Increased blood pressure can otherwise be called arterial hypertension.
Arterial hypertension occurs for a long time without obvious manifestations. However, soon enough it can lead to acute cerebrovascular accidents in the form of TIA (the so-called transient ischemic attack or, in other words, all manifestations of a stroke, but within 24 hours), strokes, as well as to hypertrophy of the walls of the heart and/or enlargement of cavities hearts.
In addition, arterial hypertension is a risk factor for the formation of atherosclerotic plaques in blood vessels and the occurrence of myocardial infarction.
The relationship between blood pressure levels and the risk of cardiovascular disease is linear.
The higher the blood pressure, the greater the likelihood of myocardial infarction, stroke, heart failure and kidney damage.
The prevalence of arterial hypertension (AH) in the Russian Federation is 39.3% among men and 41.1% among women, while blood pressure is properly controlled in only 17.5% of women and 5.7% of men.
Systolic blood pressure increases steadily with age, while diastolic blood pressure rises until age 60 in men and age 70 in women, after which it tends to decrease.
WHAT IS SYSTOLIC DIASTOLIC AND PULSE PRESSURE
Blood pressure is the pressure that blood exerts on the walls of the arteries.
There are:
- systolic pressure
- diastolic pressure
- pulse pressure
Systolic pressure (upper)
This is the maximum pressure in the arterial system developed during contraction of the left ventricle.
It is determined by the volume of blood that the heart pumps out in one contraction, as well as the elasticity of the aorta and large arteries.
Diastolic pressure (lower or heart)
This minimum pressure in the arteries during relaxation of the heart is determined by the amount of tone of the small arterioles.
Pulse pressure
This is the difference between systolic and diastolic blood pressure.
So the reasons for high blood pressure:
Causes
In approximately 90% of cases, the cause of a stable increase in blood pressure is hypertension. This diagnosis is made to the patient when no other diseases accompanied by hypertension are found during the examination. Among the latest:
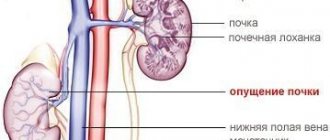
- kidney pathologies – pyelonephritis, glomerulonephritis, polycystic disease, diabetic nephropathy, renal artery stenosis;
- endocrine disorders - neoplasms of the adrenal glands, pancreas or pituitary gland, hyperfunction of the thyroid gland, Cushing's disease or syndrome, pheochromocytoma;
- obstructive sleep apnea syndrome;
- valve defects or atherosclerotic lesions of the aorta.
Regular use of some medications can also cause high blood pressure.
These include oral contraceptives, non-steroidal anti-inflammatory drugs, amphetamines, corticosteroids, drugs containing erythropoietin, cyclosporine, cocaine. The likelihood of developing cardiovascular diseases, including hypertension, is closely related to the following risk factors:
- unhealthy diet, including excess amounts of table salt, saturated fats and trans fats, lack of leafy greens, vegetables and fruits in the diet;
- obesity;
- pathologies of the heart and blood vessels in close relatives;
- age over 65 years;
- sedentary lifestyle;
- chronic stress;
- bad habits – smoking, excessive alcohol consumption.
Content:
- Why is hypertension dangerous?
- High blood pressure: causes
- Secondary hypertension
- Why does high blood pressure occur in a child?
- Brief conclusions
Hypertension is a leading risk factor for cardiovascular and cerebrovascular disorders. It is characterized by a persistent increase in blood pressure to 140/90 or more. It can occur at any age, but is more often diagnosed after 35-40 years. Found in 40% of people in the older age group. Of these, 58% are men, 42% of patients are women.
Treatment
With a moderate and low risk of cardiovascular complications, the patient is recommended only to change his or her lifestyle, adjust the diet, lose weight, increase physical activity and special exercises for hypertension, and give up bad habits while regularly measuring blood pressure.
Often these measures are enough to normalize blood pressure. A diet for hypertension involves limiting table salt, caffeine, hot, salty, smoked and spicy foods, high-fat foods, offal, confectionery with butter cream and alcoholic beverages. It is permissible to consume no more than 5 g of salt per day outside of an exacerbation of the disease. The recommended daily fluid intake is 1-1.2 liters.
In case of unsuccessful non-drug treatment for several months, as well as in case of a high risk of complications, they resort to antihypertensive therapy using medications for hypertension, the goal of which is to reduce blood pressure to less than 140/90 mm. Hg Art. For patients with diabetes or people already suffering from pathologies of the cardiovascular system, the target pressure level is even lower - 130/80 mm. Hg Art.
Modern drug treatment of hypertension includes a combination of two or more drugs from the following groups:
- calcium antagonists;
- angiotensin-converting enzyme inhibitors;
- angiotensin II blockers;
- diuretics (diuretics);
- b-blockers;
- alpha-blockers.
The vast majority of them are available in the form of tablets for hypertension.
Diagnostics
The main sign of hypertension is a stable increase in blood pressure, detected in at least three measurements on different days in a calm environment. When measuring blood pressure for the first time in a hospital or clinic, to ensure the correctness of the results obtained, it is important to follow the following rules:
- Before the examination, the patient needs to sit for a few minutes in a quiet room to calm down;
- the size of the tonometer cuff must correspond to the thickness of the arm, and the device itself must be mounted at the level of the heart;
- two measurements are performed with an interval of 1-2 minutes on each hand; if there is a large difference in the obtained figures, an additional measurement is taken;
- in elderly patients, as well as people suffering from diabetes mellitus, or if a decrease in blood pressure is suspected in case of a change in body position, measurements are taken in the first and fifth minutes in a standing position;
- Additionally, heart rate is measured for 30 seconds.
The doctor, in a conversation with the patient, clarifies at what age the pressure first began to increase, whether there are any symptoms such as snoring with pauses in breathing during sleep, attacks of muscle weakness or sudden heartbeat with sweating and headache, and unusual impurities in the urine.
It is also important to find out what medications and dietary supplements he is taking. As part of the first stage of examination for hypertension, the following tests are performed:
- clinical blood test;
- general urine analysis, detection of microalbumin in its single and daily portions;
- biochemical blood test (cholesterol, lipoprotein levels to assess the risk of atherosclerosis, blood electrolytes - potassium, sodium, chlorine, calcium, as well as glucose and creatinine);
- determination of the level of glycated hemoglobin;
- determination of the concentration of hormones - thyroxine, triiodothyronine and thyroid-stimulating hormone, antibodies to thyroid peroxidase and thyroglobulin, aldosterone.
If a hereditary predisposition to the disease is suspected, it is possible to determine polymorphisms of genes associated with the development of arterial hypertension.
In order to clarify risk factors for the development and identify existing cardiovascular pathologies in hypertension, instrumental diagnostic methods are used:
- 24-hour blood pressure monitoring;
- electrocardiographic study;
- echocardiography;
- 24-hour Holter monitoring;
- duplex scanning of the brachiocephalic, renal or iliofemoral arteries;
- ultrasound examination of the kidneys and adrenal glands;
- fundus examination.
For hypertension, it is important to monitor blood pressure at home by keeping a diary, in which it is necessary to record all the results of measurements over time, medications taken and episodes of stress that can provoke a rise in blood pressure. In this case, measurements must be taken in a sitting position, after several minutes of rest, keeping your hand at the same level as your heart.
On a note:
- Hypertension is a multifactorial disease that manifests itself as a persistent increase in blood pressure and depends on genetic predisposition and lifestyle.
- Men over 55 years of age and women over 65 years of age are at risk for the disease. However, the disease is also common among young people and children.
- Hypertension is a “silent killer” because it is often asymptomatic. To find out the presence of the disease, you need to regularly monitor your blood pressure levels and consult a specialist. Genetic testing will help determine predisposition and prevent the development of the disease.
- If your blood pressure suddenly increases, it is important to call a doctor or take medications recommended by a specialist. Self-medication with folk remedies for this condition is ineffective and even dangerous.
- Risk factors for high blood pressure: age, heredity, lack of physical activity, excess weight, smoking, alcohol, excess salt and lack of potassium, stress and chronic diseases.
- Hypertension negatively affects all areas of a person’s life. A hypotensive person must take medications regularly, limit diet and exercise. Headaches, cerebrovascular accidents, edema, increased risk of developing atherosclerosis, heart and kidney diseases are companions of arterial hypertension.
- Hypertension cannot be cured, but symptoms can be controlled with medications and its progression can be prevented with a balanced diet, regular exercise and stress reduction.
Sources:
- Oparil S. et al., Hypertension Review
- Williams B. et al.,2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH)
- Umemura S. et al.,The Japanese Society of Hypertension Guidelines for the Management of Hypertension
- Curfman G. et al., Treatment and Control of Hypertension in 2020: The Need for Substantial Improvement
- High blood pressure (hypertension)
- High blood pressure//Prevention//Causes//Diagnosis//Treatment
Classification
If it is possible to identify a disease that leads to an increase in blood pressure, arterial hypertension is called secondary or symptomatic.
When the cause is unknown, hypertension is considered to be primary hypertension. The latter has a staged course:
- Stage I. There are no obvious signs of disruption of the target organs affected by a stable increase in blood pressure - the heart, kidneys, arterial and venous vessels.
- Stage II. One of the listed signs or a combination of them is present, such as an enlargement of the left ventricle of the heart, a marked decrease in the filtration rate in the kidneys, albumin in the urine, an increase in the thickness of the walls of the carotid arteries or the appearance of atherosclerotic plaques in their lumen. In this case, clinical manifestations of the disease may be absent.
- Stage III hypertension. There is one or more pathologies associated with atherosclerotic processes in the heart and blood vessels - myocardial infarction, acute cerebrovascular accident, angina pectoris, atherosclerosis of the arteries of the lower extremities, or serious kidney damage, manifested by a pronounced decrease in filtration and/or significant loss of protein in the urine.
Arterial hypertension is divided into several degrees depending on the maximum measured blood pressure:
- First degree. Systolic blood pressure is from 140 to 159 mm. Hg Art. and/or diastolic – from 90 to 99 mm. Hg Art.
- Second degree. Systolic blood pressure from 160 to 179 mm. Hg Art. and/or diastolic – from 100 to 109 mm. Hg Art.
- Third degree. Systolic blood pressure is more than 180 mm. Hg Art. and/or diastolic over 110 mm. Hg Art.
There is also an isolated form of arterial hypertension, in which only the systolic pressure numbers are increased while the diastolic pressure is normal.
Genetic factors in the development of hypertension
Many genetic studies have revealed the stability of the renin-angiotensin-aldosterone system (RAAS). This is the human hormonal system that regulates blood pressure, blood volume, and the balance of fluids and salts in the body. Changes in this system may contribute to the development of hypertension.
But today there is data that shows a predisposition to the development of hypertension much more accurately and up-to-date. For example, genome-wide associations are worth considering. The NOS3 gene synthesizes nitric oxide and relaxes the walls of blood vessels, APOE is a cholesterol transporter, specific polymorphisms in the ADRB1 gene affect resting heart rate and may be associated with heart failure.
Increased upper pressure: causes, symptoms
Upper (systolic) pressure reflects the contractile activity of the myocardium during systole. Its increase may be due to various reasons:
- congenital defects and acquired cardiac pathology - coarctation of the aorta, PDA, blockade of the atrioventricular node, insufficiency of the valves at the entrance to the aorta;
- ion deviations - accumulation of sodium and calcium in the blood;
- atherosclerosis of large and small vessels;
- renal pathologies of an inflammatory, autoimmune nature;
- diabetes;
- dehydration of the body.
Over time, increased upper pressure first leads to hypertrophy, and then to wear and tear of the myocardium and the formation of heart failure. The aortic wall becomes rigid due to constant trauma by increasing blood pressure. Hemodynamic disturbances of internal organs are also noted due to inadequate distribution of blood through the vessels.
This type of hypertension is more often recorded in women. It manifests itself as regular headaches, discomfort in the heart, fatigue, memory impairment, tinnitus, and decreased vision.
Symptoms
Often, an increase in blood pressure is not accompanied by a deterioration in health and may go unnoticed by the patient, which is why it is so important to regularly measure blood pressure, especially for middle-aged and elderly people.
Manifestations of hypertension may include the following symptoms:
- headache, mainly in the morning after waking up;
- nosebleeds;
- hemorrhage under the mucous membrane of the eye;
- heart rhythm disturbance;
- blurred vision, flickering spots;
- tinnitus.
A sharp jump in blood pressure to high numbers, accompanied by a pronounced deterioration in well-being, is called a hypertensive crisis. Most often it occurs when systolic pressure rises to more than 180 mm Hg. Art. and/or diastolic over 120 mm Hg. Art. In this case, the patient experiences weakness, nausea, vomiting that does not bring relief, impaired consciousness, anxiety and fear, muscle tremors, and chest pain.
Ways to lower blood pressure permanently
In the initial stages of hypertension, the first step is to prescribe therapy with non-drug methods associated with changing the patient’s lifestyle:
- To give up smoking. Tobacco smoking is recognized as one of the main risk factors for the development of arterial hypertension. One cigarette smoked leads to a sharp increase in blood pressure and increased heart rate.
- Normalization of body weight. Numerous studies have proven that losing weight in overweight or obese patients leads to stabilization of blood pressure.
- Increasing physical activity. Regular dynamic physical exercises in the air for 50-40 minutes at least 4 times a week are recommended.
- Reducing salt intake to 5 g/day.
- Limit alcohol consumption.
- Compliance with the work and rest regime.
- Balanced diet. Increasing the proportion of plant foods and low-fat dairy products in the diet.
While blood pressure is slightly elevated, following the principles of a healthy lifestyle can stabilize blood pressure at a normal level with minimal drug support or even without drugs at all.
As the disease progresses, hypertension is treated using medications from various pharmacological groups to achieve a reduction in blood pressure to normal levels.
First aid at home for symptoms of high blood pressure:
- It is necessary to reassure the patient and create conditions for physical and emotional peace.
- Provide a flow of fresh air into the room.
- Breathing exercises help to quickly reduce pressure: take a deep breath, hold your breath for 10 seconds, exhale noisily through your mouth, then take short breaths in and out through your mouth for 2 minutes.
- Give the patient Corvalol to drink: dissolve 30 drops in 100 ml of water.
If attacks recur repeatedly, you should consult a doctor to find out the cause of the increase in pressure.