Classification
In world medical practice, there are several varieties of this tumor:
- cavernous hemangioma of the liver, which is several free cavities connected into a single one;
- capillary hemangioma of the liver forms a large number of small cavities, each of which houses a blood or venous vessel.
Along with the most common ones, venous, cluster-shaped hemangioma, and hemangioendothelioma can also occur.
Types of acquired red moles on the body
- Simple (capillary). Proliferation of newly formed capillaries, small venous and arterial vessels. Looks like a red spot.
- Cavernous. A spongy cavity with blood - a red or bluish nodule. Often forms under the skin.
- Branched (racellose). A plexus of tortuous dilated capillary trunks. They pulsate, noise and trembling are detected. It is rare and occurs on the extremities or face. If injured, life-threatening bleeding may occur.
How to identify hemangioma? Press on top of it and it should fade or disappear.
Symptoms of the disease
Symptoms of liver hemangioma do not appear immediately. Due to the small size of the formation, even in laboratory conditions it is not always possible to notice the presence of new cells. The same applies to clinical manifestations.
When the tumor grows to a size of 10 cm, features uncharacteristic of a healthy state can be detected:
- increase in liver volume;
- nausea, slight vomiting;
- unpleasant, painful sensations under the ribs on the right side.
All these symptoms arise as a result of the fact that the neoplasm puts pressure on neighboring organs and compresses nearby vessels.
In some cases, liver hemangioma may manifest itself after trauma to the abdomen (such as a strong blow) or intense physical exertion of the body. When it ruptures due to strain, it causes internal bleeding and acute pain in the abdominal area.
Are you experiencing symptoms of liver hemangioma?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Symptoms of liver hemangioma in adults
Most liver hemangiomas do not cause any unpleasant symptoms; they are discovered when the patient is examined for another disease.
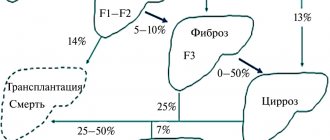
Small (a few millimeters to 2 cm in diameter) and medium-sized (2 to 5 cm) are not treated, but should be monitored regularly. Such monitoring is necessary because about 10% of hemangiomas increase in size over time for unknown reasons.
Giant liver hemangiomas (more than 10 cm) usually have symptoms and complications that require treatment. Symptoms most often include pain in the upper abdomen as the large mass presses on the surrounding tissue and liver capsule. Other symptoms include:
- poor appetite;
- nausea;
- vomiting;
- quick feeling of fullness while eating;
- feeling of bloating after eating.
Liver hemangioma may bleed or form blood clots that trap fluid. Then abdominal pain appears.
Reasons for appearance
Signs of liver hemangioma can be felt by absolutely everyone, regardless of age or gender. However, it is noted that in women it can grow more intensely due to increased levels of the hormone estrogen.
Despite the huge amount of research conducted on this formation, the exact cause of its appearance has not yet been identified. Medical scientists believe that the prerequisites are formed during the intrauterine period of fetal development.
There is an opinion that the proliferation of cells that subsequently form liver hemangioma is activated as a result of hemorrhages suffered by the body, as well as a tendency to enlarge capillary and venous vessels and thrombosis.
Should I be concerned if an MRI reveals a liver hemangioma?
You are a practically healthy person who has no pain. Taking care of your health, you decide to undergo a preventive ultrasound. “You need to get an MRI of your liver,” you hear after the study. The reason is a formation in the liver...
With questions about what liver hemangioma is and whether we should be afraid of it, as well as others, we turned to the radiologist at MRI Expert Lipetsk LLC, Alexander Konstantinovich Samaev.
- Alexander Konstantinovich, what is liver hemangioma and how often do you encounter this diagnosis in your practice?
This is a congenital vascular malformation, which is dilated venous vessels with slow blood flow. According to statistics, liver hemangioma occurs quite often - in approximately 7% of all people.
- Is liver hemangioma more often an incidental finding or are there symptoms that suggest the patient has this formation?
In most cases, this pathology is discovered by chance. Occasionally, a person may experience pain in the abdominal cavity, in the area of the right hypochondrium. However, there are no typical clinical signs of this disease.
- Liver hemangioma occurs only in adults or can it occur in children?
It is found in all age groups.
-What leads to the development of liver hemangioma?
This is a congenital disease. The reasons for its occurrence in adults, as well as in children, are not fully understood. There is a hypothesis about the role of hormones in the formation and growth of hemangiomas.
-What are the types of liver hemangiomas?
Based on the structure of these formations, capillary and cavernous varieties are distinguished. Based on size, hemangiomas are classified into small and large.
- Are there stages of development of liver hemangioma?
The classification of this disease does not describe stages.
-What is the danger of liver hemangioma? Is it possible for it to develop any complications?
This depends, among other things, on the size of the formation, its tendency to increase and its speed. Small hemangioma does not pose any immediate danger to humans.
If we are talking about a large hemangioma, then in certain situations there is a risk of its rupture with subsequent bleeding and the formation of a hematoma; thrombosis of the hemangioma and compression of surrounding organs are also possible.
Some authors point to the possibility of infection of a hemangioma thrombus, with the formation of an abscess, adhesions with intestinal loops and intestinal obstruction, as well as the possibility of torsion, in the presence of pedunculated hemangiomas, and the development of liver failure with multiple formations.
- Does any liver hemangioma require treatment? What size hemangiomas are safe?
Not every formation needs treatment. It is not entirely correct to talk about a safe size, since, as I noted earlier, not only the size of the hemangioma matters. According to some doctors, for liver hemangiomas larger than 5 cm and the patient has complaints, it is advisable to perform surgery. The issue of treatment (including surgery) is always decided on an individual basis.
-Can liver hemangioma disappear on its own?
Yes, in some cases this is possible - this phenomenon has been described, in particular, in childhood.
-Is it possible for hemangioma to become malignant?
Opinions are mixed; there are isolated reports of such a possibility.
- If there is a diagnosis, does it always require observation of the formation? Is MRI or CT indicated for liver hemangioma?
Yes, such a person needs to be observed in order to monitor the dynamics of the development of hemangioma. In addition, some other pathological liver formations can “masquerade” as hemangioma.
When it comes to choosing between magnetic resonance imaging and computed tomography, the first method is more often used. However, if there is no MRI machine, then it is also possible to detect hemangioma using CT.
- If MRI is used to diagnose liver hemangioma, is it performed with or without contrast?
With contrast agent. Moreover, CT is also indicated with contrast, since some important characteristics of hemangioma are revealed precisely with the introduction of contrast.
-If the pattern of liver hemangioma may be similar to other lesions, does this mean that it can be confused with metastases or liver cancer?
Yes it is possible. Therefore, it is so important to monitor this formation dynamically, at intervals determined by the doctor.
For reference:
Samaev Alexander Konstantinovich
Graduate of the medical faculty of the North Ossetian State Medical Academy in 2008.
In 2009, he completed an internship in the specialty “Radiology”.
Since 2013, he has been working as a radiologist at MRI Expert Lipetsk LLC.
Other interviews with Samaev A.K.:
Will an MRI show meningitis?
Diagnostics of education
In exceptionally extreme cases, only by chance, liver hemangioma in a child or adult can be detected at an early stage. In the vast majority of cases, it is found when the size reaches serious volumes.
The following diagnostic methods are used:
- Ultrasound of the gallbladder and liver (may show a round tumor with clear boundaries);
- MRI of the biliary tract and liver (in addition to the outlines of the formation, it will also show its contents);
- MSCT of the abdominal cavity (layer-by-layer will demonstrate the boundaries and contents of the tumor).
When a tumor is detected, it is necessary to determine its qualitative characteristics. To confirm hemangioma, angiography of the celiac trunk is performed; static liver scintigraphy may also be needed. To determine the degree of benignity (malignancy) of atypical cells, hepatoscintigraphy is prescribed.
Along with this, clinical tests are carried out:
- liver tests;
- complete blood count, blood biochemistry;
- blood test for genetic markers.
Diagnostic measures
Highly differentiated and poorly differentiated tumor
An effective diagnostic method is color Doppler mapping. This mode, in comparison with ultrasound, increases the ability to detect hemangioma.
Magnetic resonance imaging is also very informative.
The most effective method for diagnosing a tumor is considered to be computed tomography with intravenous contrast.
Features of treatment
The method of getting rid of a tumor largely depends on its size and shape.
Small tumors (up to 5-6 cm in volume) do not require special action. They are monitored and ultrasonic controlled after 3 months from the moment of detection. In the absence of any dynamics, ultrasound diagnostics are prescribed every 6-12 months.
The need for surgical removal is determined individually. This course of events leads to:
- rapid growth of liver hemangioma - more than 50% of the original size per year;
- volume more than 5-6 cm;
- bleeding of atypical tissue;
- aggressive manifestation of symptoms;
- inaccurate determination of the benignity of the tumor.
Modern methods of treatment
Some hemangiomas are diagnosed at birth or in early childhood (up to 5 - 10% of one-year-old children).
Hemangioma usually shrinks over time and in some cases may disappear. If it is small, stable and not causing any symptoms, it can be monitored with imaging studies every 6 to 12 months. There are no medications to treat liver hemangioma. Surgery may be necessary to remove the tumor if it is growing quickly or causing significant discomfort or pain. A technique called vascular embolization, in which the blood vessels supplying the hemangioma are closed, can slow or reverse its growth.
Nutrition
Nutrition for liver hemangioma plays a significant role in getting rid of it. The patient is required to be prescribed a diet so as not to provoke a worsening of the situation (sharp proliferation of atypical cells).
A diet for liver hemangioma in adults and children involves excluding from the diet such foods as:
- carbonated drinks;
- alcohol and low-alcohol drinks;
- any chocolate;
- egg yolks;
- hot spices;
- pears, melons;
- fresh bread.
You should limit your consumption of fatty, fried, smoked, and salty foods.
Instead, you need to focus on:
- low-fat fish;
- liver;
- dairy products;
- viscous porridge;
- vegetables;
- not sour fruits.
Vitamin B12 may be additionally prescribed.
Causes
Currently, the causes of liver hemangioma remain unknown. According to the international classification, a vascular neoplasm is considered a benign tumor. Some authors consider it a hamartoma, that is, a nodular tumor-like formation representing a developmental anomaly.
The theory of the hereditary origin of pathology has become widespread. An evidentiary example is a clinical case of a familial hemangioma, which developed in three women in three successive generations. However, genetic mechanisms of inheritance of vascular hemangioma have not been identified.
It is generally accepted that liver hemangioma begins to form during embryogenesis and is a developmental anomaly. In this regard, the neoplasm can be detected even in newborns. Localization of a vascular neoplasm in the liver is considered the most common. It leads among all benign tumors in the gland.
There are two theories about the origin of hemangioma:
- tumor, which is characterized by invasive growth, a high risk of relapse after surgical removal, as well as dependence on the level of steroids in the bloodstream;
- developmental defects. This theory is confirmed by the presence of many pathological foci within one organ, which is not typical for a tumor process.
Factors contributing to the progression of an existing tumor are considered to be the effects of endogenous hormones or steroid drugs.
Answers to common questions
What is the prevention for hemangiomas?
Since the exact cause of hemangioma has not been determined, a competent preventive measure is to conduct an ultrasound diagnosis of the liver once a year. If there is any doubt, an additional CT or MRI should be done.
Is it necessary to follow a diet for liver hemangioma?
Proper selection of nutrition is mandatory if the patient is determined for a positive result. Eating foods that are unacceptable in the diet of a sick person can provoke a sharp growth and rupture of the hemangioma.
Why is liver hemangioma dangerous?
Its main danger is possible tissue rupture and subsequent bleeding. There is also a possibility that due to the large size of the tumor, neighboring organs will be compressed, and therefore their functioning will be disrupted.
How to treat liver hemangioma?
Treatment for this disease is selected depending on its size and growth rate. The specialist can select hormonal therapy, minimally invasive methods (for example, radiation therapy), as well as surgery. To consolidate the effect of treatment, you must follow a special diet.
Education mechanism
Medicine has not found any exact reasons why this type of tumor forms on a baby’s body. There are more hypotheses than facts, despite the fact that many years of research into infant hemangiomas have been conducted.
Doctors are convinced of only one thing - the reasons are not genetic, therefore heredity in the formation mechanism is excluded by almost all specialists.
Development of hemangioma
However, there are aspects whose participation in the formation of hemangiomas is assumed with a high degree of probability.
- ARVI suffered by a pregnant woman in the early stages, between the third and sixth week. It is during this time period that the formation of the cardiovascular system of the embryo occurs.
- Rhesus conflict, when positive red blood cells from the fetus enter the maternal bloodstream.
- Pregnant women taking medications not authorized by a doctor, smoking during pregnancy, drinking alcohol.
- The presence of hormonal imbalances and disorders in both the fetus and its mother.
- Low level of ecology where the pregnant woman lives.
- Heredity aggravated by any vascular disease.
- Multiple pregnancy (starting with twins).
- The age of the woman giving birth is over 38 years.
- Birth of a child prematurely.
- Convulsive seizures in a pregnant woman.
In multiple pregnancies, there is a risk of developing hemangiomas in children
Bad habits increase the risk of developing fetal pathologies
If we briefly characterize the hypothesis of the mechanism of formation, it will sound like this. At the stage of bearing a child, when its cardiovascular system is formed, endothelial cells, under the influence of some (not precisely established) factors, are sent to the “wrong address”. Instead of forming the inner surface of the blood vessels, they form a tumor.
Bandages for pregnant women
If you want to find out in more detail what symptoms spinal hemangioma has, and also consider alternative treatment methods, you can read an article about this on our portal.
Treatment
A small liver hemangioma, the causes of which were discussed above, does not harm the body and does not require treatment. If the vascular seal grows, it is removed during surgery. But the operation becomes impossible if both lobes are affected. In this case, drug treatment is carried out, based on an individual hormonal course. Also, the accumulation of blood vessels can be destroyed using a laser, radiotherapy or electrocoagulation.
Prevention
There is an opinion that the causes of hemanginoma in most cases are the acute respiratory viral infection suffered by the mother during pregnancy. Therefore, as preventive measures for the child, the mother carrying him should protect herself as much as possible from this type of infection.
To prevent the formation from transforming into a malignant tumor, it is necessary to adhere to a strict diet, eliminating fatty, salty, spicy and fried foods from the diet and more often consuming fish, milk, liver and all products containing vitamin B12, which is very beneficial for liver health.