Alcoholic liver disease (ALD) is a complex of pathological changes in the liver, the development of which is caused by chronic alcohol consumption in toxic doses.
About 30% of all diffuse lesions of liver tissue are associated with ALD1. Long-term consumption of alcoholic beverages negatively affects all organs and systems, including the liver. The fact is that ethanol in the liver cells is metabolized into acetaldehyde, which has a toxic effect on the cells.9 It is worth noting that women, on average, have lower activity of the enzyme that produces acetaldehyde compared to men, which explains more severe ALD among women and the development of alcohol-induced liver damage in a shorter period of time and at lower doses of alcohol consumed1 (20 g/day for women compared with 30 g/day for men).10
Liver cirrhosis in Russia
In most developed countries, ALD is one of the most common diseases, diagnosed in 10-25% of men and slightly less frequently among women2. WHO (World Health Organization) studies have shown that liver cirrhosis in Russia ranks sixth among all causes of mortality2.
ALD could be called alcoholic fatty liver disease, which is associated with the development of fatty liver in the first stage of the disease with systematic consumption of ethanol in high doses.1 This phenomenon, the accumulation of fat in liver cells, also occurs in non-alcoholic fatty liver disease.
Data
· Alcohol damage occurs due to the toxic effects of alcohol on organ cells.
· The most common damage is fat accumulation. In some cases, cirrhosis and ascites develop.
· Up to a certain point, the damaged liver can recover if you stop drinking alcohol or reduce its amount.
· Cirrhosis is a serious chronic disease that has no cure. But its development can be slowed down by avoiding alcohol consumption and drug therapy.
· Treatment of alcohol-induced liver damage involves first stopping alcohol consumption.
Treatment methods for ALD
Drug and non-drug approaches to therapy can be distinguished.
Medication
Non-drug treatment requires complete abstinence from alcohol .
Medication
A drug for the treatment of alcoholic liver disease should have an antioxidant effect, suppress inflammation and prevent the progression of fibrosis. Such a drug is Phosphogliv*
, which has demonstrated all these effects in clinical studies. It should be taken 2 capsules 3 times a day with meals, without chewing, with a small amount of liquid. The course duration is usually 3 months.
If you suspect the development of liver disease, you should consult a doctor.
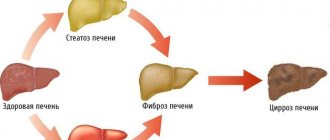
Dynamics of development of liver damage by alcohol
With systematic alcohol consumption, the patient's liver undergoes the following changes.
- At the first stage, inflammation of the liver forms - hepatitis.
- At the second stage, hepatitis turns into fatty hepatosis. At this stage, the penile cells are replaced by fat cells.
- Then the organ does not have time to form new healthy cells and connective tissue (similar to tendons) appears instead. This stage of liver damage is called cirrhosis.
- When the liver ceases to fully perform its functions, the disease ascites occurs. With it, water accumulates in the abdominal space. This condition is called hydrocele.
Hepatitis and alcoholic inflammation give the following symptoms:
· Bitterness in the mouth;
· Vomit;
· Bloating;
· In advanced stages, jaundice appears - yellowing of the skin and sclera.
Cirrhosis is a disease that has no cure. Due to irreversible changes in the cells of the organ, severe poisoning of the body occurs not only with alcohol derivatives, but also with other breakdown products formed in the human body. The brain suffers primarily from this.
Pathogenesis
The disease can develop over a long period of time: months and years. The pathological influence of viruses on liver cells, toxic substances (drugs, alcohol), impaired blood supply to the organ, immune mechanisms, and the influence of inflammatory mediators lead to massive death of hepatocytes and replacement with connective tissue. This process disrupts all vital functions of the liver.
- 1. Fatty degeneration. Initial changes in the structure and function of hepatocytes, which can completely disappear within a few weeks if the intake of alcohol in the body is stopped.
- 2. Steatohepatitis. An inflammatory process develops. The structure and size of hepatocytes change; in severe cases, the cells die, which affects the general condition of the liver. At this stage, disturbances in the functioning of the organ already occur, and specialized treatment is also required.
- 3. Cirrhosis. The formation of irreversible fibrous changes in the organ, disruption of the general structure: the appearance of tuberosity, reduction in size. If left untreated, the condition progresses and liver functionality decreases. Dangerous complications develop not only in the organ itself, but also in the structures dependent on it.
The sooner you consult a doctor and, most importantly, stop drinking alcohol, the higher your chances of getting rid of the problem.
Development of the syndrome
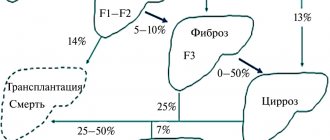
Almost everyone who drinks alcohol to excess is at risk for fatty liver disease, but only a small proportion of patients develop liver inflammation, and an even smaller percentage develop cirrhosis.
At the initial stages, a liver damaged by alcohol does not produce pronounced symptoms, but over time it begins to bother the patient more and more.
A clear sign of liver failure is the presence of icteric symptoms. With it, the patient's skin and whites of the eyes turn yellow, and a bitter taste appears in the mouth.
The organ performs the function of purifying the blood. In cases of liver failure, increased amounts of toxins are distributed throughout the body. They have a harmful effect on the brain. Over time, this leads to a person acquiring brain diseases. This is called hepatic encephalopathy or liver brain failure.
Alcoholic fatty degeneration (AFD)
This pathology is the most common type of toxic damage to liver tissue. Early diagnosis of the disorder is difficult due to minor symptoms. Patients show virtually no complaints.
When interviewed by a doctor, they may report:
- Apathy, poor health, lethargy.
- Periodic feeling of fullness in the stomach even after eating a small amount of food.
- Bloating.
- The release of foul gases.
- Diarrhea.
When examining and palpating the liver, the doctor reveals:
- Organ enlargement.
- Rounded edge.
- Thick consistency.
- Increased sensitivity.
Laboratory diagnostics do not provide any data confirming the presence of pathology. Liver tests remain within normal limits, sometimes slightly beyond the limits. The only factor indicating the disease is the bromsulfophthalein test.
Pathology is detected using:
- Ultrasound data.
- Computer and magnetic resonance imaging.
- Punch biopsy. Pathomorphological examination reveals cells filled with drops of fat, deformation with a displacement to the periphery of the nucleus and formed elements (mitochondria and lysosomes).
AD is a reversible condition. If the patient begins to lead a sober lifestyle, the identified deviations will gradually go away and recovery will begin.
Symptoms of the disease
The damaged organ does not show pronounced symptoms . Problems are most often discovered by chance, during tests, or characteristic symptoms begin to appear in the advanced stages of alcoholism. Violations in the functioning of the organ manifest themselves in the form of:
- chronic fatigue,
- digestive problems,
- bloody vomiting,
- susceptibility to infections;
- mental disorders.
Alcoholic liver inflammation usually appears suddenly and has similar symptoms.
Diagnostics
The effect of alcohol on the liver gives such a pronounced and characteristic clinical picture that doctors usually have no problems identifying the form and stage of the disease.
The main role is given to:
- Survey and collection of complaints.
- The presence of long-term chronic alcoholism.
- Blood tests (described above).
- Detection of elevated bilirubin values.
- Detection of high levels of immunoglobulin A.
Modern diagnostics are based on obtaining the results of computer and microresonance tomography, ultrasound. These techniques allow you to find violations at the very beginning of the process. The data obtained are confirmed by radionuclide methods and biopsy.
Establishing diagnosis
The doctor determines the duration of alcohol use or the degree of alcoholism. Based on these data, the patient is prescribed a medical examination. Both general diagnostics and blood tests can determine the extent of liver damage. For this purpose the following is carried out:
- Lab tests.
- Histological studies.
- Ultrasound. To have a visual idea of the disease picture, an ultrasound examination of the liver is performed.
- Biopsy. To do this, the doctor removes a tissue sample using a needle.
- Magnetic resonance and computed tomography.
Treatment of alcoholism in Moscow
The drug treatment clinic “AlkoZdrav” provides professional treatment for alcohol addiction in Moscow. We use certified medications, resort to modern psychotherapeutic programs and are guided by the principles of an individual approach to each person. It is important to note that treatment at AlkoZdrav is carried out strictly anonymously.
Diagnostics
Diagnosis is the first link in the chain of treatment of liver pathologies. To determine the condition of the gland, it is necessary to take a general blood and urine test, undergo an ultrasound, and take markers (cytolysis, cholestasis). In severe cases, a biopsy is necessary. After a visual examination and medical history, the doctor determines the current diagnostic method.
Alcohol detoxification
The most common methods of detoxification from ethyl alcohol include:
- Placement of IVs to cleanse the bloodstream;
- Taking enterosorbents;
- Carrying out injections;
- Resorting to the help of specialized devices (plasmapheresis, UBOD, etc.).
Detoxification is necessary to remove waste and toxins from the body. The procedure must be carried out with the participation of medical personnel.
Drug therapy
Pharmacotherapy is carried out with the aim of accelerating detoxification processes, relieving symptoms of the disease and restoring the functions of organs and systems. The current group of drugs is determined only by a narcologist. Self-medication may lead to adverse reactions.
Alcohol rehabilitation
Rehabilitation in a specialized center is necessary to restore the body and psychological state of a person.
During the rehabilitation process, the clinic resident undergoes intensive individual and group psychotherapy and struggles with psychological dependence on psychoactive substances. Together with a specialist, a person works through psychological problems, learns the principles of social adaptation, shows an active social position, and learns to live in sobriety.
Causes of alcoholic liver damage
Alcohol affects the metabolism of organ cells. This causes fat (fat cells) to accumulate. In some cases, this causes inflammatory reactions in the liver, leading to the formation of scar or connective tissue.
If exposure (irritation) occurs over a long period of time, the connective tissue contracts and destroys the liver structure. Thus, individual liver cells will not function normally and blood will have difficulty flowing through the organ. This causes the blood to seek other routes, such as through the esophagus. So, as a result of liver disease, varicose veins can appear.
Alcoholic hepatitis: modern diagnostic and treatment algorithms
For citation. Kostyukevich O.I. Alcoholic hepatitis: modern algorithms for diagnosis and treatment // Breast Cancer. 2016. No. 3. pp. 177–182.
The problem of alcoholic liver damage (ALD) still remains relevant. Alcohol consumption remains at extremely high levels everywhere. According to the latest data, in our country the average annual consumption of ethanol is 15.7 liters per capita. Alcohol is the main cause of PP and makes a significant contribution to the genesis of overall morbidity and mortality [1]. Alcoholic liver disease (ALD) includes a whole spectrum of pathologies, ranging from fatty hepatosis to liver cirrhosis. Timely diagnosis of ALD is extremely important in clinical practice, since early abstinence can significantly slow down the progression of fibrosis and the development of serious complications, and in some cases lead to recovery. At the same time, a practicing physician is well aware that collecting an alcohol history sometimes turns into a real medical detective story. In many cases, patients either downplay or completely deny alcohol use, leading the “investigation” down the wrong trail. And sometimes we ourselves, out of “pity” for the patient, when formulating a diagnosis, replace the term “alcoholic” with “food” or “cryptogenic”, misleading our colleagues. Now there is a fairly large range of objective and laboratory markers of chronic alcohol intoxication (CAI), special questionnaires and scales that allow one to assess the true contribution of alcohol to the genesis of PP and damage to other organs. Their introduction into clinical practice allows the definition of “alcoholic” to be used much more widely in the diagnosis, even if the patient initially denies the fact of alcohol abuse. The gold standard for diagnosing ALD is still liver biopsy, although in real practice we resort to it in extreme cases of a questionable diagnosis or to assess the degree of fibrosis. Today, non-invasive techniques such as elastography and various biochemical tests are increasingly used.
BPA forms
Alcoholic PP has three sequential stages-forms.
1. Steatosis
(fatty hepatosis) – present to one degree or another in 90% of patients who abuse alcohol (consuming ethanol more than 60 g/day) and is usually asymptomatic [2], revealing itself only during ultrasound examination.
The main symptom is hepatomegaly with normal transaminases. 2. Alcoholic hepatitis
(AH) – the stage of accumulation of cytokines, damage to hepatocyte membranes with prolonged alcohol consumption.
Morphologically, this stage is characterized by inflammatory infiltration, degeneration of hepatocytes, the presence of alcoholic hyaline (Mallory bodies), collagenosis of the space of Disse, and, less commonly, the presence of stepwise necrosis. There are acute and chronic hypertension. • Acute hypertension often develops after prolonged use of high doses of ethanol; it can develop at any stage of ALD - both against the background of steatosis and against the background of existing cirrhosis of the liver, which significantly worsens the prognosis. Severe hypertension is characterized by extremely high mortality, reaching 50%. • Chronic hypertension is diagnosed in patients with mildly expressed cytolytic and immunoinflammatory syndrome, in the absence of signs of cirrhotic transformation. 3. Liver cirrhosis
– develops with long-term (more than 10 years) consumption of “dangerous” doses of alcohol (in terms of ethanol: 60–80 g/day for men and 20 g/day for women) in 20–40% of cases [3] .
It has been shown that sensitivity to the hepatotoxic effects of ethanol is influenced by a number of factors and ALD does not develop in all “chronically abusing” patients. Risk factors for ALD:
• high doses of ethanol;
• genetic predisposition; • female; • use of drugs metabolized in the liver; • viral hepatitis; • underweight or obesity. High doses of ethanol.
A distinctive feature of alcoholic PPs is their high dose dependence.
Recent studies have shown that the risk of developing ALD increases significantly when consuming more than 30 g of ethanol per day. Doses of more than 120–160 g/day are considered absolutely hepatotoxic. Moreover, daily consumption of even small doses of alcohol is more dangerous than periodic consumption of high doses, when the liver has the opportunity to regenerate. Genetic predisposition. It is a known fact that different nations differ in the degree of alcohol elimination by at least 3 times. This is explained by genetic polymorphism of enzyme systems (alcohol dehydrogenase, cytochrome P450 and aldehyde dehydrogenase). Female.
It has been proven that women are 2 times more sensitive to the toxic effects of alcohol, and they are more likely to develop cirrhosis of the liver.
The most likely reason for such differences is associated with different activities of the gastric fraction of alcohol dehydrogenase, which causes a greater load on the liver enzyme systems. Hepatotropic drugs.
It must be remembered that in people who abuse alcohol, many medications become hepatotoxic (paracetamol, acetylsalicylic acid, antituberculosis, antiretroviral drugs, antitumor and psychotropic drugs, etc.), and the risk of PP increases several times.
This phenomenon is explained by competitive metabolism in the liver with the participation of the cytochrome P450 system. Viral hepatitis.
When chronic hepatitis is combined with alcohol consumption, PP progresses noticeably faster and the risk of developing hepatocellular carcinoma increases.
Nutrition
. There is currently no doubt that general malnutrition or nutrient deficiencies in addition to alcohol dependence lead to greater PP. Alcohol supplies a large amount of energy (1 g of ethanol provides 7 kcal), but plastic substances are not supplied, which leads to the destruction of one’s own proteins and aggravates nutritional deficiency. Malnutrition and ethanol hepatotoxicity act as synergists.
Pathogenetic aspects of alcoholic liver damage
PP is based on several mechanisms.
1. Direct hepatotoxic effects of ethanol. A weakly polarized solvent, ethanol can dissolve phospholipids in the membranes of hepatocytes and mitochondria. It is damage to mitochondria that underlies fatty liver degeneration, since the latter lose the ability to metabolize triglycerides. 2. Toxic effect of acetaldehyde. Acetaldehyde is an extremely toxic substrate for hepatocytes. It accumulates in hepatocytes and leads to the destruction of plasma membranes by depolymerization of proteins and activation of lipid peroxidation (LPO) products. In addition, acetaldehyde activates cells, which leads to excess collagen production. This explains the development of liver fibrosis in CAI. 3. Retention of proteins and water in hepatocytes. Ethanol suppresses the secretion of newly synthesized proteins from hepatocytes, which leads to the accumulation of protein, and subsequently water - this leads, along with fatty degeneration, to the development of hepatomegaly. 4. Immune PP. It is immune mechanisms that can explain cases of progression of ALD, despite cessation of alcohol consumption. Clinical picture of hypertension
There are 4 main clinical forms of hypertension: latent, icteric, cholestatic and fulminant.
1. The latent form does not give an independent clinical picture and is diagnosed by a moderate increase in transaminases in a patient who abuses alcohol. There may be such nonspecific complaints as weakness, loss of appetite, unstable stool, dull pain in the right hypochondrium, etc. 2. The icteric form is the most common. Patients experience severe weakness, anorexia, dull pain in the right hypochondrium, nausea, vomiting, diarrhea, weight loss, jaundice, and half of the patients have fever. 3. The cholestatic form is characterized by a significant increase in gamma-glutamyl transpeptidase (GGTP) and alkaline phosphatase (ALP), accompanied by painful skin itching. Quite rarely, already at the stage of hepatitis, signs of transient portal hypertension with the development of ascites may appear. 4. Fulminant (severe) acute hypertension is characterized by increasing encephalopathy, severe jaundice, edematous-ascitic and hemorrhagic syndromes. The risk of developing fulminant hypertension occurs when taking hepatotoxic drugs (for example, paracetamol) simultaneously. Characterized by neutrophilic leukocytosis up to 15–25×109/l, increased ESR up to 30–50 mm/h. Bilirubin increases mainly due to the direct fraction. The level of transaminases increases 5–10 times. The activity of GGTP and alkaline phosphatase increases, and the concentration of immunoglobulin A (IgA) increases. Diagnostics of hypertension
Diagnosis of hypertension consists of 4 stages: 1) verification of PP (fact of hepatitis);
2) confirmation of the fact of alcohol abuse; 3) assessment of hepatitis severity and prognosis; 4) assessment of the degree of fibrosis. Assessment of the condition of the liver includes the determination of structural (ultrasound, CT and MRI of the abdominal cavity, liver biopsy) and functional (laboratory diagnostics, liver scintigraphy) changes. The main criteria for hepatitis are hepatomegaly and increased serum transaminases. Ultrasound, CT and MRI of the liver reveal hepatomegaly of varying severity; in the case of transient portal hypertension, ascites and splenomegaly can be verified. Liver biopsy remains the gold standard for diagnosing hypertension. Indications for liver biopsy are the need for differential diagnosis between alcoholic and other PP, determining the stage of ALP, identifying perivenular fibrosis as a prognostically unfavorable factor in the transition of the disease to cirrhosis in people who continue to abuse alcohol. To date, the accuracy of the diagnosis of alcoholic steatohepatitis can only be confirmed by liver biopsy (grade 1A recommendation). Morphological signs of acute hypertension are: • necrosis of hepatocytes; • inflammatory infiltration; • fatty and balloon degeneration; • alcoholic hyaline (Mallory bodies); • damage to the centrilobular region. Acute hypertension is characterized by signs of an acute inflammatory reaction: leukocytosis, accelerated erythrocyte sedimentation rate (ESR) (20–50 mm/h), increased C-reactive protein. In patients with hypertension, the following clinical and laboratory syndromes can be distinguished: 1) cytolysis syndrome - actually reflects the fact of damage to hepatocytes. It is characterized by an increase in transaminases: alanine aminotransferase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase. The degree of enzyme elevation generally correlates with the severity of hepatitis; 2) cholestasis syndrome – verified by at least a 3-fold increase in ALP and GGTP; 3) jaundice – increased bilirubin mainly due to the direct fraction; 4) hepatocellular failure syndrome - progresses in parallel with the severity of the disease, its markers are a decrease in albumin, prothrombin, and increasing encephalopathy; 5) portal hypertension – also occurs in acute hypertension and, as a rule, is reversible. The presence of persistent portal hypertension indicates possible cirrhotic liver damage. The next most important stage of diagnosis is
to determine the etiological factor of hepatitis. In all patients without exception, even with a history of alcohol abuse, it is mandatory to determine markers of viral hepatitis and carefully collect a drug history. The fact of ethanol consumption and the true doses of alcoholic beverages are often hidden by the patients themselves, which sometimes leads the attending physician down the wrong path and leads to a false diagnosis. Knowledge of the objective criteria for CAI helps not only in diagnosing ALD, but also many other somatic diseases.
Identification of CAI
I. There are several questionnaires that allow with high reliability not only to identify the fact of alcohol abuse, but also to take into account
the contribution of CAI to the genesis of somatic pathology.
1. CAGE questionnaire (Cut down, Annoyed, Guilty, Eye-opener) – consists of only 4 questions (Table 1).
2. AUDIT (Alcohol Use Disorders Identification Test) questionnaire – has international standardization and consists of 10 questions (Table 2).
II. To the objective criteria of CAI
include the so-called “alcohol stigmas”: vasodilatation of the face and nose, scleral injection, hypertrophy of the parotid glands, atrophy of the muscles of the shoulder girdle, bright telangiectasia, gynecomastia, Dupuytren’s contracture, testicular atrophy.
1. The PAS questionnaire (determining the severity of post-intoxication alcohol syndrome), which includes 35 questions, has great sensitivity for identifying CAI (Table 3). Positive answers to 15 or more questions suggest a high probability of systematic use of unsafe doses of alcohol-containing beverages [4]. 2. In order to identify the physical signs of CAI, the “LeGo Grid” is used [4] (Table 4). III. Laboratory signs of CAI.
Alcoholic hepatitis is characterized by an excess of AST activity over ALT by 1.5–2.0 times (de-Ritis coefficient), an increase in GGTP. The test for determining carbohydrate-deficient (desialized) transferrin in blood serum is highly sensitive and specific - a compound of transferrin with acetaldehyde, leading to the accumulation of iron in the liver and acetaldehyde-modified hemoglobin (Table 5).
Assessment of severity and prognostic criteria for hypertension
Various scales are used to assess the severity of hypertension and prognosis. The following are the most popular (Table 6):
1. Maddray index, or discriminant function (mDF) [5]. An indicator of more than 32 indicates severe hypertension and is characterized by a high risk of death during the current hospitalization (>50%). 2. MELD (Model for End-Stage Liver Disease) score, originally developed to determine the priority for liver transplantation. 3. Glasgow alcoholic hepatitis score (GAHS). With values greater than 9 points, 46% survive by day 28 [6]. 4. The Lille scale is used, as a rule, to assess the advisability of continuing treatment with corticosteroids, since the calculation uses laboratory parameters before and after a week of therapy. If the value is less than 0.45, patient survival is for 6 months. averages 25%.
Assessing the degree of fibrosis
There are invasive (liver biopsy) and non-invasive methods: fibrotest (determination of serum markers of fibrosis) and fibroscan, which have a fairly high sensitivity and specificity.
Treatment of hypertension
The choice of therapeutic tactics for the treatment of hypertension depends, first of all, on the severity of the disease.
Therefore, before starting therapy, it is necessary to assess the severity and prognosis of hepatitis (Maddray index). Rational approaches to the treatment of hypertension: 1) abstinence from alcohol; 2) nutritional support; 3) careful selection of candidates for a short course of corticosteroids; 4) prescribing pentoxifylline if it is impossible to take corticosteroids; 5) prescribing maintenance therapy for mild and moderate hypertension; 5) treatment of complications of hypertension (portal hypertension, hepatic encephalopathy, infectious complications). Quitting alcohol.
A mandatory condition for the treatment of any stage of ALD is abstinence.
Nutritional support.
It has been shown that nutritional deficiency is present to varying degrees in all patients with ALD.
In case of severe disturbances in nutritional status, the issue of nutritional support with specialized enteral nutritional mixtures is resolved. All patients are recommended to eat a diet with a daily calorie content of 2000–3000 kcal, with a protein content of at least 1 g per 1 kg of body weight. Limiting the amount of protein is introduced only in cases of hepatic encephalopathy; in this case, it is recommended to use branched chain amino acids. Increasing dietary protein intake helps reduce catabolic processes, normalize immune status and directly improve liver function. The diet should contain a sufficient amount of vitamins (especially group B, folic and lipoic acids) and microelements - zinc, selenium. It has been established that zinc deficiency (40% of patients with ALD) significantly increases the manifestations of hepatic encephalopathy. It is also known that alcohol dehydrogenase is a zinc-dependent enzyme, therefore, with zinc deficiency, its activity decreases. Glucocorticosteroids
A meta-analysis of 13 randomized trials conducted by Mathurin in 2002 showed that glucocorticoid therapy significantly improves survival in patients with severe acute hypertension. Today, corticosteroids are the first-line treatment for severe hypertension with a Maddrey index of more than 32 (level of evidence 1B) [7]. Prednisolone is prescribed orally 40 mg/day for up to 4 weeks. followed by rapid replacement by 5 mg/week; a prerequisite is a normal creatinine level. If there is no decrease in bilirubin within 7 days (Lille scale score - 0.45), GCS is discontinued (level of evidence 1B). If there are contraindications to the administration of GCS, it is advisable to prescribe pentoxifylline (1B) 1200 mg/day per os or 400–600 mg/day intravenously. Pentoxifylline therapy has less evidence base and is used only when GCS therapy is impossible.
Maintenance therapy for mild to moderate hypertension
Hepatoprotectors
Traditionally, hepatoprotectors include a fairly wide range of drugs that differ in their mechanism of action and have a selective protective effect on liver cells. Based on their origin, hepatoprotectors can be divided into several groups [8]: • plant polyphenols (extract of milk thistle fruits, a combination preparation containing extract of fumitory and milk thistle extract, etc.); • synthetic drugs (morpholinium methyl triazolyl thioacetate); • phospholipid preparations; • organopreparations (hydrolyzed liver extract with a standardized amount of cyanocobalamin, etc.). Unfortunately, many of these drugs have not yet been proven effective in large clinical trials. 1. Silymarin preparations. The mechanism of its action is associated with the suppression of lipid peroxidation and collagen synthesis by Ito cells (antifibrotic effect). Silymarin is prescribed at a dose of 70–100 mg/day for a course of at least 3 months, often as part of combination therapy. 2. S-ademetionine. Its use in ALD is associated with the body’s need to replenish endogenous ademetionine, which performs one of the main functions in intermediate metabolism. Its prescription is especially justified in the presence of cholestasis syndrome (increased GGTP and alkaline phosphatase). Recommended doses of ademetionine are 800 mg/day for parenteral administration (for 2 weeks) and 1600 mg/day for oral administration (from 2 to 4–8 weeks). The disadvantage of the drug is its low bioavailability when administered orally (5%). 3. There are indications of an improvement in the clinical, biochemical and histological picture with the use of ursodeoxycholic acid in patients with ALD, which is likely due not only to its anticholestatic effect, but also to the suppression of the secretion of anti-inflammatory cytokines. 4. Essential phospholipids (EPL). The membrane-stabilizing and hepatoprotective effect of EPL is achieved by directly integrating molecules into the phospholipid structure of damaged hepatocytes, replacing defects and restoring the barrier function of the lipid bilayer of membranes. 5. Thiotriazoline (morpholinium methyl triazolyl thioacetate) has antioxidant and antihypoxic properties. Since oxidative stress plays a significant role in the pathogenesis of alcoholic hepatitis, the prescription of drugs that inhibit lipid peroxidation processes is pathogenetically justified [8]. Numerous studies have proven that in alcoholic hepatitis, a large number of reactive oxygen species are formed, such as hydroxyl radical (HO•), superoxide anion (O2•), singlet oxygen (1O2), etc. Free radicals promote the oxidation of lipids in hepatocyte membranes, which leads to the formation of pores and the release of enzymes and other cytoplasmic components through the damaged membrane. Thiotriazoline contains in its structure a thiol group, which is capable of accepting electrons from reactive oxygen species, while the sulfur in the thiol group passes from a divalent to a tetravalent state. The antioxidant effect of the drug is also manifested in the fact that it activates antioxidant enzymes - superoxide dismutase, catalase, glutathione peroxidase, and promotes more economical consumption of the endogenous antioxidant - -tocopherol [9]. There is also data indicating the inhibitory effect of Thiotriazolin on the processes of oxidative modification of proteins [10]. It has been shown that in patients with liver diseases, Thiotriazolin reduces the intensity of endogenous intoxication, reduces the severity of cytolysis, prevents the development of complications and reduces the length of patient stay in the hospital [11]. The selection of drug doses should be carried out differentially, taking into account the severity of cytolysis. For liver diseases, Thiotriazoline is administered intravenously in a slow stream or drip of 4 ml of a 2.5% solution in the first 5 days of the disease, or, if intravenous administration is not possible, intramuscularly 1-2 times a day. Maintenance therapy is carried out for up to 3 weeks. at the rate of 600 mg/day (1 tablet 200 mg 3 times a day). Currently, extensive experience has been accumulated in the clinical use of the drug not only for diseases of the gastrointestinal tract but also for cardiovascular and neurological diseases. Thiotriazolin combines well with other pharmacological agents, which allows its use in combination therapy. In conclusion, I would like to note that in order to solve the problem of alcoholic liver damage, timely diagnosis of “alcohol abuse” and chronic alcohol intoxication is first of all important. Patients themselves sometimes do not realize that they drink alcohol in subtoxic and toxic doses, denying the connection between the symptoms of “disease” and alcohol. It has been shown that 33% of patients visiting clinics abuse alcohol, and among those admitted to hospitals, their share increases to 60% [12]. In this regard, it is extremely important for any practicing doctor to be able to recognize the signs of CAI in a timely manner and explain to patients the true causes of their ailments. Indeed, in most cases, alcoholic hepatitis is preceded by a long stage of alcoholic hepatosis, which either was not recognized or remained without due attention. If hypertension has already developed and we have not been able to “prevent the disease,” today there is still a fairly wide arsenal of therapeutic agents for treating the patient. Here it is necessary to correctly assess the severity of the disease and possible risks in order to choose the optimal treatment tactics. It is important to remember that until the stage of cirrhosis, in many cases ALD is reversible, of course, subject to absolute abstinence.♦
Mechanism of treatment of the syndrome
The goal of treatment is to stop the further development of liver disease and stop necrosis of organ cells. The most important thing is that the patient completely stops drinking alcohol. Diet is also a significant factor in recovery. The patient needs to be provided with good nutrition with vitamin supplements and plenty of fluids.
Diuretics and antihypertensive drugs are also used in therapy. They lower liver blood pressure. If liver function is so poor that waste products such as ammonia are not eliminated naturally, they affect the brain and liver failure (hepatic encephalopathy) develops. Since ammonia is produced in the colon, its elimination can be increased with the help of laxatives. Cirrhosis is treated with antibiotics and protein-rich diets.
In cases of severe jaundice and alcoholic inflammation, they are treated with the adrenal cortical hormone - prednisole.
When to ask for help
If you or your family think there is a problem with alcohol, talk to your GP or consult a drug specialist . If you suspect that you have developed liver disease, you should inform your doctor and undergo the necessary examinations.
You need to contact a specialist in the following cases:
· Systematic consumption of alcohol for 1 year ( Alcoholism ).
· General malaise: drowsiness, chronic fatigue.
· Previous liver diseases.
· Presence of dyspeptic syndrome: morning sickness, indigestion, vomiting, change in stool.
· Tremor of the limbs.
· Sudden change in body weight (dystrophy or obesity).
· Enlarged parotid lymph nodes (Dupuytren's contracture).
· Signs of hypogonadism. In men, they manifest themselves as a slight expression of secondary sexual characteristics: testicular atrophy, gynecomastia, female type of hair growth.
· Pain in the hypochondrium, heaviness in the stomach.
Symptoms of the disease
ALD can be asymptomatic. However, symptoms of alcoholic liver damage may be nonspecific. These include complaints such as heaviness or pain in the right hypochondrium, bloating, abnormal stool, nausea, etc.
In addition to the liver, other organs and systems may be involved in the pathological process. In particular, there may be atrophy of the muscles of the shoulder girdle, impaired sensitivity in the extremities (polyneuropathy), heart disease (cardiomyopathy), and pancreas disease (pancreatitis).
How do liver diseases develop?
Fatty liver degeneration
If it is fatty liver, then stopping alcohol consumption will be enough to prevent further development of the disease. Over time, the number of fat cells will decrease and the symptoms of the disease will subside. The patient is prescribed a complete abolition of alcohol, special diet food and medications to restore organ cells.
Cirrhosis of the liver
Alcoholic cirrhosis of the liver is a dangerous and incurable disease with high mortality and a significantly reduced quality of life. Cirrhosis begins with fatty liver and, in the absence of timely treatment, leads to irreversible consequences and further death.
Cirrhosis develops into a chronic disease that progresses to ascites if alcohol consumption continues. This leads to a significant increase in mortality and a difficult life with the following symptoms.
· Chronic fatigue and constant lack of strength.
· Tendency to varicose veins in the esophagus. This phenomenon develops into bloody vomiting.
· Tendency to infections (decreased immunity).
· Mental disorders such as difficulty concentrating, bizarre behavior patterns, sleep disturbances, and depression often occur.
These complications significantly reduce life expectancy. In particularly advanced cases, the problem is solved by liver transplantation.
Alcohol liver inflammation
This disease occurs against the background of intensive alcohol for 1 or more years. Alcohol inflammation without cessation of alcohol consumption and lack of treatment leads the patient to death.
Causes, risk factors
The main reason for the development of ALD is alcohol abuse, but a direct relationship between the doses of regularly consumed alcoholic beverages and the occurrence of the disease, the degree of its progression and prognosis has not been established1,3. The main risk factors for the development of ALD are:
- Daily long-term consumption of alcohol in toxic doses: more than 30 g of ethanol for men10 (this is 75 g of vodka or 600 ml of beer), and for women - 20 g (about 200 ml of wine) per day1. The amount of alcohol allowed for daily consumption, regarded as a “safe dose,” varies: in European recommendations for the diagnosis and treatment of ALD10, for example, the “safe dose” for women is considered to be 12 g of ethanol per day and 24 g/day for men. The type of drink also influences: there is evidence that among consumers of red wine, the risk of developing alcoholic cirrhosis of the liver is lower than when drinking beer or spirits4. However, you should not take such news as a guide to action. In any case, alcohol is a factor of toxic damage, so you should be careful about drinking alcoholic beverages even in the smallest doses.
- Heredity. Predisposition to the development of alcoholic liver disease is explained by genetically determined differences in the functioning of enzyme systems responsible for neutralizing ethanol1.
- Ethnicity. Insufficient activity of the ethanol metabolizing enzyme occurs in 50% of the Asian population.1
- Overweight or obese. Is an independent risk factor for the development of ALD.1
- Alcohol dependence in people with viral hepatitis (especially B and C) is associated with more pronounced pathological changes in the organ, as well as a higher mortality rate compared to patients who do not suffer from viral hepatitis.1
- Autoimmune processes. Abnormal immune responses can cause further organ damage even after the effects of alcohol have stopped.1
Mechanism of development of ALD
Ethanol in the stomach and liver is oxidized to acetaldehyde, a very reactive compound that damages proteins and disrupts their functions, which in turn interferes with the normal function of liver cells and stimulates lipid peroxidation by free radicals.
This disrupts fat metabolism and the deposition of fat droplets in liver cells. The toxic effect of acetaldehyde also leads to damage to cell membranes and, ultimately, their death.1
Morbidity statistics
- Cellular obesity is a fairly common problem among the population of post-Soviet countries. The disease affects up to 10% of all Russian residents. This is primarily associated with excessive alcohol consumption, excess weight and high rates of diabetes.
- Alcoholic cirrhosis occurs with a probability of about 1000 new cases per year. For example, in Denmark about 12,000 people have this disease; in the Russian Federation this number is not precisely determined. It is known that incidence rates are several times higher than in European countries. The lack of accurate data on incidence is explained by the fact that many cases are diagnosed only after an autopsy of the deceased patient.
- Alcohol-related inflammation is a rarer disease and has fewer new cases per year than cirrhosis.