
Side effects are reduced if the drug is taken after meals with plenty of liquid.
If side effects occur, reduce the dose or stop taking the drug.
Modern approaches to the treatment of pyelonephritis in children
What diet is recommended for pyelonephritis? What is the choice of antibiotic based on and what is the duration of its use? In what cases is combined antibacterial therapy preferred?
Complex treatment of pyelonephritis involves the organization and implementation of measures aimed at eliminating the microbial inflammatory process in the renal tissue, restoring the functional state of the kidneys, urodynamics, and immune disorders. The choice of therapeutic measures is determined by the state of the macroorganism, the form of pyelonephritis (obstructive, non-obstructive), the phase of the disease (active phase, remission), and the biological properties of the pathogen itself.
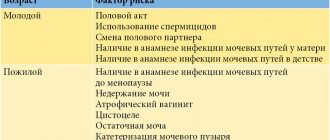
During the period of pronounced activity of the microbial inflammatory process, bed or semi-bed rest is recommended. The regimen is expanded starting from the second week of the disease, after the disappearance of extrarenal manifestations. The diet is based on the activity of the disease, the functional state of the kidneys, as well as the presence or absence of metabolic disorders. During the active phase of pyelonephritis, it is recommended to limit the intake of foods containing excess protein and extractives, exclude or limit foods that require high energy costs for metabolism, as well as limit the consumption of foods containing excess sodium. In case of acute pyelonephritis, a dairy-vegetable diet with moderate restriction of protein (1.5–2.0/kg) and salt (up to 2–3 g per day) is prescribed for 7–10 days. In the absence of obstruction of the urinary system, sufficient drinking (50% more than the age norm) is recommended in the form of “weak” tea, compotes, and juices. Therapeutic nutrition for chronic pyelonephritis should be as gentle as possible for the tubular apparatus of the kidneys. It is recommended to take slightly alkaline mineral waters (such as Slavyanovskaya, Smirnovskaya) at the rate of 2–3 ml/kg of body weight per dose for 20 days, 2 courses per year.
Patients with pyelonephritis should follow a “regular” urination regime - urinate every 2-3 hours, depending on age. It is necessary to monitor regular bowel movements and toileting of the external genitalia. Daily hygiene measures are shown - shower, bath, wiping, depending on the child’s condition. Physical therapy is carried out lying down or sitting, again depending on the child’s condition.
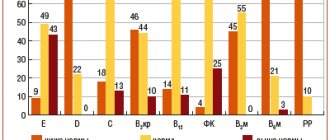
For many years, the main etiologically significant microflora of urine in pyelonephritis in children and adults has been E. coli, which has a large set of virulence factors. In 2000 - 2001, a scientific study of ARMID was conducted in 8 medical institutions in 7 cities of Russia, which was coordinated by L. S. Strachunsky and N. A. Korovina. We examined 607 children aged from 1 month to 18 years with community-acquired infections of the upper and lower urinary system, in whom a bacteriological examination of urine identified the pathogen in a diagnostic titer (>=105 CFU/ml). The sensitivity of the isolated microorganisms to antimicrobial drugs of the main groups was determined. As a result of the study, it was shown that urinary system infections (UTIs) in the vast majority of cases are caused by one type of microorganism, but if several types of bacteria are detected in the test samples, it is necessary to exclude violations of the technique for collecting and transporting the material. At the same time, microbial associations can also be determined during the chronic course of urorenal infection.
According to the data obtained, the main causative agents of community-acquired UTIs in Russia are representatives of the Enterobacteriaceae family (80.6%), mainly E. coli, which was detected in 53.0% of cases (with variations from 41.3 to 83.3% in different centers ). Other uropathogens were isolated much less frequently. Thus, Proteus spp. was found in 8.5%, Enterococcus spp. - in 8.5%, Klebsiella pneumoniae - in 8.0%, Enterobacter spp. - in 5.7%, Pseudomonas spp. - in 5.4%, Staphylococcus aureus - in 3.7% of children. It should be noted that in 7.2% of patients the following microorganisms were detected, which are usually rarely found in clinical practice: Morganella morganii - 2.0%, Klebsiella oxytoca - 1.7%, Citrobacter freundii - 1.1%, Serratia marcescens - 0 .8%, Acinetobacter lwoffii - 0.5%, Acinetobacter baumannii - 0.3%, Citrobacter diversus - 0.2%, Streptococcus pyogenes - 0.2%, Flavobacter spp. - 0.2%, Candida kruzei - 0.2%. The structure of uropathogens in different regions of Russia was different. A higher frequency of K. pneumoniae isolation was observed in St. Petersburg (12.3%); Enterococcus spp. — in Irkutsk and Kazan (22.9 and 13.5%, respectively). The data obtained indicate the need for regular microbiological monitoring in various regions of the country.
In most patients with acute pyelonephritis, before the pathogen is isolated, “starting” antibacterial therapy is prescribed empirically, that is, taking into account knowledge about the etiological characteristics of the most likely pathogens and their potential sensitivity to this drug, since urine culture and sensitivity determination take time, and the start of therapy is delayed unacceptable. In the absence of clinical and laboratory (urinalysis) effect, after three days of empirical therapy, its correction is carried out by changing the antibiotic, taking into account the data obtained on the nature of the microbial flora and the sensitivity of the drug to it. In severe cases of infection, the success of therapy is largely determined by timely bacteriological examination of urine.
In case of mild pyelonephritis, the oral route of antibiotic administration can be used - there are special children's forms of antibiotics (syrup, suspension), which are characterized by good absorption from the gastrointestinal tract and pleasant taste. The parenteral route of antibiotic administration is used for severe and moderate pyelonephritis and provides for a subsequent transition to the oral route - “stepped” therapy. When choosing a drug, preference should be given to bactericidal antibiotics. The duration of antibacterial therapy should be optimal, until the activity of the pathogen is completely suppressed (for acute pyelonephritis and exacerbation of chronic pyelonephritis in a hospital setting, antibacterial drugs are usually prescribed continuously for 3 weeks, with a change of drug every 7 - 10 - 14 days). Lysozyme, recombinant interferon preparations (Viferon), and herbal medicine potentiate the effect of antibiotics.
In severe cases of pyelonephritis, combined antibacterial therapy or the introduction of second-line drugs is practiced.
Combined antibacterial therapy in nephrology is used for the following indications:
- severe septic course of the microbial inflammatory process in the renal tissue (in order to use the synergism of the action of antibacterial drugs);
- severe pyelonephritis caused by microbial associations;
- in order to overcome the multiresistance of microorganisms to antibiotics (especially in the treatment of “problematic” infections caused by Proteus, Pseudomonas aeruginosa, Citrobacter, Klebsiella, etc.);
- to influence intracellular microorganisms (chlamydia, mycoplasma, ureaplasma).
| Structure of pathogens of community-acquired UTIs in children in Russia |
In severe cases of pyelonephritic process, most often a combination of antibiotics is used to expand the spectrum of antimicrobial action, which is especially important in the absence of data on the causative agent. When combining two drugs, it is necessary to take into account their mechanism of action, pharmacokinetic and pharmacodynamic features, that is, simultaneously use bactericidal and bactericidal antibiotics, and combine drugs with bacteriostatic action with similar ones. In patients with severe pyelonephritis, continuous antibacterial therapy is carried out until the pathogen is completely suppressed, changing the antibiotic every 10-14 days if effective. Against the background of maximum activity of pyelonephritis, accompanied by a syndrome of endogenous intoxication, infusion-corrective therapy is indicated. The composition and volume of infusion therapy depend on the patient’s condition, homeostasis indicators, diuresis and other renal functions. In case of severe, purulent pyelonephritis, the urologist installs a nephrostomy tube and a urethral catheter.
After receiving the results of a bacteriological examination of urine, if there is no effect from empirical therapy, etiotropic therapy is carried out in accordance with the nature of the cultured urine microflora and sensitivity.
In some cases, with exacerbation of chronic pyelonephritis, older children can be treated on an outpatient basis with the organization of a “hospital at home”. “Protected” penicillins and third-generation cephalosporins are used as antibacterial therapy. Aminoglycosides should not be used in outpatient practice. In the clinic, under the supervision of a nephrologist and local pediatrician, after a course of continuous antibacterial therapy in the presence of obstruction, anti-relapse treatment is carried out for 4-6 weeks or more, depending on the nature of the urodynamic disorders.
The following anti-relapse therapy options are recommended:
- furagin at the rate of 6-8 mg/kg body weight (full dose) for 2-3 weeks; then, when urine and blood tests are normalized, they switch to 1/2-1/3-1/4 of the maximum therapeutic dose for 2-4-8 or more weeks, depending on the nature of the identified urodynamic changes;
- co-trimoxazole (Biseptol) at the rate of 2 mg of trimethoprim + 10 mg of sulfamethoxazole per kilogram of body weight orally 1 time per day for 4 weeks.
One of the listed drugs can be prescribed for 10 days every month for a period of 3-4 months in age-specific dosages:
- nalidixic acid (negram, nevigramon);
- pipemidic acid (pimidel, palin, pipegal, etc.);
- 8-hydroxyquinoline (nitroxoline, 5-NOC).
Against the background of maximum activity of pyelonephritis, accompanied by a syndrome of endogenous intoxication, infusion-corrective therapy is indicated. The composition and volume of infusion therapy depend on the patient’s condition, homeostasis indicators, diuresis and other renal functions.
As a rule, in the acute period of pyelonephritis, given the high activity of the body's antioxidant system, antioxidant therapy is not carried out. As the microbial inflammatory process in the renal tissue subsides, after 3-5 days from the start of antibacterial therapy, antioxidants are prescribed for a period of 3-4 weeks (vitamin E, C, vetoron, drugs containing selenium - triovit, seltsinc, etc.). Taking into account the fact that secondary mitochondrial dysfunction is observed in the microbial inflammatory process in the renal tissue, its medicinal correction involves the use of coenzyme Q10 preparations (kudesan, synergin), polyunsaturated fatty acid carriers (L-carnitine), cofactors of enzymatic reactions of energy metabolism (riboflavin, nicotinamide , lipoic acid), dimephosphone.
In order to improve renal blood flow in patients with pyelonephritis, aminophylline and magnetic therapy courses are used.
In most children, pyelonephritis is usually accompanied by pronounced changes in the body's immune system, affecting the course and progression of the disease.
Immunocorrective therapy for pyelonephritis is prescribed:
- young children with age-related immune dysfunction;
- in severe and recurrent variants of the course of pyelonephritis, occurring against the background of multiple organ failure and developmental defects;
- with prolonged course of pyelonephritis in the postoperative period;
- for pyelonephritis in frequently ill children;
- for pyelonephritis caused by “hospital”, multi-resistant strains (Pseudomonas, Proteus, Enterobacter, Citrobacter, Serratia, Hafnia, etc.) and mixed infection.
Immunomodulatory therapy in the phase of maximum activity is usually not prescribed; it is indicated when the microbial inflammatory process subsides. The use of immunomodulatory therapy for pyelonephritis in children contributes to:
- reducing the duration of the active period of the disease and the length of the patient’s stay in the hospital;
- reducing the risk of recurrence of pyelonephritis and repeated respiratory infections.
Recombinant interferon preparations (viferon, reaferon) are used. Viferon is prescribed rectally depending on age: children under 7 years of age are given Viferon-1 (150 IU) 1 suppository twice a day for 7-10 days, then in intermittent courses 2-3 times a week for 4-6 weeks. Children over 7 years old are prescribed Viferon-2 (500 IU). A similar course of treatment is carried out in young children.
Reaferon is used intramuscularly 2 times a day, no more than 2 million IU. The drug is administered daily for 5-7 days. For the purpose of immunocorrection, lysozyme can be used (orally at the rate of 5 mg/kg body weight per day (no more than 100-200 mg per day) for 10-20 days or intramuscularly at the rate of 2-5 mg/kg body weight). The use of licopid is justified; the drug is prescribed to children starting from the neonatal period, 1 tablet (1 mg) once a day for 10 days. In children over 14 years of age, you can use adult dosages (10 mg tablets) - 1 tablet (10 mg) 1 time per day for 10 days. While taking licopid, a short-term increase in temperature in the range of 37.1-37.5°C may be observed. In some cases, for the purpose of immunocorrection, Immunal is used, which is prescribed orally 3 times a day for 4 weeks (children from 1 to 6 years old, 15-30 drops, over 7 years old, 30-45 drops per dose).
Bacteriophages are administered orally after persistent seeding of the same type of pathogen from urine and feces; with persistent isolated bacteriuria. Herbal medicine is indicated during remission. Herbs that have anti-inflammatory, antiseptic, and regenerating effects are recommended.
For obstructive pyelonephritis, treatment is carried out together with a pediatric urologist or pediatric surgeon. The issue of indications for surgical treatment, bladder catheterization, etc. is being resolved. When choosing antibacterial drugs in children with obstructive pyelonephritis, it is necessary to take into account the state of kidney function and the nephrotoxicity of antibiotics. The use of aminoglycosides for severe obstruction is not indicated. In patients with a slight decrease in glomerular filtration, the doses of “protected” penicillins and cephalosporins may not be adjusted. When glomerular filtration decreases by more than 50% according to the Rehberg test, the doses of these drugs should be reduced by 25-75%. In case of pronounced activity of obstructive pyelonephritis with manifestations of endogenous intoxication syndrome, along with etiotropic treatment, infusion-corrective therapy is carried out. If arterial hypertension is detected, the issue of prescribing antihypertensive drugs is decided.
The success of therapy for pyelonephritis, which develops against the background of metabolic disorders, depends on timely correction of nutrition, the appointment of an appropriate drinking regime, and the use of drugs that normalize metabolic processes. For oxaluria, vitamins B6, E, A are prescribed. The duration of the course of treatment is 15-30 days, repeated courses are carried out quarterly. You can use a 2% solution of xydiphone at the rate of 3 mg/kg of body weight per day (tea, dessert, tablespoon, depending on age), the course of treatment is up to 3-4 weeks. Xidifon is contraindicated for hypercalcemia and is taken together with vitamin E. For hyperoxaluria, magnesium oxide is indicated, which is prescribed in a dose of 50-100-200 mg/day, depending on age, once a day for 2-3 weeks in courses 3-4 times a year. A decoction of oats and an infusion of flax seed are indicated; courses lasting 1 month, 4 courses per year, are conducted.
For secondary pyelonephritis against the background of hyperuraturia, vitamin B6 is indicated (in the first half of the day, from 10 to 60 mg per day, depending on the severity of uraturia, for 3-4 weeks). Potassium orotate, which has a uricosuric effect, is prescribed (0.3-0.5 g 2-3 times a day, treatment course is 2-4 weeks), antioxidants (vitamins A, E, C), urolesan, soluran, blemaren, magurlit, uralit .
Treatment of pyelonephritis of a single kidney is carried out according to the generally accepted method, taking into account the nephrotoxicity of antibacterial drugs (the use of aminoglycosides, first generation cephalosporins, carbapenems, monobactams must be avoided). When prescribing antibacterial drugs, one should take into account the condition of the kidneys and, if the function of the latter decreases, use average doses of drugs. If arterial hypertension develops, antihypertensive drugs are prescribed. If renal failure develops, treatment is carried out in a dialysis center.
Vaccination of children with pyelonephritis is carried out after achieving remission, with mandatory preliminary laboratory monitoring of blood and urine tests in order to clarify the activity of the process and the functional state of the kidneys. Vaccination is carried out according to an individual schedule.
Indications for sanatorium-resort treatment in patients with pyelonephritis are:
- period of subsidence of acute pyelonephritis (3 months from the onset of disease activity);
- primary pyelonephritis during remission without renal dysfunction and arterial hypertension;
- secondary pyelonephritis during remission without renal dysfunction and arterial hypertension;
Thus, the complexity and versatility of the pathogenetic mechanisms underlying pyelonephritis in children, the high risk of chronicity of the disease associated with the characteristics of macro- and microorganisms, require not only the timely detection of the microbial inflammatory process in the renal tissue and urinary tract with the subsequent use of sufficiently intensive antibacterial therapy, but also a whole range of therapeutic measures aimed at normalizing metabolic disorders, the functional state of the kidneys, restoring hemo- and urodynamics, stimulating regenerative processes and reducing sclerotic changes in the interstitium of the kidneys.
N. A. Korovina, Doctor of Medical Sciences, Professor I. N. Zakharova, Doctor of Medical Sciences, Professor E. B. Mumladze Ali Ahmed al-Makramani RMAPO, Moscow
To the 100th anniversary of the birth of Professor P. L. Sukhinin
November 27, 2002 marks the 100th anniversary of the birth of Professor Pavel Leonidovich Sukhinin.
Pavel Leonidovich was born in Tula, in the family of a hereditary pediatrician L. G. Sukhinin, who for many years was the home doctor of L. N. Tolstoy’s younger children. The whole situation in the family contributed to the fact that L. G. Sukhinin’s older children followed in their father’s footsteps and became doctors.
In 1920, P. L. Sukhinin entered the medical faculty of Moscow University. In 1923, he had to interrupt his studies: the future doctor was arrested in connection with the Moscow Theosophical Group case. Fortunately, the arrest lasted relatively short, 5 months.
Pavel Leonidovich completed his interrupted studies in 1926 and was retained in the residency of Professor D. D. Pletnev, with whom he worked until 1938, the time of the tragic death of Professor Pletnev.
In 1932, Sukhinin was invited to the position of consultant-therapist at the Moscow Regional Institute of Obstetrics and Gynecology. More than 60 scientific publications by Sukhinin, the monograph “Endocarditis of the puerperal period,” as well as his doctoral dissertation “Septic endocarditis after abortion and childbirth,” are devoted to the problems of cardiovascular diseases in pregnant women and gynecological patients.
However, Pavel Leonidovich's main activity was still associated with the faculty therapy clinic of the 1st Moscow State Medical Institute, and during the Great Patriotic War - with the Central Military Hospital named after. N. N. Burdenko. In 1952, in connection with the arrest of the head of the clinic, Academician V.N. Vinogradov, Sukhinin submitted his resignation and went to work at the Kursk Medical Institute, where he created the Department of Hospital Therapy. However, after V.N. Vinogradov returned to the leadership of the clinic and department in 1953, Pavel Leonidovich returned to the 1st MOLGMI, without, however, leaving work in Kursk until 1955.
In 1955, Sukhinin became the head of the therapeutic clinic of the Institute of Emergency Medicine named after. Sklifosofsky. During this period, more than 18 candidates and doctors of medical sciences were trained within the clinic. In 1964, Sukhinin sought to open the first Center for Toxicological Emergency Care in the USSR and became its scientific director. In 1968, on the basis of the clinic, the Department of Hospital Therapy of the Third Medical Faculty of the Moscow State Medical Institute was created, the head of which Sukhinin remained until 1975. He died in 1983.
Pavel Leonidovich Sukhinin had to live in difficult times, but he invariably maintained compassion for patients, a sense of duty, independence of judgment, kindness and attention to students and employees.