Home | About us | Delivery | Advertisers | Login | Registration
Delivery on Sundays and holidays does not work!
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2022 Pharmacy 84.
Instructions for use DOPEGYT®
During treatment with drugs containing methyldopa, in rare cases, hemolytic anemia may develop. If symptoms indicating hemolytic anemia develop, it is necessary to determine the hematocrit and hemoglobin level. If anemia is confirmed, further studies should be performed to confirm hemolysis. If hemolytic anemia is confirmed, methyldopa should be discontinued immediately. After discontinuation of methyldopa, hemolytic anemia resolves rapidly with or without treatment with corticosteroids. However, in rare cases, deaths have been observed. If hemolytic anemia is caused by taking methyldopa, the patient should not continue to receive this drug.
Some patients taking methyldopa for a long period of time may experience a positive Coombs test. According to the literature, the incidence of a positive Coombs test may be 10-20% in patients receiving this drug. A positive Coombs test is rarely observed during the first 6 months of treatment. If it does not develop within 12 months, then its development is unlikely with further use of this drug. A positive Coombs test is dose-dependent and is unlikely to develop at doses less than 1 g/day. A positive Coombs test during treatment with methyldopa will become negative only a few weeks or months after discontinuation of the drug.
Before starting a course of treatment, as well as at 6 and 12 months of treatment with methyldopa, the number of blood cells should be examined and a direct Coombs test should be performed.
The mere presence of a previous positive Coombs test or its occurrence in a patient during treatment is not a contraindication to methyldopa therapy. If the Coombs test becomes positive during treatment with methyldopa, the presence of hemolytic anemia and the clinical significance of a positive Coombs test should be assessed.
Information about the presence of a positive Coombs test helps in the evaluation of cross-blood compatibility testing. If a blood transfusion is necessary in a patient receiving methyldopa, direct and indirect Coombs tests should be performed. In the absence of hemolytic anemia, only the direct Coombs test is usually positive. The direct Coombs test itself does not affect blood typing or crossmatching. If the indirect Coombs test is also positive, cross-matching may be difficult to assess. In such cases, consultation with a hematologist or transfusiologist is necessary.
During treatment, rare cases of leukopenia, granulocytopenia and thrombocytopenia are possible. Typically, the granulocyte count normalizes after discontinuation of methyldopa. Rare cases of reversible thrombocytopenia have also been reported.
Some patients experienced fever during the first three weeks of drug therapy, which was sometimes accompanied by eosinophilia or increased liver transaminases. In addition, taking methyldopa may be accompanied by the development of jaundice. Jaundice usually appears during the first two to three months of therapy. In some cases, cholestasis was confirmed against the background of jaundice. In very rare cases, patients have developed necrotizing hepatitis with a fatal outcome. Liver biopsies performed in several patients with liver dysfunction showed microscopic focal necrosis consistent with a hypersensitivity reaction.
Before starting treatment with methyldopa and during the first 6-12 weeks of treatment, as well as at any time with the development of fever of unknown etiology, liver function tests are recommended, as well as a qualitative and quantitative general blood test with leukemia.
If fever, changes in liver enzyme activity, or jaundice occur, treatment with methyldopa should be discontinued immediately. If this condition is caused by a hypersensitivity reaction, the increase in temperature and changes in laboratory parameters disappear after discontinuation of the drug. Such patients should not be further prescribed methyldopa.
Patients with a history of liver disease or dysfunction should use this drug with extreme caution.
Patients receiving methyldopa may require reduced anesthetic doses. If hypotension occurs during anesthesia, vasoconstrictor drugs can be administered to correct it. Adrenergic receptors remain sensitive while taking methyldopa (see Drug Interactions section).
Some patients may experience swelling or weight gain while taking methyldopa. In these conditions, diuretics should be prescribed. Treatment with methyldopa should not be continued if edema increases or symptoms of heart failure develop.
Methyldopa is eliminated by dialysis. Therefore, after this procedure, blood pressure in patients on hemodialysis may increase (see sections Dosage regimen and Pharmacokinetics).
In patients with severe bilateral damage to the cerebral vessels, involuntary choreoathetotic movements may occur in rare cases (see section Side effects). In this case, treatment should be discontinued.
Extreme caution is required when prescribing methyldopa to patients with hepatic porphyria or their close relatives.
Methyldopa may alter urinary uric acid test results using the phosphotungstic acid method, serum creatinine results using the alkaline picrate method, and colorimetric AST enzyme determinations. To date, there is no evidence that methyldopa altered the results of spectrophotometric determination of AST.
Because methyldopa fluoresces at the same wavelength as catecholamines, methyldopa may give pseudo-positive results and high concentrations of catecholamines may be found in urine, interfering with the diagnosis of pheochromocytoma. However, methyldopa does not affect the results of measurements of VMA (vanillyl mandelic acid) in urine.
In rare cases, urine may darken when exposed to air, which may be due to the breakdown of methyldopa and its metabolites.
Avoid drinking alcohol while taking methyldopa.
(see section Drug interactions).
Impact on the ability to drive vehicles and machinery
Methyldopa may have a sedative effect, which is usually transient and may occur either at the beginning of treatment or when the dose is increased. If patients develop symptoms indicating the development of sedation, they are prohibited from driving vehicles and performing work that requires concentration.
Dopegit 250 mg No. 50 tablet.
Instructions for medical use of the drug DOPEGITâ Trade name Dopegitâ International nonproprietary name Methyldopa Dosage form Tablets 250 mg Composition One tablet contains the active substance - methyldopa anhydrous 250 mg (equivalent to methyldopa sesquihydrate 282 mg), excipients: corn starch, ethylcellulose, talc, sodium starch glycolate (type A), stearic acid, magnesium stearate. Description White or grayish-white round flat tablets with a bevel, smooth on one side, engraved with DOPEGYT on the other side, odorless or almost odorless. Pharmacotherapeutic group Antihypertensive drugs. Central agonists. Methyldopa (levorotatory). ATC code C02A B01 Pharmacological properties Pharmacokinetics Absorption of methyldopa from the gastrointestinal tract is variable. After oral administration, bioavailability is 25%. Maximum plasma concentration is achieved after 2-3 hours. Binding to plasma proteins is less than 20%. The site of the main and intensive metabolism of methyldopa is the liver. The drug's active metabolite, alpha-methylnorepinephrine, originates from central adrenergic neurons. In addition, many other metabolites are known to be excreted in urine. Approximately 2/3 of methyldopa is excreted in the urine as methyldopa or sulfate conjugate, and the remaining amount is excreted unchanged in the feces. Removal is biphasic. With normal renal function, the half-life is 1.8 ± 0.2 hours. The active component of the drug is completely eliminated from the body within 36 hours. Methyldopa is eliminated during hemodialysis. Six-hour hemodialysis can remove 60% of the absorbed dose of methyldopa from the circulating blood, and peritoneal dialysis within 20-30 hours removes approximately 22-39%. Methyldopa crosses the placental barrier and is excreted into breast milk. The maximum reduction in blood pressure occurs 4 - 6 hours after taking one dose orally and lasts 12 - 24 hours. After repeated administration, the maximum hypotensive effect develops within 2 to 3 days. After discontinuation of the drug, blood pressure returns to its original level within 1 to 2 days. In renal failure, the elimination of methyldopa slows down in accordance with the degree of decline in renal function. In severe cases (without hemodialysis), the half-life of methyldopa is extended by 10 times. Pharmacodynamics The active substance of the drug, methyldopa, is a centrally acting antihypertensive agent. The mechanism of its action is currently still completely unknown. The active metabolite (α-methylnorepinephrine) formed in the central nervous system stimulates central inhibitory presynaptic α2-adrenoreceptors, reducing sympathetic tone; replaces endogenous dopamine in dopaminergic nerve endings as a false neurotransmitter; reduces plasma renin activity and reduces peripheral vascular resistance; inhibits the enzyme dopa decarboxylase, thereby reducing the synthesis of norepinephrine, dopamine, serotonin and the concentration of norepinephrine and adrenaline in tissues. Dopegit has no direct effect on cardiac function, does not reduce cardiac output, does not cause reflex tachycardia, and does not reduce glomerular filtration rate, renal blood flow, or filtered fraction. In some cases, the heart rate decreases. The drug reduces blood pressure when the patient is lying down or standing and only in rare cases causes orthostatic hypotension. Indications for use: arterial hypertension. Method of administration and dosage: Tablets for oral administration. The tablets can be taken before or after meals. The recommended starting dose is 250 mg 2-3 times a day for the first two days. The daily dose may then be increased or decreased, depending on the degree of blood pressure reduction, at two-day intervals. To reduce the severity of sedation, which is possible at the beginning of the course of treatment and when increasing the dose, first increase the evening dose. Maintenance dose - 500-2000 mg 2-4 times a day. If the drug is insufficiently effective at a dose of 2 g/day, it is recommended to use a combination with other antihypertensive drugs. After 1 to 3 months of treatment, tolerance may develop. Effective blood pressure control can be restored by adding a diuretic or increasing the dose of methyldopa. After discontinuation of Dopegyt, blood pressure returns to the initial level after 48 hours without the phenomenon of reverse effects. Dopegit can also be used in patients who are already taking other antihypertensive drugs, gradually withdrawing the previous drug. In such cases, the recommended starting dose is 500 mg per day. To achieve the desired therapeutic effect, the dose can be increased at intervals of at least two days. If Dopegit is used as an addition to existing antihypertensive therapy, it may be necessary to change the dose of the antihypertensive drug so that the transition to combination therapy occurs without complications. In elderly patients, the initial dose should be lower and not exceed 500 mg/day. If necessary, the dose can be gradually increased every 2 days to a maximum dose of 2 g/day, which cannot be exceeded. Syncope (loss of consciousness), which is more often observed in elderly patients, probably associated with the increased sensitivity of elderly patients and with a pronounced narrowing of the lumen of blood vessels, can be avoided by using lower doses. If renal function is impaired, reduced doses should be used. In case of mild renal failure (glomerular filtration rate GFR > 50 ml/min), an interval of 8 hours should be maintained between doses, in case of moderate renal failure (GFR = 10-50 ml/min) with an interval of 8-12 hours, and in case of severe renal failure (GFR < 10 ml/min) 12-24 hours. Since methyldopa is removed by hemodialysis, the patient should be given an additional dose of 250 mg after this procedure to avoid an increase in blood pressure. Children and adolescents under 18 years of age The recommended initial dose in children is 10 mg/kg body weight per day in 2 to 4 doses. If necessary, the daily dose can be gradually increased (up to 65 mg/kg body weight) at intervals of at least two days. The daily dose should not exceed 3000 mg. The dose of the drug and duration of treatment are determined by the doctor individually depending on the clinical condition of the patient. Side effects Very common (≥ 1/10) - positive Coombs test Rare (≥ 1/10,000 and <1/1000) - hemolytic anemia, leukopenia, granulocytopenia, thrombocytopenia Very rare (<1/10,000) - myocarditis, pericarditis - parkinsonism - increased angina - pancreatitis - hepatitis, liver necrosis Not known (frequency cannot be estimated from available data) - bone marrow suppression, positive test for antinuclear antibodies, LE cells, rheumatoid factor - hyperprolactinemia, gynecomastia, galactorrhea, amenorrhea - nightmares, usually unexpressed, transient psychosis or depression, decreased libido - peripheral paresis of the facial nerve, lethargy, involuntary choreoathetotic movements, symptoms of cerebrovascular insufficiency (possibly associated with hypotension), headache, sedation (usually transient), apathy, weakness, dizziness, paresthesia - congestive heart failure, sinus bradycardia, edema, weight gain. Edema and weight gain usually respond well to diuretics. If edema becomes more pronounced, as well as when symptoms of heart failure appear, treatment with the drug should be discontinued - increased sensitivity of the carotid sinus, orthostatic hypotension (a dose reduction is recommended) - nasal congestion - colitis, vomiting, inflammation of the salivary glands, soreness or blackening of the tongue, nausea , constipation, flatulence, dry mouth - cholestasis, jaundice, liver function test disorders - toxic epidermal necrolysis, eczema, lichenoid eruptions - impotence, ejaculation disorders - increased residual blood nitrogen Contraindications - hypersensitivity to the active or other components of the drug - liver dysfunction associated with previous use of methyldopa - active stage of liver disease (active hepatitis or active cirrhosis) - concomitant therapy with monoamine oxidase inhibitors - depression - pheochromocytoma - children under 18 years of age. Drug interactions Dopegit should not be used simultaneously with monoamine oxidase inhibitors. Concomitant use with the following drugs requires special caution: Drugs that reduce the hypotensive effect of Dopegit: - sympathomimetics - tricyclic antidepressants - phenothiazines (at the same time, an additive hypotensive effect is possible) - oral iron preparations (ferrous sulfate and gluconate/II) (may reduce the bioavailability of methyldopa) - non-steroidal anti-inflammatory drugs - estrogen drugs · Drugs that enhance the hypotensive effect of the drug Dopegit: - other antihypertensive drugs (summation of hypotensive effects is possible) - anesthetics Dopegit and the following drugs can change the effects of each other: - lithium preparations (possible development of lithium intoxication ) - levodopa (reduced antiparkinsonian effect and increased undesirable effect on the central nervous system) - ethanol and other drugs that depress the central nervous system (increased depression of the central nervous system) - anticoagulants (increased anticoagulant effect, risk of bleeding) - bromocriptine (possibly undesirable effect on concentration of prolactin) - haloperidol (possible impairment of cognitive functions - disorientation and confusion). Special instructions During treatment with drugs containing methyldopa, hemolytic anemia may develop in rare cases. If symptoms indicating hemolytic anemia develop, it is necessary to determine the hematocrit and hemoglobin level. If anemia is confirmed, further studies should be performed to confirm hemolysis. If hemolytic anemia is confirmed, methyldopa should be discontinued immediately. After discontinuation of the drug, hemolytic anemia quickly resolves without or with the help of corticosteroid treatment. In rare cases, fatalities have been observed. If hemolytic anemia is caused by taking methyldopa, the patient should not continue to receive this drug. In some patients, with long-term use of Dopegyt, a positive Coombs test may be observed. A positive Coombs test, according to the literature, can occur in 10 - 20% of patients receiving this drug. A positive Coombs test is rarely observed during the first 6 months of treatment. If it does not develop within 12 months, then its development is unlikely with further use of this drug. A positive Coombs test is dose-dependent and is unlikely to develop at doses less than 1 g/day. A positive Coombs test that developed during treatment with Dopegyt may become negative only a few weeks or months after discontinuation of the drug. Before starting the course of treatment, as well as at 6 and 12 months of treatment with Dopegyt, the number of blood cells should be examined and a direct Coombs test should be performed. The mere presence of a previous positive Coombs test or its occurrence in a patient during treatment is not a contraindication to Dopegyt therapy. If the Coombs test becomes positive during treatment with Dopegyt, the presence of hemolytic anemia and the degree of clinical significance of a positive Coombs test should be checked. Information about the presence of a positive Coombs test helps in the evaluation of cross-blood compatibility testing. If a blood transfusion is necessary in a patient receiving Dopegyt, direct and indirect Coombs tests should be performed. In the absence of hemolytic anemia, only the direct Coombs test is usually positive. The direct Coombs test itself does not affect blood typing or crossmatching. If the indirect Coombs test is also positive, consultation with a hematologist or transfusiologist is necessary. During treatment, rare cases of leukopenia, granulocytopenia and thrombocytopenia are possible. Typically, the granulocyte count normalizes after discontinuation of methyldopa. Thrombocytopenia is also reversible. In some cases, fever may occur, accompanied by eosinophilia and liver dysfunction. Jaundice may also develop with or without fever. These symptoms usually develop in the 2nd – 3rd month of treatment. In some cases, the symptoms were found to be due to cholestasis. Biopsies were taken from some patients with liver dysfunction. Histological examination revealed focal necrosis, characteristic of a hypersensitivity reaction. Before starting treatment with Dopegyt and during the first 6–12 weeks of treatment, as well as at any time with the development of fever of unknown etiology, tests to determine liver function, as well as qualitative and quantitative blood tests are recommended. Therefore, if fever, changes in the activity of liver enzymes or jaundice occur, the course of treatment with Dopegyt should be stopped immediately. If this condition is caused by a hypersensitivity reaction, the increase in temperature and changes in laboratory parameters disappear after discontinuation of the drug. Such patients should not be prescribed Dopegit in the future. This drug should be given with extreme caution to patients with a history of liver disease or impairment. Patients receiving Dopegyt may require reduced doses of anesthetics. If hypotension occurs during anesthesia, vasoconstrictor drugs can be administered to correct it. Adrenergic receptors remain sensitive when using methyldopa. Some patients may experience swelling or weight gain while taking Dopegyt; in these conditions, diuretics should be prescribed. Treatment with Dopegyt should not be continued if edema increases or symptoms of heart failure develop. Methyldopa is eliminated by dialysis. Therefore, after this procedure, blood pressure in patients on hemodialysis may increase. In rare cases, involuntary choreoathetotic movements may occur in patients with severe bilateral cerebral vascular disease. In this case, treatment should be discontinued. Extreme caution is required when prescribing Dopegyt to patients with hepatic porphyria or their close relatives. Dopegit can change the results of the analysis of uric acid in urine using the phosphotungstic acid method, the determination of serum creatinine by the alkaline picrate method, and the colorimetric determination of the AST enzyme. To date, there is no evidence that methyldopa changed the results of spectrophotometric determination of AST. Since methyldopa fluoresces at the same wavelength as catecholamines, the use of Dopegyt may give pseudo-positive results; high concentrations of catecholamines may be detected in the urine, which interferes with the diagnosis of pheochromocytoma. However, methyldopa does not affect the results of measurements of VMA (vanillyl mandelic acid) in urine. Drinking alcohol is not recommended during treatment. Pregnancy and lactation For arterial hypertension in pregnant women, the drug should be prescribed after careful medical supervision. Available data showed no evidence of harm to the fetus or newborn. The drug can be prescribed to pregnant women, women planning pregnancy and women who have the possibility of pregnancy, only in cases where the expected benefit of treatment outweighs the possible risk. Methyldopa passes through the placenta and is detected in the blood of the umbilical cord and in breast milk. Dopegit can be prescribed to nursing mothers only after careful comparison of the expected benefits of treatment and the possible risks. Features of the effect of the drug on the ability to drive a vehicle and potentially dangerous mechanisms Dopegit may have a sedative effect, which is usually transient and can be observed either at the beginning of treatment or when the dose is increased. If patients develop symptoms indicating the development of sedation, they are prohibited from driving a vehicle or performing work that requires concentration. Overdose Symptoms: severe arterial hypotension, bradycardia, drowsiness, weakness, dizziness, nausea, vomiting, intestinal atony, flatulence, constipation, diarrhea. Treatment: symptomatic treatment - gastric lavage, stimulation of vomiting (if the drug has been taken recently). After absorption of the drug, its excretion through the kidneys can be stimulated by administering fluids. Monitoring of heart rate, cardiac output and blood volume, electrolyte balance, bowel and renal function, and brain function is required. According to indications, sympathomimetics (for example, adrenaline) are prescribed. If a chronic overdose is suspected, the drug Dopegit should be discontinued. Release form and packaging 50 tablets are placed in brown glass bottles with polyethylene caps, with first-opening control and equipped with an accordion shock absorber. One bottle each along with instructions for medical use in the state and Russian languages in a cardboard pack. Storage conditions Store at a temperature not exceeding 25°C. Keep out of the reach of children! Shelf life: 5 years Do not use after expiration date. Conditions for dispensing from pharmacies By prescription 1106 BUDAPEST, st. Keresturi, 30-38 Hungary Phone: (36-1) 803-5555, fax: (36-1) 803-5529 Registration certificate owner JSC "EGIS Pharmaceutical Plant", Hungary Address of the organization accepting claims from consumers on the territory of the Republic of Kazakhstan quality of products (goods) Representative office in the Republic of Kazakhstan CJSC "EGIS Pharmaceutical Plant" 050060, Almaty, st. Zharokova 286 G tel: +, +, fax: + 7 (727) 247 61 41 e-mail
Arterial hypertension in pregnant women: diagnosis, management tactics and treatment approaches
Arterial hypertension (AH) occurs in 4–8% of pregnant women [6, 7, 8]. Hypertension includes a whole spectrum of different clinical and pathogenetic conditions: hypertension, symptomatic hypertension (renal, endocrine), preeclampsia. According to WHO, hypertensive syndrome is the second cause of maternal mortality after embolism [20, 31], accounting for 20–30% of cases in the structure of maternal mortality [1, 7]. Rates of perinatal mortality (30–100 0/00) and preterm birth (10–12%) in pregnant women with chronic hypertension significantly exceed the corresponding rates in pregnant women without hypertension [8]. Hypertension increases the risk of abruption of a normally located placenta and can cause cerebrovascular accidents, retinal detachment, eclampsia, and massive coagulopathic bleeding as a result of placental abruption [7, 20].
Until recently, hypertension was thought to occur relatively rarely in people under 30 years of age. However, in recent years, population surveys have revealed elevated blood pressure (BP) in 23.1% of people aged 17–29 years [2]. At the same time, the early appearance of hypertension is one of the factors responsible for the unfavorable prognosis of the disease in the future [9]. An important fact is that the frequency of identifying patients with hypertension based on visits is significantly lower than during mass surveys of the population. This is due to the fact that a significant proportion of people, mainly with early stages of the disease, feel well and do not visit a doctor. This, apparently, to a certain extent explains the fact that many women find out that they have high blood pressure only during pregnancy, which significantly complicates the diagnosis and treatment of such patients.
The physiological characteristics of the cardiovascular system, depending on the developing pregnancy, sometimes create a situation where it is difficult to distinguish physiological changes from pathological ones.
Hemodynamic changes during physiological pregnancy represent an adaptation to the coexistence of mother and fetus, they are reversible and are due to the following reasons [7, 10]:
- strengthening metabolic processes aimed at ensuring the normal functioning of the fetus;
- an increase in circulating blood volume (CBV);
- the appearance of an additional placental circulatory system;
- gradual increase in body weight of the pregnant woman;
- an increase in the size of the uterus and limited mobility of the diaphragm;
- increased intra-abdominal pressure;
- changes in the position of the heart in the chest;
- an increase in the blood levels of estrogens, progesterone, and prostaglandins E.
Physiological hypervolemia is one of the main mechanisms ensuring the maintenance of optimal microcirculation (oxygen transport) in the placenta and such vital organs of the mother as the heart, brain and kidneys. In addition, hypervolemia allows some pregnant women to lose up to 30–35% of their blood volume during labor without developing severe hypotension. Blood plasma volume in pregnant women increases from about the 10th week, then increases rapidly (until about the 34th week), after which the increase continues, but more slowly. The volume of erythrocytes increases at the same time, but to a lesser extent than the volume of plasma. Since the percentage increase in plasma volume exceeds the increase in red blood cell volume, so-called physiological anemia of pregnancy occurs, on the one hand, and hypervolemic dilution, leading to a decrease in blood viscosity, on the other.
By the time of birth, blood viscosity reaches normal levels.
Systemic blood pressure in healthy women changes slightly. During a normal pregnancy, systolic blood pressure (SBP) and diastolic blood pressure (DBP), as a rule, decrease in the second trimester by 5–15 mmHg. Art. The reasons for these changes are the formation of placental blood circulation during these periods of pregnancy and the vasodilating effect of a number of hormones, including progesterone and prostaglandins E, which cause a drop in total peripheral vascular resistance (TPVR).
During pregnancy, physiological tachycardia is observed. The heart rate (HR) reaches its maximum in the third trimester of pregnancy, when it is 15–20 beats/min higher than the heart rate of a non-pregnant woman. Thus, the normal heart rate in late pregnancy is 80–95 beats/min, and it is the same for both sleeping and waking women.
It is now known that cardiac output (CV) increases by approximately 1–1.5 L per minute mainly during the first 10 weeks of pregnancy and reaches an average of 6–7 L per minute by the end of the 20th week. Towards the end of pregnancy, MOS begins to decline.
During a physiologically proceeding pregnancy, a significant decrease in peripheral vascular resistance occurs, which is associated with the formation of the uterine circulatory system with low resistance, as well as with the vasodilating effect of estrogens and progesterone. A decrease in peripheral vascular resistance, as well as a decrease in blood viscosity, facilitates hemocirculation and reduces afterload on the heart.
Thus, the individual blood pressure level in pregnant women is determined by the interaction of the main factors:
- a decrease in peripheral vascular resistance and blood viscosity aimed at reducing blood pressure;
- an increase in BCC and MOS, aimed at increasing blood pressure.
If the balance between these groups of factors is disturbed, blood pressure in pregnant women ceases to be consistently normal.
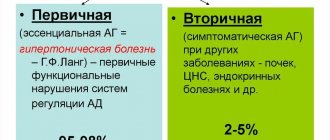
Classification of hypertension
Hypertension in pregnant women is a heterogeneous concept that unites various clinical and pathogenetic forms of hypertensive conditions in pregnant women.
Currently, the classification is a subject of debate, since there are no uniform criteria and classification signs of hypertension during pregnancy [4, 5], there is no single terminological base (for example, the term is used to denote the same process in Russia and many European countries gestosis, in the USA and Great Britain - preeclampsia, in Japan - toxemia).
More than 100 classifications of hypertensive conditions during pregnancy have been proposed. In particular, the International Classification of Diseases, 10th revision (ICD-10) combines all such pregnancy-related manifestations in the 2nd obstetric block. In Russia, all diseases are encrypted in accordance with this classification, although due to different terminology, encryption in accordance with ICD-10 causes disagreement among specialists.
The Working Group on High Blood Pressure in Pregnancy in 2000 developed a more concise classification of hypertensive conditions during pregnancy [20], which includes the following forms:
- chronic hypertension;
- preeclampsia - eclampsia;
- preeclampsia superimposed on chronic hypertension;
- gestational hypertension: a) transient hypertension in pregnant women (there is no gestosis at the time of birth and the pressure returns to normal by the 12th week after birth (retrospective diagnosis)); b) chronic hypertension (pressure rise after childbirth persists (retrospective diagnosis)).
Chronic hypertension refers to hypertension that was present before pregnancy or diagnosed before the 20th week of gestation. Hypertension is defined as a condition with a SBP equal to or higher than 140 mmHg. Art. and DBP - 90 mm Hg. Art. Hypertension that was first diagnosed during pregnancy but did not disappear after childbirth is also classified as chronic.
Pregnancy-specific preeclampsia syndrome usually occurs after the 20th week of gestation. It is determined by an increased level of blood pressure (gestational rise in blood pressure), accompanied by proteinuria. Gestational hypertension is defined as a SBP above 140 mmHg. Art. and DBP above 90 mm Hg. Art. in women who had normal blood pressure before the 20th week. In this case, proteinuria is considered to be a protein concentration in the urine of 0.3 g per day or higher when analyzing a daily urine sample. The dipstick method can be used to diagnose proteinuria. If it is used, two urine samples must be obtained 4 hours or more apart. For analysis, an average portion of urine or urine obtained through a catheter is used. The sample is considered positive if the amount of albumin in both samples reaches 1 g/l.
Previously, an increase in SBP by 30 and DBP by 15 mmHg. Art. It was recommended to consider it a diagnostic criterion, even if the absolute values of blood pressure are below 140/90 mm Hg. Art. Some authors do not consider this a sufficient criterion, since available data show that the number of adverse outcomes does not increase in women in this group. Nevertheless, most experts call for special attention to be paid to women in this group who have an increase in SBP by 30 and DBP by 15 mmHg. Art., especially in the presence of concomitant proteinuria and hyperuricemia [20].
Diagnostics
According to WHO recommendations, blood pressure should be measured after a 5-minute rest, in a sitting position, on both arms, using a cuff of the appropriate size.
The most common errors when measuring blood pressure include: measuring blood pressure once without prior rest, using an incorrectly sized cuff (“cuff” hyper- or hypotension) and rounding numbers. The measurement should be taken on both hands. The SBP value is determined by the first of two successive auscultatory tones. In the presence of an auscultatory failure, an underestimation of blood pressure may occur. The DBP value is determined by the V phase of Korotkoff sounds. Blood pressure should be measured with an accuracy of 2 mmHg. Art., which is achieved by slowly releasing air from the tonometer cuff. For different values, the true blood pressure is considered higher [4]. It is preferable to take measurements in pregnant women in a sitting position. In the supine position, due to compression of the inferior vena cava, blood pressure values may be distorted.
A single increase in blood pressure ≥ 140/90 mm Hg. Art. is registered in approximately 40–50% of women. It is obvious that a random single measurement of blood pressure to make a diagnosis of hypertension in pregnant women is clearly not enough. In addition, the phenomenon of so-called “white coat hypertension”, i.e. high blood pressure when measured in a medical environment (office blood pressure) in comparison with outpatient (home) measurement, is widely known. In approximately 30% of pregnant women with hypertension registered at a doctor's appointment, daily blood pressure monitoring (ABPM) resulted in normal average daily blood pressure [4]. The question of the prognostic significance of the phenomenon of “white coat hypertension” has not yet been finally resolved. Currently, most researchers believe that it reflects increased reactivity of the vascular wall, which, in turn, potentially increases the risk of cardiovascular disease. The role of ABPM in pregnant women has also not been fully determined. In addition to diagnosing “white coat hypertension” and assessing the effectiveness of therapy for established hypertension, this method can be used to predict the development of preeclampsia. BP usually decreases at night in patients with mild gestosis and chronic hypertension, but in severe gestosis the circadian rhythm of BP may be distorted, with a BP peak at 2 am [16].
However, given the complexity of the technology, the high cost of equipment, as well as the existence of other alternative methods for predicting preeclampsia, it can be considered that ABPM is not included in the group of mandatory (screening) methods for examining pregnant women with high blood pressure. However, it can be successfully used for individual indications.
Antihypertensive therapy for hypertension in pregnant women
Long-term use of antihypertensive drugs in pregnant women with chronic hypertension is a matter of controversy. A decrease in blood pressure may impair uteroplacental blood flow and compromise fetal development [16, 25, 30]. Over the past more than 30 years, seven international studies have been conducted that compared groups of women with mild chronic hypertension in pregnancy using different management regimens (with antihypertensive therapy and without pharmacological correction of hypertension) [11]. Treatment did not reduce the incidence of preeclampsia, preterm birth, placental abruption, or perinatal mortality compared with groups without treatment [20].
Some centers in the United States now maintain close monitoring of women with chronic hypertension who have stopped taking antihypertensive medications [32, 36]. In women with hypertension that has developed over several years, with damage to target organs, and taking large doses of antihypertensive drugs, therapy should be continued [25]. Reports on the experience of monitoring patients with severe chronic hypertension without adequate antihypertensive therapy in the first trimester describe fetal loss in 50% of cases and significant maternal mortality.
Experts from the Working Group on High Blood Pressure in Pregnancy, 2000, consider the following criteria for prescribing treatment: SBP - from 150 to 160 mm Hg. Art., DBP - from 100 to 110 mm Hg. Art. or the presence of target organ damage, such as left ventricular hypertrophy or renal failure [20]. There are other provisions on the criteria for starting antihypertensive therapy: with blood pressure more than 170/110 mm Hg. Art. [15, 24] (at higher blood pressure, the risk of placental abruption increases, regardless of the genesis of hypertension) [18]. There is an opinion that treatment of hypertension at lower values of initial blood pressure “removes” such a significant marker of gestosis as elevated blood pressure. At the same time, normal AH numbers give a picture of false well-being [14, 22]. European recommendations for the diagnosis and treatment of pregnant women with hypertension offer the following tactics for managing pregnant women with various types of hypertension [28].
- Pre-pregnancy hypertension without target organ damage - non-drug therapy for blood pressure 140–149/90–95 mm Hg. Art.
- Gestational hypertension that developed after 28 weeks of gestation - drug therapy at blood pressure 150/95 mm Hg. Art.
- Pre-pregnancy hypertension with target organ damage, pre-pregnancy hypertension with superimposed preeclampsia, pre-eclampsia, gestational hypertension that developed before the 28th week of pregnancy - drug therapy for blood pressure 140/90 mm Hg. Art.
Basic principles of drug therapy for pregnant women: proven effectiveness and proven safety [13].
In Russia there is no classification of drugs according to safety criteria for the fetus. It is possible to use the criteria of the American classification of medicinal and food products Food and Drug Administration (FDA–2002).
FDA classification criteria for drug safety for the fetus (2002):
A - studies in pregnant women have not revealed a risk to the fetus;
B - a risk to the fetus was detected in animals, but not in humans, or there is no risk in the experiment, but there is not enough research in humans;
C—Side effects have been identified in animals, but there is insufficient research in humans. The expected therapeutic effect of the drug may justify its use, despite the potential risk to the fetus;
D - a risk to the fetus has been proven in humans, but the expected benefit from its use for the expectant mother may exceed the potential risk to the fetus;
X is a drug that is dangerous to the fetus, and the negative effects of this drug on the fetus exceed the potential benefits for the expectant mother.
Despite the fact that the range of drugs used in the treatment of hypertension in pregnant women is quite wide (methyldopa, beta blockers, alpha blockers, calcium antagonists, myotropic antispasmodics, diuretics, clonidine), the choice of drug therapy for a pregnant woman is very responsible and complex a matter that requires strict consideration of all the pros and cons of this treatment [32].
Methyldopa
This drug is classified as Class B by the FDA. It is preferred as a first-line treatment by many clinicians based on reports of stability of uteroplacental blood flow and fetal hemodynamics, as well as 7.5 years of follow-up with a limited number of children experiencing no delayed adverse developmental effects following methyldopa administration during pregnancy. their mothers [27].
Benefits of Methyldopa:
- does not worsen uteroplacental blood flow and fetal hemodynamics;
- does not cause delayed adverse effects on the development of children after administration during pregnancy to their mothers;
- reduces perinatal mortality;
- safe for mother and fetus.
Disadvantages of Methyldopa:
- not recommended for use at 16–20 weeks (possible effect on dopamine content in the fetal nervous system);
- intolerance: 22% experience depression, sedation, orthostatic hypotension.
There have been no adequate and strictly controlled studies on other groups of antihypertensive drugs during pregnancy. Even when the results of studies are combined into a meta-analysis, there is no clear evidence of the effectiveness and safety of antihypertensive drugs in pregnancy.
β-blockers
Most of the published literature on antihypertensive therapy in pregnancy comes from studies of the effects of adrenergic blockers, including β-blockers and the α-β blocker labetalol. There is an opinion that β-blockers prescribed in early pregnancy, especially atenolol, can cause fetal growth restriction [19]. However, none of these drugs produced serious side effects; although in order to state this with complete confidence, long-term follow-up is not enough [24, 29].
The advantage of β-blockers is the gradual onset of the hypotensive effect, characterized by a decrease in the frequency of proteinuria, no effect on blood volume, absence of postural hypotension, and a decrease in the frequency of respiratory distress syndrome in the newborn.
The disadvantages of β-blockers are a decrease in the weight of the newborn and placenta due to increased vascular resistance when prescribed in early pregnancy.
In accordance with the FDA classification, atenolol, metoprolol, timolol oxprenolol, propranolol, labetolol belong to class C, pindolol, acebutolol - to class B.
Dadelszen in 2000 conducted a “fresh” meta-analysis of clinical trials on β-blockers and came to very interesting conclusions. Intrauterine growth retardation is not due to the effect of β-blockers, but to a decrease in blood pressure as a result of antihypertensive therapy with any drug. All antihypertensive drugs equally reduced the risk of developing severe hypertension by 2 times compared with placebo. When comparing various antihypertensive drugs with each other, no advantages were found regarding the effect on end points (development of severe hypertension, maternal and perinatal mortality) [30].
α-blockers are used in the treatment of hypertension in pregnant women, but there have been no adequate and well-controlled studies in humans [21]. In limited, uncontrolled use of prazosin and a β-blocker in 44 pregnant women, no adverse effects were observed. The use of prazosin in the third trimester in 8 women with hypertension did not reveal clinical complications after 6–30 months, the children developed normally [3].
The advantages of this group of drugs are as follows:
- effective reduction of blood pressure (used in combination with β-blockers);
- do not affect the bcc;
- absence of adverse effects (based on the results of clinical studies in a small number of women).
Flaws:
- a sharp decrease in blood pressure;
- possible orthostatic reactions;
- lack of adequate and strictly controlled studies in humans.
In accordance with the FDA classification, prazosin and terazosin belong to class C, doxazosin to class B. In our country, according to the instructions of the Pharmaceutical Committee of the Russian Federation, α-blockers are not used for hypertension in pregnant women.
Calcium antagonists. Experience with the use of calcium antagonists is limited to their use mainly in the third trimester of pregnancy. However, a multicenter prospective cohort study on the use of these drugs in the first trimester of pregnancy did not reveal teratogenicity [12]. A recent multicenter randomized trial of slow-release nifedipine in the second trimester found neither positive nor negative effects of the drug when compared with a no-treatment control group [23, 29].
Benefits of calcium antagonists:
- fetal weight in women taking nifedipine is higher than in women taking hydralazine;
- early use reduces the incidence of severe gestosis and other complications in the mother and fetus (however, in a number of studies using nifedipine in the second trimester, neither positive nor negative effects of the drug were detected when compared with a control group that did not receive treatment);
- absence (according to the results of clinical studies) of embryotoxicity in humans;
- antiplatelet effect;
- when used in the first trimester of pregnancy, there are no teratogenic effects (not detected in studies).
Disadvantages of calcium antagonists:
- embryotoxicity of calcium antagonists in animals;
- a rapid decrease in blood pressure can lead to a deterioration in uteroplacental blood flow (therefore, nifedipine is better taken orally than sublingually to relieve a hypertensive crisis in pregnant women);
- side effects: swelling of the legs, nausea, heaviness in the epigastrium, allergic reactions.
According to the FDA classification, nifedipine, amlodipine, felodipine, nifedipine SR, isradipine, diltiazem belong to class C.
Diuretics (hypothiazide 25–100 mg/day). Opinions regarding the use of diuretics during pregnancy are controversial. Doctors' concerns are mostly understandable. It is known that gestosis is associated with a decrease in plasma volume and the prognosis for the fetus is worse in women with chronic hypertension who have not experienced an increase in blood volume. Dehydration may impair uteroplacental circulation.
During treatment, electrolyte disturbances and increased uric acid levels may develop (which means this indicator cannot be used to determine the severity of gestosis) [17]. In women taking diuretics, from the beginning of pregnancy there is no increase in blood volume to normal values. For this reason, due to theoretical concerns, diuretics are not usually prescribed first. A meta-analysis of nine randomized trials involving more than 7000 subjects treated with diuretics found a trend towards a reduction in the development of edema and/or hypertension with a confirmed lack of increase in adverse fetal outcomes. Moreover, if their use is justified, they prove to be safe and effective agents that can significantly potentiate the effect of other antihypertensive drugs, and are not contraindicated during pregnancy, except in cases of decreased uteroplacental blood flow (preeclampsia and intrauterine growth retardation). A number of experts believe that pregnancy is not a contraindication for taking diuretics in women with essential hypertension that preceded conception or manifested before mid-pregnancy. However, there is insufficient data regarding the use of diuretics to lower blood pressure in pregnant women with hypertension.
In accordance with the FDA classification, hypothiazide belongs to class B. However, the instructions of the Pharmaceutical Committee of the Russian Federation state that hypothiazide is contraindicated in the first trimester of pregnancy; in the second and third trimesters it is prescribed according to strict indications.
Clonidine , a central α2-adrenergic agonist, has restrictions for use during pregnancy, and when taken in the postpartum period, breastfeeding should be avoided. The drug has no advantages over β-blockers. Sleep disorders have been identified in children whose mothers received clonidine during pregnancy. When used in early pregnancy, embryotoxicity was detected [4].
Myotropic antispasmodics are currently not used for routine therapy. They are prescribed only in emergency situations - during a hypertensive crisis [18]. Hydralazine (apressin) with long-term use can cause: headache, tachycardia, fluid retention, lupus-like syndrome. Diazoxide (hyperstat) with long-term treatment can cause sodium and water retention in the mother, hypoxia, hyperglycemia, hyperbilirubinemia, thrombocytopenia in the fetus. Sodium nitroprusside can cause cyanide intoxication with long-term use [16].
Angiotensin-converting enzyme (ACE) inhibitors are contraindicated during pregnancy due to the high risk of intrauterine growth retardation, the development of bone dysplasia with impaired ossification of the cranial vault, shortening of the limbs, oligohydramnios (oligohydramnios), neonatal renal failure (renal dysgenesis, acute renal failure in the fetus or newborn ), fetal death [20].
Although no data have been accumulated regarding the use of angiotensin II receptor antagonists, their adverse effects are likely to be similar to those of ACE inhibitors, so these drugs should also be avoided [16].
Treatment of acute severe hypertension in pregnant women
Some experts raise DBP to 105 mm Hg. Art. or higher is considered an indication for starting antihypertensive therapy [20], others consider it possible to abstain from antihypertensive therapy up to 110 mm Hg. Art. [15, 18]. There is evidence that if the initial diastolic blood pressure did not exceed 75 mm Hg. Art., treatment should begin when it rises to 100 mm Hg. Art. [16].
The range of drugs used in the treatment of acute severe hypertension in pregnancy includes hydralazine (start with 5 mg intravenously or 10 mg intramuscularly). If there is insufficient effectiveness, repeat after 20 minutes (from 5 to 10 mg depending on the reaction; when the desired blood pressure levels are achieved, repeat as necessary (usually after 3 hours); if there is no effect from the total dose of 20 mg intravenously or 30 mg intramuscularly, use another drug ); labetalol (start with a dose of 20 mg intravenously; if the effect is insufficient, prescribe 40 mg 10 minutes later and 80 mg every 10 minutes 2 more times, maximum dose - 220 mg; if the desired result is not achieved, prescribe another drug; do not use in women with asthma and heart failure); nifedipine (start with 10 mg per os and repeat after 30 minutes if necessary); sodium nitroprusside (rarely used when there is no effect from the above drugs and/or there are signs of hypertensive encephalopathy; start with 0.25 mg/kg/min to a maximum of 5 mg/kg/min; the effect of cyanide poisoning of the fetus may occur with therapy lasting more than 4 hours).
Sudden and severe hypotension may occur when any of these drugs are given, especially the short-acting nifedipine. The ultimate goal of lowering blood pressure in emergency situations should be its gradual normalization.
In the treatment of acute hypertension, the intravenous route of administration is safer than the oral or intramuscular route, since it is easier to prevent accidental hypotension by stopping the intravenous infusion than by stopping the intestinal or intramuscular absorption of drugs [20].
Of the above drugs for relieving hypertensive crisis in pregnant women, only nifedipine is currently registered with the Pharmaceutical Committee of the Russian Federation. However, the instructions for this drug indicate pregnancy as a contraindication to its use.
Thus, the problem of arterial hypertension in pregnant women is still far from being resolved and requires the combined efforts of obstetricians, clinical pharmacologists and cardiologists.
Literature
- Arias F. High-risk pregnancy and childbirth: trans. from English M.: Medicine. 1989. 654 p.
- Ardamatskaya T.N., Ivanova I.A., Bebeshko S.Ya. Prevalence and features of the course of arterial hypertension in young people. Modern aspects of arterial hypertension: materials of the All-Russian scientific conference. St. Petersburg, 1995. P. 28
- Information about medicines for healthcare professionals. Issue 2. Medicines acting on the cardiovascular system. USP DI. Russian edition /ed. M. D. Mashkovsky: trans. from English M.: RC "Pharmedinfo", 1997. 388 p.
- Kobalava Zh. D., Serebryannikova K. G. Arterial hypertension and associated disorders during pregnancy // Heart. 2002. No. 5. P. 244–250.
- Kobalava Zh. D. Modern problems of arterial hypertension. No. 3. 45 p.
- Savelyeva G. M. Obstetrics. M.: Medicine. 2000. P. 816.
- Serov V.N., Strizhakov A.N., Markin S.A. Practical obstetrics. M.: Medicine, 1989. P. 109.
- Serov V.N., Strizhakov A.N., Markin S.A. Guide to practical obstetrics. M.: OOO MIA, 1997. 436 p.
- Williams G. H., Braunwald E. Hypertension of vascular origin // Internal diseases / ed. E. Braunwald, K. J. Isselbacher, R. G. Petersdorf, etc.: trans. from English: in 10 volumes. M.: Medicine, 1995. T. 5. P. 384–417.
- Shekhtman M. M. Guide to extragenital pathology in pregnant women. M.: Triada, 1999. 815 p.
- Abalos E., Duley L., Steyn DW, Henderson-Smart DJ Antihypertensive drug therapy for mild to moderate hypertension during pregnancy (Cochrane Review)//In: The Cochrane Library, Issue 1, 2002.
- Bortolus R., Ricci E., Chatenoud L., Parazzini F. Nifedipine administered in pregnancy: effect on the development of children at 18 months // British Journal of Obstetrics and Gynaecology. 2000; 107:792–794.
- Bucher H., Guyatt G., Cook R., Hatala R., Cook D., Lang J., Hunt D. Effect of calcium supplementation on pregnancy-induced hypertension and preeclampsia: a meta-analysis of randomized controlled trials//JAMA . 1996, 275(14), 1113–1117.
- Butters L., Kennedy S., Rubin PC Atenolol in essential hypertension during pregnancy//BMJ. 1990; 301:587–589.
- Cunningham FG Common complications of pregnancy: hypertensive disorders in pregnancy//In: Cunningham FG, editor. Williams Obstetrics. Stamford, CT.: Appleton and Lange. 1997: 693–744.
- DeCherney A.H., Nathan L. A Lange medical book. Current Obstetric and Gynecologic Diagnosis and Treatment. 9th Edition. McGraw-Hill. 2003; 338.
- Duley L., Henderson-Smart DJ Reduced salt intake compared to normal dietary salt, or high intake, in pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 2, 2000.
- Duley L., Henderson-Smart DJ Drugs for rapid treatment of very high blood pressure during pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 1, 2000.
- Easterling TR, Brateng D., Schmucker B., Brown Z., Millard SP Prevention of preeclampsia: a randomized trial of atenolol in hyperdynamic patients before onset of hypertension // Obstet. Gynecol. 1999; 93:725–733.
- Gifford RW, August PA, Cunningham G. Working Group Report on High Blood Pressure in Pregnancy. July. 2000; 38.
- Hall DR, Odendaal HJ, Steyn DW, Smith M. Nifedipine or prazosin as a second agent to control early severe hypertension in pregnancy: a randomized controlled trial//BJOG. 2000; 107:6:759–765.
- Laupacis A., Sackett DL, Roberts RS As assessment of clinically useful measures of the consequences of treatment//N. Engl. J. Med. 1988; 318:1728–1733.
- Levin AC, Doering PL, Hatton RC Use of nifedipine in the hypertensive diseases of pregnancy. Annals of Pharmacotherapy Levin AC, Doering PL, Hatton RC Use of nifedipine in the hypertensive diseases of pregnancy//Annals of Pharmacotherapy. 1994; 28(12): 1371–1378.
- Magee LA, Duley L. Oral beta-blockers for mild to moderate hypertension during pregnancy (Cochrane Review)//In: The Cochrane Library/Issue 1, 2002.
- Mulrow CD, Chiquette E., Ferrer RL, Sibai BM, Stevens KR, Harris M., Montgomery KA, Stamm K. Management of chronic hypertension during pregnancy. Rockville, MD, USA: Agency for Healthcare Research and Quality. Evidence Report//Tech. 2000: 1–208.
- Ross-McGill H., Hewison J., Hirst J., Dowswell T., Holt A., Brunskill P., Thornton JG Antenatal home blood pressure monitoring: a pilot randomized controlled trial//BJOG. 2000; 107:2:217–221.
- Rudnicki M., Frolich A., Pilsgaard K., Nyrnberg L., Moller M., Sanchez M., Fischer-Rasmussen W. Comparison of magnesium and methyldopa for the control of blood pressure in pregnancies complicated with hypertension//Gynecologic & Obstetric Investigation. 2000; 49:4:231–235.
- The Task Force on the Management of Cardiovascular Diseases During Pregnancy on the European Society of Cardiology. Expert consensus document on management of cardiovascular diseases during pregnancy//Eur. Heart. J. 2003; 24: 761–781.
- Vermillion ST, Scardo JA, Newman RB, Chauhan SP A randomized, double-blind trial of oral nifedipine and intravenous labetalol in hypertensive emergencies of pregnancy//American Journal of Obstetrics & Gynecology. 1999; 181:4:858–861.
- Von Dadelszen P., Ornstein MP, Bull SB, Logan AG, Koren G., Magee LA Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis//The Lancet. 2000; 355:87–92.
- WHO international collaborative study of hypertensive disorders of pregnancy. Geographic variation in the incidence of hypertension in pregnancy//Am. J. Obstet. Gynecol. 1988; 158:80–83.
- Yeo S., Steele NM, Chang MC, Leclaire SM, Ronis DL, Hayashi R. Effect of exercise on blood pressure in pregnant women with a high risk of gestational hypertensive disorders // Journal of Reproductive Medicine. 2000; 45:4:293–298.
A. L. Vertkin, Doctor of Medical Sciences, Professor O. N. Tkacheva , Doctor of Medical Sciences, Professor L. E. Murashko, Doctor of Medical Sciences, Professor I. V. Tumbaev I. E. Mishina MGMSU, TsAGiP, IvSMA, Moscow , Ivanovo
Dopegyt®
In rare cases, hemolytic anemia has developed in patients taking methyldopa. If signs of anemia appear, it is necessary to determine the hemoglobin concentration and hematocrit. If anemia is confirmed, the degree of hemolysis should be further assessed. If hemolytic anemia develops, therapy with Dopegit® should be discontinued. After cessation of therapy (with or without corticosteroids), remission is usually achieved quickly. However, in rare cases, deaths have been observed. Taking Dopegit® is contraindicated in patients with hemolytic anemia that has developed during therapy with this drug.
In some patients taking the drug Dopegit® for a long time, a positive Coombs test is determined. According to reports from various researchers, the prevalence of this reaction varies from 10 to 20%. A positive Coombs test is rarely observed during the first six months of therapy. If this phenomenon does not develop during the first 12 months of therapy, then its detection in the future is unlikely. The prevalence of a positive Coombs test is dose-dependent. This phenomenon is most rarely observed in patients taking the drug at a dose of 1000 mg/day or less. The Coombs test, which is positive while taking methyldopa, becomes negative several weeks or months after stopping drug therapy.
Before starting treatment, as well as at 6 and 12 months of therapy, it is recommended to perform a general blood test and a direct Coombs test.
Detection of a positive Coombs test in the past or during ongoing therapy is not in itself a contraindication to taking the drug Dopegit®. In cases where a positive direct Coombs test is detected while taking the drug, it is necessary to exclude the presence of hemolytic anemia in the patient and determine the clinical significance of this phenomenon.
Knowledge of previous positive Coombs test results is helpful in assessing blood for crossmatch before transfusion. If, when treating a patient taking the drug Dopegit®, there is a need for a transfusion, then before blood transfusion it is necessary to perform both a direct and indirect Coombs test. In the absence of hemolytic anemia, only the direct Coombs test is usually positive. A positive direct Coombs test does not affect the determination of blood group and the result of the cross-match test. If the indirect Coombs test is also positive, then difficulties may arise in assessing cross-compatibility. In such cases, consultation with a hematologist or transfusiologist is necessary.
In rare cases, the development of reversible leukopenia and granulocytopenia has been observed during methyldopa therapy. After cessation of therapy, the granulocyte count returned to normal. In addition, rare cases of reversible thrombocytopenia have been reported in patients taking methyldopa.
Some patients experienced fever during the first three weeks of drug therapy, which was sometimes accompanied by eosinophilia or increased activity of liver transaminases. In addition, taking methyldopa may be accompanied by the development of jaundice. Jaundice usually appears during the first 2-3 months of therapy. In some cases, cholestasis was confirmed against the background of jaundice. Very rarely, patients have developed fatal necrotizing hepatitis. Liver biopsies performed in several patients with liver dysfunction showed microscopic focal necrosis consistent with drug hypersensitivity.
Before starting to take the drug Dopegit®, at 6 and 12 weeks of treatment, as well as at any time when an unexplained fever occurs, it is recommended to determine the activity of “liver” transaminases and a general blood test with leukemia.
If fever, jaundice or increased activity of “hepatic” transmiases occurs, taking Dopegit® should be stopped immediately. If the appearance of these signs is associated with hypersensitivity to methyldopa, then after discontinuation of the drug, the fever will disappear and liver function tests will return to normal values. It is not recommended to restart the drug in such patients.
Patients with a history of liver pathology should be treated with Dopegit® with extreme caution.
Patients taking Dopegit® may require a reduction in anesthetic doses. If hypotension develops during general anesthesia, it is recommended to use vasopressor therapy. Adrenergic receptors do not lose their sensitivity during methyldopa therapy.
Some patients taking methyldopa experience peripheral edema and weight gain. These side effects can be easily managed with diuretics. If edema increases and symptoms of heart failure appear, therapy with Dopegit® should be discontinued.
Since methyldopa is removed from the body through dialysis, you may experience an increase in blood pressure levels after the session is completed.
In patients with bilateral cerebral vascular disease (cerebrovascular disease), taking methyldopa may be accompanied by involuntary choreoathetotic movements. In such cases, drug therapy should be discontinued.
The drug Dopegit® must be used with great caution when treating patients with hepatic porphyria and their close relatives.
Therapy with Dopegit® may affect the results of measuring the concentration of uric acid (using a phosphorus-tungsten reagent), creatinine (using alkaline picrate) and aspartate aminotransferase (colorimetric method) in blood serum. The effect of methyldopa therapy on spectrophotometric analysis of aspartate aminotransferase concentrations has not been reported.
During methyldopa therapy, false-positive results may be obtained for determining the content of catecholamines in urine using the fluorescent method, which complicates the diagnosis of pheochromocytoma. At the same time, methyldopa has no effect on the assessment of the concentration of vanillylmandelic acid in the urine.
In rare cases, the urine of patients taking methyldopa may darken when exposed to air.
This effect is due to the degradation of methyldopa and its metabolites.
While taking Dopegit®, you should not drink alcoholic beverages.
Methyldopa
Due to the fact that cases of hemolytic anemia and severe liver damage, as well as positive Coombs tests, were observed when taking the drug, monitoring of liver function and peripheral blood patterns is necessary during treatment.
Before starting a course of treatment with methyldopa, the amount of blood cells, hemoglobin, and hematocrit should be examined, with their subsequent monitoring during therapy.
During the first 6-10 weeks of therapy, perform a direct Coombs test, which should then be repeated every six months or year. A positive Coombs test may occur in 10-20% of patients receiving this drug, especially after taking more than 1 g of methyldopa daily for six months to one year. Less than 5% of these patients may develop hemolytic anemia. In this case, you must immediately stop taking methyldopa. After discontinuation of the drug, hemolytic anemia should resolve. If this does not occur, the use of corticosteroids or analysis of other possible causes of hemolytic anemia is required. If hemolytic anemia is caused by taking methyldopa, the patient should not continue to receive this drug.
A positive Coombs test becomes negative several weeks or months after stopping the drug. The mere presence of a positive Coombs test or its occurrence in a patient is not a contraindication to methyldopa therapy. If the Coombs test becomes positive during treatment with methyldopa, the presence of hemolytic anemia and the clinical significance of a positive Coombs test should be assessed. For example, in addition to a positive direct Coombs test, a positive indirect Coombs test is less common, which can affect blood cross-compatibility. If a blood transfusion is necessary in a patient receiving methyldopa, direct and indirect Coombs tests should be performed. In the absence of hemolytic anemia, only the direct Coombs test is usually positive. The direct Coombs test itself does not affect blood typing or crossmatching. If the indirect Coombs test is also positive, consultation with a hematologist or transfusiologist is necessary.
During the first 6-12 weeks of treatment, as well as at any time when unexplained fever occurs, it is necessary to determine the activity of “liver” transaminases and the leukocyte formula. If there is a change in the activity of “liver” transaminases or the presence of jaundice, a hypersensitivity reaction should be assumed, in which cholestasis, liver cell damage or hepatitis is observed. In very rare cases, fatal liver necrosis can occur. Therefore, if the activity of “liver” transaminases changes or symptoms of liver failure occur, the course of treatment should be stopped immediately. Such patients should not be further prescribed methyldopa. If this condition is caused by a hypersensitivity reaction, then the increase in temperature and liver dysfunction disappear after discontinuation of the drug. Such patients should not be further prescribed methyldopa.
Patients with a history of liver disease or dysfunction should use this drug with extreme caution.
During treatment, very rare cases of leukopenia, granulocytopenia and thrombocytopenia are possible. They usually go away after methyldopa is discontinued.
Some patients may develop visible swelling or weight gain while taking methyldopa; in these conditions, diuretics should be prescribed. Treatment with methyldopa should not be continued if edema increases or symptoms of heart failure develop.
Methyldopa is eliminated during dialysis, so after this procedure blood pressure may increase (see “Method of administration and dosage”).
Patients receiving methyldopa should have their doses of general anesthetics reduced. If arterial hypotension occurs during general anesthesia, vasoconstrictors can be administered to correct it. Adrenergic receptors remain sensitive when taking methyldopa.
In rare cases, involuntary choreoathetoid movements may occur in patients with severe bilateral cerebral vascular disease. Stop using the drug if choreoathetoid movements occur in patients with cerebral atherosclerosis.
If there is hepatic porphyria in the patient's immediate family, methyldopa should be used with extreme caution.
When using the drug, a change in the color (darkening) of urine is possible.
Alcoholic beverages should be avoided while taking methyldopa.