Causes of the disease
Bursitis is usually infectious in nature. It can be caused by untreated inflammatory pathologies. Viruses and bacteria are often the causative agents, leading to the development of sinusitis, otitis, bronchitis, abscess or the formation of another source of infection.
The cause of the onset of the inflammatory process can also be:
- allergic reaction;
- poor circulation in the joint capsule;
- injuries of the synovial bursa or its vessels.
People at risk include people with low or excessive physical activity. In both cases there is an increased risk of injury. Therefore, inflammation of the joint capsule is more common among housewives, office workers, drivers, miners, and professional athletes.
How to deal with bursitis
Bursitis
(from Late Latin bursa - bursa) is
a painful inflammation of the joint capsule (a flat, fluid-filled sac used to protect when skin, muscles, tendons and ligaments rub against bone).
- Movement is usually accompanied by pain, and the joint capsule near the surface of the skin may swell and hurt.
- Pain around the joint capsules may prompt the diagnosis, but analysis of synovial fluid collected from the joint capsule or imaging studies are sometimes required.
- Rest, splinting, nonsteroidal anti-inflammatory drugs, and occasional corticosteroid injections help relieve symptoms.
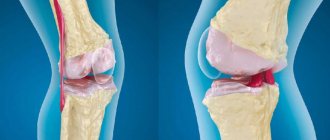
Usually there is a small amount of fluid in the joint capsule that provides shock absorption. The bursa reduces friction and prevents wear and tear when structures move relative to each other. Some joint capsules are located directly under the skin (superficial joint capsules). Others are located under the muscles and tendons (deep joint capsules). In case of injury or high load, inflammation of the joint capsule may occur, which leads to the accumulation of excess fluid in it.
Inflammation can be caused by an infection, but more often it is a consequence of bruises or injuries, as well as constant friction of tendons and muscles against bones and ligaments. This is why bursitis is common among professional athletes, especially weightlifters and team sports players, skydivers, and anyone who lands hard or hits their knee.
The chronic form of the disease often occurs in those who, due to their occupation, spend a lot of time standing or crawling on their knees. The same maids used to often suffer from bursitis because they washed the floors with their hands. Today they use a vacuum cleaner more and more, so they take less risks. But roofers, parquet layers, gardeners, as well as overzealous housewives who care more about the cleanliness of the floors than about their health are in a particularly dangerous zone.
Bursitis usually occurs when:
- irritation from unusual or excessive exertion.
It can also result from injury, gout, pseudogout, rheumatoid arthritis, or certain infections, especially those caused by Staphylococcus aureus. The cause of bursitis is often unknown.
The shoulder joint is most vulnerable to bursitis, but the elbows, hips (acetabulum bursitis), pelvis, knees, toes and heels (Achilles bursitis) can also be affected. People with shoulder bursitis often develop inflammation of the tendons around the shoulder (rotator cuff tendonitis—the tendons and other structures involved in moving, rotating, and stabilizing the shoulder joint are called the rotator cuff).
SYMPTOMS OF BURSITIS
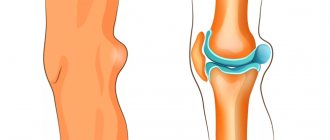
Bursitis is usually accompanied by pain and often limits freedom of movement, but specific symptoms depend on the location of the inflamed joint capsule. For example, when the joint capsule of the shoulder is inflamed, raising the arm to the side (for example, when putting on a jacket) is accompanied by pain and difficulty. However, elbow bursitis may be accompanied by swelling in the absence of significant discomfort (or its complete absence).
Acute bursitis develops over several hours or days. The inflamed area is usually characterized by pain when moving or touching. The skin over superficial joint capsules, such as near the knee and elbow joints, may become red and swollen. Acute bursitis, caused by infection or gout, may be partially painful and the affected area may become red and hot.
Chronic bursitis may develop due to repeated or persistent episodes of acute bursitis or repeated trauma. Occasionally, thinning of the walls of the joint capsule is observed. With unusual loading or stretching of the damaged joint capsule, the course of the inflammatory process may worsen. Prolonged pain and swelling can limit freedom of movement and lead to muscle weakness. Exacerbations of chronic bursitis can last several months and often recur.
DIAGNOSTICS
- Medical examination;
- Sometimes examination of the contents of the joint capsule;
- Sometimes imaging tests.
The doctor suspects bursitis if the area near the superficial joint capsule is painful to the touch, or if pain occurs during movements that lead to displacement or increased pressure on the deep joint capsule.
If the superficial joint bursa, especially near the knee or elbow joint, is noticeably swollen, the doctor may use a needle to remove a sample of synovial fluid from the bursa. The sample is then sent for analysis to determine the cause of inflammation, such as infection or gout.
An X-ray is usually done if the bursitis does not improve with treatment or continues to recur, or if the doctor suspects a problem in the joint, such as arthritis.
Magnetic resonance imaging (MRI) or ultrasound may be ordered to confirm deep bursitis.
TREATMENT OF BURSITIS
- Painkillers, anti-inflammatory drugs and rest;
- Treatment of gout or infection;
- Sometimes corticosteroid injections.
For the treatment of acute bursitis not caused by an infectious agent, the following is usually prescribed:
- Peace;
- Temporary immobilization (for example, using a splint) of the affected joint;
- Applying ice to the painful area;
- Nonsteroidal anti-inflammatory drugs (NSAIDs) in high doses.
Sometimes strong painkillers are required. Often, the doctor may inject a local anesthetic directly into the joint capsule, especially if the shoulder joint is affected. This treatment often provides symptom relief for several days after the injection. The injection can be repeated after a few months. Removing fluid with a needle may also help relieve pain.
Patients with acute bursitis are sometimes prescribed corticosteroids, such as prednisone, taken by mouth for several days. Once the pain has subsided, patients can do special exercises to increase the range of motion of the joint.
Chronic bursitis, if it is not caused by an infectious agent, is treated in a similar way, although rest and immobilization are not as effective. In rare cases, surgery is performed to remove the joint capsule.
It is often possible to restore function with physical therapy. Exercises can strengthen weakened muscles and restore the full range of motion of the joint.
It is necessary to drain the infected joint capsule and prescribe appropriate antibiotics, often active against Staphylococcus aureus.
If the cause of bursitis, such as gout, rheumatoid arthritis or chronic overuse, is not treated or corrected, relapses of bursitis are common.
AT-RISK GROUPS
Athletes whose activities involve lifting weights, as well as track and field athletes and runners are most likely to develop bursitis.
The risk of developing bursitis is also increased by monotonous physical activity, which can be experienced by people whose professional activities require long stays in one position (roofers, parquet layers and other professions with monotonous physical activity).
Also at risk for developing bursitis are patients suffering from alcoholism, diabetes, and kidney disease.
In addition, gout, arthritis, rheumatoid arthritis, scleroderma, and erysipelas can trigger the development of bursitis.
Types of bursitis
In medicine, the disease is given several classifications. Types of the disease are distinguished by the location of inflammation, the composition of the exudate and the reasons that led to the development of the pathology. There are 160 bursae in the human body. But the bursae of large joints become inflamed more often:
- elbows;
- shoulder;
- knee;
- hip
Based on the composition of the exudate released into the capsule, serous, purulent, fibrinous and hemorrhagic bursitis are distinguished. In the first case, an almost transparent and quickly absorbable liquid accumulates in the bursa. In the purulent form of the disease, pus is released into it, fibrinous - fibrin, hemorrhagic - blood.
Bursitis can be primary or secondary. In the first case, there are no internal reasons that could cause it. Secondary pathology is usually a consequence of another disease - rheumatoid arthritis, psoriasis, diabetes, etc.
Why self-medication is dangerous
Self-medication is no less dangerous. A doctor at an appointment can recognize bursitis even by minimal signs. To confirm the diagnosis, he will prescribe an ultrasound, x-ray, MRI and will know exactly where the inflammatory process is located. After this, the doctor prescribes treatment for acute bursitis, which may include:
- non-steroidal anti-inflammatory drugs (NSAIDs) – Ibuprofen, Dexalgin, etc.; these drugs also have an analgesic effect;
- in case of a purulent process, the doctor pierces the bursa, removes the pus and rinses the cavity with antiseptics and administers antibiotics;
- in case of severe inflammation, hormonal drugs are injected into the bag;
- prescribes physiotherapeutic procedures.
If all this is not done and treatment is carried out at home with folk remedies, then the risk of developing complications increases sharply, the treatment of which is problematic even for a specialist.
Acute bursitis rarely develops without chronic joint injury. Joint pain requires immediate medical attention. If this is not done, the consequences may last a lifetime.
Sign up for a free initial appointment
How does the disease manifest itself?
Bursitis can be acute or chronic. Both forms of the disease have a similar clinical picture. For the first time, the disease develops acutely and is manifested by the following symptoms:
- swelling of the joint;
- redness of the skin at the site of the lesion;
- pain that gets worse with exercise;
- stiffness of movements;
- increased weakness;
- increased sweating;
- increased body temperature;
- elastic swelling of a round shape, deflecting when pressed (due to the accumulation of effusion in the bag).
If there is no treatment, symptoms worsen. Body temperature rises to +39…+40 °C, swelling increases, pain does not go away even with rest. Then the disease becomes chronic. It is characterized by alternating periods of remission and exacerbation.
Chronic bursitis of the elbow, knee or other joint is manifested by softening of the swelling. Pain when pressed goes away and mobility returns. Redness and swelling disappear. But the inflammation may worsen. This is facilitated by particles of tissue remaining in the bursa after the end of the acute period.
What happens if acute bursitis is not treated?
The appearance of protrusion and pain should be a reason to consult a doctor. If treatment is not started in time, bursitis can become more complicated:
- development of an acute purulent process, infection of surrounding tissues, phlegmon;
- development of arthritis with subsequent decrease in limb function;
- the acute course will turn into chronic with constant pain that forces you to leave your profession or sports.
We combine proven techniques of the East and innovative methods of Western medicine
Read more about our unique method of treating bursitis
Methods of treating the disease
Bursitis is treated by a surgeon or orthopedic traumatologist. But before his appointment, he conducts a diagnosis. It includes an external examination, palpation of the joint, as well as blood tests and puncture of the bursa to collect synovial fluid. Its research helps to establish the type of pathogen and select drugs effective against it.
During treatment, it is important for the patient to ensure the immobility of the diseased joint. Therefore, most of the time he should be at rest. He is prescribed:
- Injections with glucocorticosteroids into the cavity of the bursa. They reduce inflammation and relieve pain.
- Removal of excess effusion using a sharp needle that is inserted into the capsule.
- Rinsing the bag with antiseptic solutions. They are also introduced into the cavity through a needle.
- Antibacterial therapy for the bacterial form of the disease.
- Compresses with anti-inflammatory and analgesic solutions to reduce pain and external symptoms of inflammation.
The initial stage of the disease can be easily treated without consequences for the patient. Therefore, at the first symptoms of bursitis, contact your doctor. Our surgeons will conduct a series of studies to clarify the diagnosis and prescribe competent treatment.
Diagnostics
Acute bursitis is usually visible to the naked eye due to reddened skin and swelling of the joint. For more accurate diagnosis, use:
- Palpation (feeling) of the joint.
- X-ray - the study will show not only inflammation, but also pathologies of bone and cartilage tissue in the joint, salt deposits, thickening of the synovial bursa.
- Ultrasound or MRI - for diagnosing soft tissues.
- Laboratory tests - blood, PCR diagnostics for the analysis of inflammatory pathogens.
2.What parts of the body does bursitis affect?
Bursitis can develop in different joints. And depending on the location, there are different types of bursitis
:
- Elbow bursitis, or bursitis of the elbow joint;
- Shoulder bursitis, or bursitis of the shoulder joint;
- Bursitis of the hip, or bursitis of the hip joint;
- Bursitis of the knee, or knee bursitis, bursitis of the knee joint;
- Bursitis of the calcaneal tendon, or calcaneal bursitis, subcalcaneal bursitis.
Visit our Traumatology and Orthopedics page
4. Treatment of the disease
Elbow bursitis, shoulder bursitis, knee bursitis and other types of bursitis can be treated in different ways:
- First of all, you should avoid those actions that caused bursitis;
- The affected area should be given maximum rest, without stress;
- At the time of injury, you can apply cold to the painful area;
- Over-the-counter anti-inflammatory medications can be used.
If treating bursitis at home within a week does not produce noticeable results, you need to consult a good doctor.
The doctor may recommend medications
to reduce inflammation. Corticosteroid anti-inflammatory drugs are often used to treat bursitis because they quickly help reduce inflammation and pain. Steroids can be given directly to the injured area as an injection. Often, although not always, this method of treating bursitis is very effective. Sometimes a repeat injection is required. However, multiple injections of steroid medications are generally not used because they may cause side effects. In addition, if such treatment does not work, there may be another problem that frequent injections will not reveal.
Treatment of bursitis with physiotherapy
is another common method. When combined with splinting the thumb, forearm and other areas, it can be very effective. In rare cases, when other treatments for bursitis do not help, surgery may be performed.