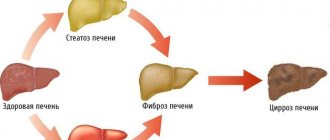
Fatty liver hepatosis (steatosis) is a primary or secondary pathological syndrome that occupies a leading position in the general structure of hepatopathologies. The main reason for the development of this condition is a metabolic disorder, leading to excessive accumulation of lipids and subsequent degeneration of hepatic parenchyma cells.
Causes of fatty hepatosis
There are three main reasons for the development of hepatic steatosis:
- Obesity. If the body mass index exceeds 30, the likelihood of dystrophy is about 40%.
- Drinking alcoholic beverages. Moreover, hepatosis can occur even in people who drink a little, but every day. There is a direct relationship between the duration of alcohol consumption and the severity of liver dystrophy and, as a consequence, the risk of developing cirrhosis.
- Long-term use of medications with hepatotoxic effects.
Less commonly, hepatosis develops against the background of diseases that occur with metabolic disorders; this category includes hyperlipidemia, hypercholesterolemia, diabetes mellitus, thyrotoxicosis, myxedema, Itsenko-Cushing syndrome, malignant neoplasms, chronic diseases of the gastrointestinal tract, in which the absorption process is disrupted, etc. .
Liver dystrophy can be caused not only by obesity, but also by poor nutrition - overeating, abuse of fatty foods and foods containing hydrogenated fats and simple carbohydrates.
The disease is sometimes diagnosed in people who have a deficiency of enzymes involved in lipid metabolism (hereditary disease).
Most often, more than one factor leads to the development of steatosis. In most cases, there is a multifactorial factor, for example, the consumption of alcohol by a person who is eating poorly or taking toxic medications.
Classification
Based on etiology, hepatosis is divided into non-alcoholic fatty liver disease and alcoholic steatosis. The first type of disease is diagnosed in only 7–10% of cases.
Hepatosis occurs:
- primary - caused by metabolic disorders, for example, obesity or hyperlipidemia;
- secondary – due to the impact on the body of external negative factors, which subsequently lead to metabolic disorders, for example, fasting, long-term use of corticosteroids, intestinal resection.
Doctors also take into account the characteristics of fat deposition, according to which hepatosis is divided into:
- diffuse;
- zonal;
- focal disseminated;
- pronounced disseminated.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Ultrasound of the abdominal organs (liver, gall bladder, pancreas, spleen) | 3 800 |
| Liver elastography (shear wave method) | 4 000 |
| MSCT of the abdominal cavity and retroperitoneal space of the abdomen | 6 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Symptoms of fatty liver disease
There are no specific signs of fatty liver hepatosis, even when there are already significant morphological changes. This is the insidiousness of the disease and lies a serious danger.
At the initial stage, the following nonspecific symptoms of fatty hepatosis may occur:
- general fatigue, asthenia, decreased ability to work;
- heaviness in the abdomen, stool instability, discomfort in the right hypochondrium, nausea, flatulence, sometimes vomiting;
- weight gain;
- causeless increase in body temperature for a long period of time;
- slight enlargement of the liver;
- skin itching.
As the disease progresses, icteric staining of the mucous membranes and skin is possible. Blood pressure often decreases and fainting occurs. There is a tendency to hemorrhages (increased bleeding).
There are 3 degrees of fatty hepatosis depending on the lesion:
- up to 33% – I degree;
- 33–66% – II degree;
- more than 66% – III degree.
How can we help you?
Examine . Ultrasound and elastography will show how much the liver tissue has changed, whether there is fibrosis, and the analyzes will make it clear whether there are disorders of fat and carbohydrate metabolism. If ultrasound results reveal fatty liver, the hepatologist will recommend testing for viral hepatitis. Viral hepatitis often occurs under the guise of fatty liver.
The liver does not hurt, fat accumulates unnoticed. Think about it before it's too late. Get examined and make sure everything is ok. And if a problem exists, do not close your eyes to it and seek help. We are ready to help.
Diagnostics
Diagnosis of the disease is difficult. Firstly, steatosis has no specific symptoms. Secondly, biochemical tests do not show significant changes. Sometimes the activity of serum transaminases increases, but this indicator does not change in all patients with steatosis. In this regard, differential diagnosis with hepatitis, biliary tract obstruction, primary hemochromatosis, and hepatocerebral dystrophy is of primary importance.
The doctor makes the final diagnosis based on a comprehensive examination and a series of tests, including ultrasound and biopsy.
To find out the cause of fatty hepatosis, the level of insulin in the blood, serum glucose concentration, hormonal status, antibodies to cytomegalovirus and hepatitis viruses, markers of autoimmune hepatitis, etc. are determined.
How to get rid of liver fat? 5 rules of behavior
Unfortunately, there is no “magic pill” for fatty liver disease. Only diet and physical activity. That's why:
- Limit animal fat - exclude butter, fatty meat, lard, smoked meats, remove the skin from poultry, switch to vegetable oils.
- Limit sweets and starchy foods, love vegetables - only “slow” carbohydrates, up to 100 g per day, instead of sugar - use substitutes, preferably stevia.
- Eat enough proteins, but less red meat - fish, poultry, low-fat cottage cheese, natural yogurt, eggs are best.
- Stop drinking alcohol or reduce the dose to a safe one.
- Exercise 3 times a week for 45 minutes. Every time you exercise, your insulin levels drop for 48 hours and your liver will gradually stop storing fat.
Treatment of fatty hepatosis
Treatment of fatty hepatosis is usually complex, including diet therapy, drug therapy and physical therapy.
Diet plays an important and sometimes paramount role in the treatment of steatosis. Sometimes, to cure the first stage, it is enough to follow a diet. Thanks to a significant limitation of fat consumption, healthy cells, and there are more than 66% of them, independently remove the fat present in the liver. But even in the later stages, nutritional correction is a prerequisite. It is recommended to steam food, eat more greens, vegetables and low-fat dairy products, eggs, cereals, and vegetarian dishes.
The cause of its occurrence directly affects how fatty hepatosis is treated.
Weight loss is a necessary condition for obese patients. As a rule, this helps to get rid of insulin resistance, which leads to normalization of carbohydrate and lipid metabolism. But there is one important nuance here - you should not lose weight too quickly (up to 600 g per week is allowed), otherwise there is a risk of progression of fatty hepatosis.
For alcoholic fatty degeneration, successful treatment is only possible with complete abstinence from alcohol. Patients are recommended to consult a narcologist.
Lipotropic drugs for fatty hepatosis are prescribed to accelerate the removal of fat from the liver. This category includes drugs that normalize cholesterol and lipid metabolism, promote fat oxidation and its mobilization from the liver: lipoic acid, essential phospholipids, folic acid, B vitamins.
To prevent the destruction of cell membranes and stimulate the regeneration of hepatocytes, hepatoprotective drugs are prescribed for fatty liver hepatosis: betaine, taurine, ursodeoxycholic acid, glutargin, phosphatidylcholine,
Tablets containing ursodeoxycholic acid often prescribed for fatty hepatosis: Livodexa, Grinterol, Urdoxa, Ursodez, Ursoliv, Ursofalk, Exchol, Ekurochol.
Thiazolidinediones and biguanides are used to eliminate insulin resistance.
The utilization of fatty acids is improved by physical exercise, so it is recommended for all patients with this disease.
Old and new approaches to the treatment of non-alcoholic fatty liver disease
Total duration: 16:20
00:00
Presenter: Now with great pleasure I present to everyone a well-known colleague, Professor Alexey Olegovich Bueverov, who will introduce us to modern approaches to the treatment of various forms of non-alcoholic fatty liver disease.
Alexey Olegovich Bueverov, Doctor of Medical Sciences:
— Dear Chairman, dear colleagues.
Non-alcoholic fatty liver disease today has already replaced such common liver pathologies as alcoholic liver disease and viral hepatitis in economically developed countries, taking first place in prevalence.
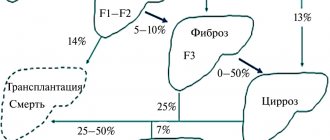
Indeed, the prevalence of non-alcoholic fatty liver disease in the general population reaches 20%. The likelihood of non-alcoholic steatohepatitis is significantly lower, but still this is not a small figure. In obese patients it reaches 75–100%. The frequency of non-alcoholic steatohepatitis is 25 – 75%.
If we take the population of patients with type 2 diabetes mellitus, non-alcoholic fatty liver disease occurs on average in 60% of cases. Recently, data were published showing that 6.3% of men and 2.6% of women (patients with type 2 diabetes mellitus) die from liver cirrhosis as a result of non-alcoholic steatohepatitis, and not from cardiovascular diseases, which are as the leading cause of death in such patients.
In 1998, two renowned researchers, Oliver James and Christopher Day, proposed a “two-hit” theory for the development of non-alcoholic fatty liver disease. The first blow is the development of steatosis, the second blow is the development of steatohepatitis.
Just recently, these same authors have been very skeptical about this theory. Clinical practice shows that in most patients, steatosis remains steatosis for the rest of their lives, without leading to the development of significant inflammation. With the development of steatohepatitis, steatosis and inflammation usually progress simultaneously. Perhaps in the near future the concept of “two strikes” will be replaced by the concept of “one strike”.
It is well known that adipose tissue cells - adipocytes - are biologically very active cells. They produce a huge number of different substances that affect a variety of parts of the life of the cell and various tissues. In particular, tumor necrosis factor α, a well-known pro-inflammatory, propathogenic cytokine, can lead to impaired phosphorylation of the insulin receptor.
As a result, disruption of a number of intracellular processes leads to a decrease in glucose entry into the cell due to a decrease in the activity of the glucose transporters GLUT-4. As a result, the development of insulin resistance, which underlies both non-alcoholic fatty liver disease and the initial stages of type 2 diabetes mellitus.
03:22
With obesity, adipose tissue cells not only increase in size, but also undergo apoptosis in greater numbers than normal. In addition, macrophages and other inflammatory cells are attracted to adipose tissue. As a result, a so-called cellular dialogue develops, which is carried out through the interaction of various cytokines with the corresponding receptors.
A well-known diagram demonstrating the effect of lipid peroxidation as a result of the formation of reactive oxygen species. It is typical for both non-alcoholic steatohepatitis and alcoholic steatohepatitis. We see almost identical changes in the histological specimen (death of hepatocytes by apaptosis and necrosis, formation of Mallory bodies, varying degrees of fibrosis (up to sarotic transformation) and infiltration of polymorphonuclear leukocytes (PMN) .
At the Immuno-thematic Conference of the European Association for the Study of the Liver, which took place in Bologna in September 2009, several reports were devoted to the question of which patients still need a liver biopsy.
Histological studies remain the gold standard in the diagnosis of non-alcoholic steatohepatitis. Considering millions of such patients, experts suggest primarily using this invasive method in motivated patients (patients with type 2 diabetes mellitus with android obesity and even a borderline platelet count, a high level of insulin resistance and any indirect signs of liver cirrhosis).
Non-invasive risk factors for the progression of non-alcoholic steatohepatitis include:
- older age (over 50 years old);
- presence of obesity;
- type 2 diabetes;
- arterial hypertension;
- hypertriglyceridemia;
- the ratio of aspartic transaminase to alanine is greater than one (according to some other data, more than 1.3);
- infection with the hepatitis C virus, which itself acts as an independent factor in the development of liver steatosis.
05:46
There are two known parts of the pathogenesis of non-alcoholic steatohepatitis: insulin resistance and oxidative stress. They dictate the theoretical possibility of using appropriate treatment methods. With regard to insulin resistance, this means following a hypoglycemic diet, prescribing the drug Orlistat (which will be discussed in more detail), physical activity and prescribing insulin sensitizers.
Regarding oxidative stress. These are primarily drugs of the antioxidant group, also possibly anti-cytokine drugs and drugs with hypolipidemic action.
As for weight loss, of course, it is indicated for all patients who are not only obese, but also overweight, not yet reaching the stage of obesity. Their approaches are well known. This is a low-calorie diet and physical activity.
Practically the only remaining approved drug in most countries is Orlistat. Finally, a patient with morbid obesity undergoes gastroplasty. Weight loss must be gradual. Very rapid weight loss can lead to a decrease in steatosis, but a simultaneous progression of inflammation primarily due to the release of free fatty acids and progression of liver fibrosis.
A meta-analysis of 29 liver studies with a follow-up period of at least 2 years demonstrated that intense physical activity leads to a significant reduction in body weight. They are significantly more effective than even a very low-calorie diet.
Another question is that such recommendations cannot practically be given to all patients. For example, a patient with a high cardiovascular risk, of course, should exercise in doses.
07:45
Interesting data have now been accumulated on long-term therapy of the drug Orlistat, well known under the name Xenical. "Xenical" is a drug that inhibits intestinal triglyceride lipase.
It is prescribed in a standard dose, regardless of body weight - 120 mg 3 times a day with meals or within one hour after meals (meals that contain a certain amount of fat). One-year, and even more so four-year treatment with Xenical significantly exceeds the effectiveness of weight loss using a hypocaloric diet. It turns out that long-term therapy with Xenical leads not only to a decrease in body weight, but also to an improvement in lipid status, a decrease in total cholesterol and the atherogenic fraction of low-density lipoprotein cholesterol.
Data published in the last 1.5 - 2 years indicate that the mechanism of action of Orlistat (perhaps even the key one) is the effect on adiponectin. A number of studies have shown that with a loss of more than 5% of body weight during treatment with Xenical, there is a significant increase in the level of serum adiponectin. With a loss of more than 9% of body weight, an increase in adiponectin clearly correlates with a decrease in the severity of steatosis, balloon degeneration and the activity index of non-alcoholic steatohepatitis according to puncture biopsy.
09:28
Studies were conducted directly with Orlistat for non-alcoholic steatohepatitis. Even a short six-month course of treatment with Xenical at a standard dose of 120 mg three times a day leads to a decrease in steatosis, a decrease in alanine transaminase levels, insulin resistance, cholesterol, triglycerides and low-density lipoprotein levels.
Another study (although it contained a small number of patients - only 14) demonstrated, along with an improvement in other histological parameters, also a decrease in fibrosis. Moreover, in three patients the decrease in fibrosis was two points compared to the baseline according to the paired biopsy.
Other drugs that increase insulin sensitivity are primarily represented by Metformin (an activator of adenosine monophosphate-dependent protein kinase) and thiazolidinediones, of which only Pioglitazone remains on the market.
Rosiglitazone has been withdrawn from the market in most countries due to an increased risk of cardiovascular complications. It should be remembered that these drugs can be prescribed to patients who do not have diabetes mellitus, since they extremely rarely cause glypoglycemia.
Studies with Metformin, in particular with the drug Glucophage, indicate that its administration leads to a decrease in the severity of steatosis and necroinflammatory activity. In the Bugianesi study, it reduced fibrosis. Metformin leads to normalization of alanine transaminase or a slight decrease in its level in patients who are not on a diet, and the effect of diet and the use of Ursodeoxycholic acid.
Another study demonstrated that a year's administration of Metformin leads to improvement in insulin resistance, normalization of glucose levels and normalization of adiponectin levels.
Another insulin sensitizer from a different group is Pioglitazone. There was a large study called Pivins, where Pioglitazone was compared with vitamin E 800 mg per day or placebo. It demonstrated greater reductions in steatosis and lobular inflammation compared with vitamin E or placebo. The dynamics of fibrosis in these patients was not reliable, despite the fact that the study lasted almost 2 years.
12:09
“Pentoxifylline” – an inhibitor of tumor necrosis factor synthesis? – has serious side effects when used in large doses. It is in these doses that it is used for non-alcoholic and alcoholic steatohepatitis, which significantly limits its use. Early studies demonstrated both biochemical and histological dynamics during the use of Pentoxifylline. More recent studies demonstrate a lack of histological effect, making the drug's prospects in patients with nonalcoholic steatohepatitis questionable, at least in the near future.
"Ursodeoxycholic acid." The most famous study here is “Ratzui”, which was published in 2009, demonstrating a statistically significant decrease in the levels of alanine and aspartic transaminases, as well as gamma-glutamyl transpeptidase.
However, the Leuschen study published last year only showed a reduction in lobular inflammation. However, the authors note that the best results from the use of Ursodeoxycholic acid were observed in men under 50 years of age with slight excess body weight and the presence of arterial hypertension.
"Adenosylmethionine." Here you can refer to domestic experience. This is a study by Professor A. Yu. Baranovsky from St. Petersburg. Unfortunately, it was carried out without a histological assessment of the liver. However, the use of Heptral for 6 months at a dose of 1200 mg per day led to normalization of transaminases in the vast majority of patients. The effect was achieved very quickly.
As an additional effect of using Adenosylmethionine, a decrease in serum cholesterol levels was noted during six-month therapy with this drug. This allows it to be considered as a promising drug for the treatment of patients with non-alcoholic fatty liver disease.
14:20
Data from a very large number of studies have been obtained on non-alcoholic fatty liver disease. The large number of these studies is due to the fact that this problem is extremely relevant, primarily in view of the wide prevalence of this nosological form.
What conclusion can be drawn about the most effective treatment method? Unfortunately, an unambiguous conclusion cannot be drawn today. Of course, these patients (especially those with signs of metabolic syndrome) are indicated for lifestyle modification, represented by diet and adequate physical activity.
Unfortunately, long-term maintenance is difficult, sometimes for objective, sometimes for subjective reasons. Medicines such as Orlistat, insulin sensitizers, Metformin and Pioglitazone, antioxidants, anti-cytokine and lipid-lowering drugs, which I did not dwell on. There are some studies that suggest that lipid-lowering drugs such as statins and fibrates may also be effective in treating non-alcoholic steatohepatitis in some patients.
The research results to date are contradictory. Studies on the effect of Orlistat (the drug Xenical) demonstrate that the drug helps not only to reduce and maintain body weight, but also in a number of studies to improve the biochemical and histological picture.
Thus, today we can conclude that patients with non-alcoholic fatty liver disease require a complex of therapeutic measures, taking into account the individual characteristics of the disease and comorbidity. Evaluating the effect of a particular drug or combination of drugs appears to require many years of research.
Thank you for your attention.
16:20
Fatty hepatosis of pregnant women
Separately, there is hepatic steatosis, which occurs without a significant cause in women bearing a child. Acute fatty hepatosis of pregnancy is diagnosed in one out of 13,000 women. 20–25% of cases end in death, according to foreign authors, and up to 60%, according to domestic sources.
The disease progresses quickly, over 2–3 weeks. Occurs mainly in late pregnancy - 32–36 weeks. The exact cause of this pathology has not yet been established.
Symptoms that may indicate acute fatty hepatosis in pregnant women: excessive vomiting, severe nervous disorders, general weakness, drowsiness.
The only treatment method is emergency delivery. Within 5 weeks after birth, the disease regresses.
Prevention
Preventive measures include:
- proper nutrition, in particular limiting fatty, spicy, fried and smoked foods;
- moderation in the consumption of alcoholic beverages;
- taking medications correctly;
- regular physical activity.
Fat accumulation is often caused by excess weight due to a sedentary lifestyle. Scientists have proven that if you eat only fast food for 4 weeks, this disease will almost certainly occur. Student volunteers took part in the experiment. Moreover, the first signs appeared after 1 week of such nutrition. Therefore, nutrition and weight control are of great importance.
For prevention, hepatoprotectors should be used, especially during periods of increased load on the liver, for example, with prolonged alcohol consumption, antibiotic treatment, and following a diet aimed at weight loss.
How to treat liver hepatosis
It is advisable to begin treatment of hepatosis at the first stage of stearosis, when irreversible processes in the liver have not yet occurred. Therapy involves adjusting the patient’s diet and lifestyle. A Mediterranean diet is prescribed, which consists of fish, vegetables, fruits, limit the consumption of fatty and fried foods, carbohydrates and sugary drinks.
Conservative treatment with medications includes phospholipid drugs; if necessary, anti-inflammatory drugs and antioxidants are prescribed.
Frequently asked questions about fatty liver disease
Which doctor should I contact?
A hepatologist specializes in liver diseases.
How to determine fatty hepatosis?
Unfortunately, the disease has no specific symptoms. A comprehensive examination allows you to identify deviations.
Can hepatic steatosis be cured?
With proper and timely therapy, changes in the liver are reversible. The main thing is to strictly follow all the doctor’s instructions, stick to your diet, and give up alcohol and “harmful” foods.
What kills a patient with untreated fatty liver: heart attack or cirrhosis?
Fatty liver disease, as fatty liver is also called, is combined with the deposition of fat on the walls of the arteries, and, as a result, accelerates the development of cardiovascular accidents. If fatty liver disease is not treated, it turns into fibrosis, when connective tissue, in other words, a scar, is formed instead of the “workhorses” - liver cells. This is how cirrhosis gradually develops. And these are the consequences of loving sweets, fatty foods, strict diets, “relaxing” with a glass of beer in hand or something stronger.
But the liver is an amazing organ, and the process can be reversed if we start paying attention to ourselves in time.