What is Parkinson's disease (PD)? This is a chronic pathology of the central nervous system with a gradually progressive course, the development of which is based on the degeneration and death of neurons that synthesize dopamine in the substantia nigra of the brain. Dopamine is known as a neurotransmitter, which in a healthy person is supplied in sufficient quantities by axonal transport to the subcortical nuclei of the brain. This process allows you to keep motor activity and muscle tone under control. In Parkinson's disease, the production of a biological substance is reduced due to neurodegeneration (destruction) of dopamine neurons, which gradually die.
As nerve cells die, dopamine synthesis becomes more and more inhibited. When the level of dead neurons reaches a critical level, the disease begins to manifest itself. A person develops serious movement disorders, which become a difficult ordeal for the patient and his family. Due to chronic degeneration of the structures of the substantia nigra of the brain, the pathological process is irreversible and permanent.
general information
Parkinson's disease affects men twice as often as women. In most cases, it develops after 60 years of age, but cases of early onset of the disease are recorded (at 30-40 years of age), as well as juvenile forms that develop in people in their twenties.
There are several hypotheses for the formation of pathology. It has now been precisely proven that one of the mechanisms of its development is the gradual degeneration of neurons and a decrease in the production of dopamine. It is an important neurotransmitter involved in the transmission of nerve impulses. As a result, a specific set of disorders is formed, which makes it easy to make a diagnosis.
Epidemiology
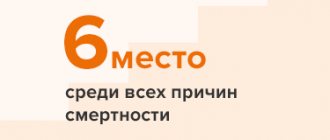
According to a continuous population study, the prevalence of PD in Russia is 139 cases per 100,000 population, the incidence of PD is 16 cases per 100,000 population per year. With increasing age, the risk of PD increases, and the detection rate of PD among people over 65 years of age is already about 1%. Most cases of the disease occur between the ages of 60 and 70 years. However, in 15% of cases, PD debuts before the age of 45 years.
Based on the available data and the age-sex structure of the Russian population, we can roughly estimate the total number of patients with PD in our country at 210 thousand, with the disease occurring in approximately 20 thousand patients each year. Approximate calculations show that at least a quarter of patients (that is, more than 50 thousand) end up outside the scope of medical care, and most of these are patients with an early stage of the disease [3].
Causes
The exact causes of Parkinson's disease have not been identified. Scientists have been able to identify only a number of factors that increase the risk of developing neurodegenerative processes:
- natural processes of aging of the body, accompanied by a decrease in the ability of tissues to regenerate;
- genetic predisposition (this is especially true for forms with early onset);
- chronic lack of vitamin D, which protects neurons from the pathological effects of toxins;
- intoxication with salts of heavy metals, pesticides, alcohol;
- poor environmental conditions in the region of residence;
- taking certain medications (for example, chlorpromazine);
- chronic insufficiency of blood supply to the brain (due to atherosclerosis, osteochondrosis of the cervical spine, etc.);
- infections affecting the central and peripheral nervous system (meningitis, encephalitis, herpes viruses, influenza);
- brain tumors;
- traumatic brain injuries;
- smoking;
- frequent and prolonged stress, chronic fatigue.
Make an appointment
Treatment of parkinsonism, drugs
There are two types of medications used in the treatment of parkinsonism:
- antiparkinsonian anticholinergic drugs, which include dynesin, bellazone, cyclodol, etpenal, tropacin, norakin;
- antiparkinsonian dopaminergic drugs levopa, glutantan, midantan, deprenyl.
Medicines have contraindications. Many are capable of provoking negative reactions. Including provoking hallucinations.
Symptoms
Parkinson's disease is manifested by specific symptoms, which together form a clear picture of the disease:
- tremor: fine trembling begins in one hand and then spreads to both limbs and head; the movement of the fingers is somewhat reminiscent of counting coins; while performing purposeful movements (for example, while working at a computer);
- general slowness of movements (bradykinesia): the patient often freezes in one position;
- specific gait: a person moves with small, shuffling steps, as if he is constantly on very slippery ice;
- poor facial expressions: a mask effect is formed due to low mobility of facial muscles;
- monotonous, quiet speech;
- increased muscle tone (muscle rigidity): the figure becomes stooped, arms and legs are slightly bent, the head is tilted forward;
- postural instability: a person has difficulty starting and ending movements, resulting in decreased ability to maintain balance;
- disorders of the autonomic nervous system: oily skin, excessive secretion of saliva and sweat;
- decreased sense of smell;
- constipation, urinary disorders.
Unlike other neurodegenerative diseases, Parkinson's disease has little effect on intelligence in early and middle stages of development. As the pathology progresses, there is a decrease in the speed of thinking and speaking, decreased mood, depression and indifference to everything that happens.
How does the disease manifest itself?
Main symptoms of Parkinson's disease:
- Tremor of the limbs is often the first sign of pathology. At rest, the patient’s hands tremble uncontrollably, and in more severe stages also the tongue, lower jaw, and eyelids;
- slow, stiff movements, shuffling gait;
- quiet and emotionless speech;
- constant tension in the muscles;
- mask effect on the face (hypomimia). The facial muscles stop moving normally, so the person looks devoid of emotions;
- difficulties with coordination and maintaining balance; in later stages, the patient may fall when trying to move without assistance;
- disturbances in the functioning of the salivary, sweat, sebaceous glands, loss of smell.
As the disease progresses, these symptoms may intensify and multiply. Sometimes the above-mentioned manifestations are accompanied by sleep disturbances, pain, depression and other symptoms.
Stages of development
Currently, doctors distinguish 5 stages of Parkinson's disease, manifested by a certain set of symptoms:
- Stage 0: no clinical manifestations;
- Stage 1: there are slight difficulties in moving one arm, a slight tremor, first with excitement, then at rest; the sense of smell and sleep are disrupted, fatigue and apathy appear;
- Stage 2: disturbances involve the second hand, trembling of the tongue and lower jaw appears; salivation; hypokinesia is formed; the ability to self-care is preserved;
- Stage 3: stiffness and impoverishment of movements increases, facial expressions are almost absent; a specific gait and posture is formed; during a conversation, the patient begins to get stuck on the same word; self-care is difficult, but possible;
- Stage 4: postural instability develops, the patient begins to fall frequently; the intellect begins to suffer, depression increases; At this time, suicide attempts are common; a person needs help to perform simple actions;
- Stage 5: manifestations reach their climax, the person cannot sit down, stand up and walk independently, eating is difficult due to swallowing disorders; loss of control over bowel movements and urination; the patient requires constant care.
Use of extended-release pramipexole in early PD
The development of new dosage forms of antiparkinsonian drugs that provide them with a prolonged release and allow a single dose during the day not only makes treatment more convenient, but also, by improving patient adherence to treatment, increases the long-term effectiveness of therapy. In addition, with a slow release of the drug throughout the day, a more stable concentration in the blood is achieved, which can ensure better tolerability and effective control of disease symptoms throughout the day (both during the day and at night).
A new dosage form of pramipexole with prolonged (controlled) release, which involves a single dose during the day, has been used in European countries and the USA since 2009, and in our country - since 2012. It is a matrix tablet in which the active substance is evenly distributed in a polymer matrix. In the gastrointestinal tract, the matrix absorbs liquid and turns into a gel, which uniformly releases pramipexole over 24 hours. Since pramipexole is highly soluble in a liquid medium, regardless of its pH, the active substance is released from the matrix and absorbed throughout the intestine. The rate of gastric emptying and intestinal motility do not significantly affect the effect of the drug. Absorption parameters also do not depend on whether the drug is taken on an empty stomach or after a meal [2].
When developing a new dosage form, the possibility of a simple, immediate transition from the traditional form of the drug to the new one was taken into account. The condition for this is that equal daily doses of immediate release (taken 3 times a day) and extended release (taken once a day) have the same antiparkinsonian effect. The difference between the new and traditional dosage forms of pramipexole lies only in the rate of release of the active substance. The half-life of pramipexole is the same when using both forms, but controlled release ensures longer maintenance of therapeutic drug concentrations in the blood [5].
The equivalence of equal daily doses of immediate- and extended-release pramipexole has been demonstrated in a number of clinical trials.
It is worth emphasizing the particular convenience of the new dosage form of pramipexole, which can be taken once a day, for patients with early stage PD who continue to work. To avoid side effects, the drug is prescribed by slow titration - according to the same scheme as the immediate-release drug. For this purpose, extended-release pramipexole tablets are available in several strengths: 0.375, 0.75, 1.5, 3 and 4.5 mg. Treatment begins with a dose of 0.375 mg once a day, then, subject to good tolerance, every 7 days they move to the next dose level until the optimal effect is achieved, up to a maximum of 4.5 mg/day (Table 3). After reaching a dose of 1.5 mg/day, it is sometimes advisable to titrate more slowly, since the development of the full therapeutic effect may require several weeks. The recommended dose for maintenance therapy (both in early and in advanced or late stages of the disease) can range from 0.375 to 4.5 mg/day. The most commonly used dose is 3 mg/day.
Table 3. Titration schedule for extended-release pramipexole.
| A week | Dose |
| 1st | 0.375 mg 1 time per day |
| 2nd | 0.75 mg 1 time per day |
| 3rd | 1.5 mg 1 time per day |
| 4th | 2.25 mg 1 time per day |
| 5th | 3 mg 1 time per day |
| 6th | 3.75 mg 1 time per day |
| 7th | 4.5 mg 1 time per day |
Diagnostics
The diagnosis of Parkinson's disease is made based on the characteristic clinical picture. The patient is examined by a neurologist who notes typical signs. Complaints must be clarified and an anamnesis of the disease (history of the appearance of symptoms) and life history (information about previous injuries, chronic diseases, surgical interventions) is collected. Laboratory and instrumental diagnostics are used to clarify concomitant pathology and exclude other causes of neurological disorders.
Treatment of Parkinson's disease
At the moment, successfully selected treatment for Parkinson's disease can stop the process of degradation and reduce the severity of pathological symptoms. The disease begins to progress more slowly, which allows patients to stay in good shape longer.
Drug treatment
Drug treatment is aimed at restoring the balance of dopamine in the central nervous system. The following drugs are used:
- Levodopa and its analogues: serve as the basis for the production of dopamine;
- dopamine receptor agonists: stimulate receptors similar to a natural neurotransmitter and reduce the severity of symptoms;
- MAO-B inhibitors: reduce the breakdown of dopamine;
- COMT inhibitors: prescribed in combination with levodopa and reduce its breakdown;
- anticholinergics: aimed at reducing symptoms.
There are combination products that combine several active ingredients for the fastest possible effect.
Non-drug treatment
Drug treatment is complemented by physiotherapy, exercise therapy and massage. Physiotherapy is used to activate metabolic processes and increase blood flow in the brain. Depending on the patient’s condition and concomitant diseases, the following may be prescribed:
- magnetic therapy;
- ultrasound stimulation;
- electrosleep;
- mineral baths;
- acupuncture.
The massage is aimed at improving motor activity. Intensive muscle kneading and passive gymnastics reduce muscle stiffness and have a general strengthening effect.
Physical therapy exercises allow you to:
- reduce muscle stiffness and strengthen it;
- increase sense of balance;
- improve the patient's emotional state.
Most exercises are aimed at training the sense of balance. The complex is selected individually depending on the patient’s condition, age and concomitant diseases.
Surgery
The help of surgeons is relevant in the last stages of the disease. The most effective and safest operation is the installation of a brain stimulator. The intervention does not require opening the skull. Thin electrodes are inserted into the brain and a small stimulator is placed under the skin of the collarbone. The device is programmed for a specific pulse frequency; in addition, the patient and his relatives can change the settings depending on the condition. Using a stimulant allows you to reduce the dosage of medications and keep symptoms under control for a long time.
Other surgical treatment options require working on an open brain:
- thalamotomy: destruction of part of the thalamus, allowing to get rid of tremors, but maintaining other symptoms;
- pallidotomy: partial removal of one area of the brain (globus pallidus), significantly reducing all the main symptoms of the pathology.
Non-drug methods
Treatment of Parkinson's disease in our clinic is not limited to the selection of medications. To improve the condition, it is recommended to use a diet. According to the research results, the patient has positive changes in motor function with certain dietary habits:
- reducing the amount of protein food;
- sufficient fluid intake (in the absence of contraindications);
- frequency of meals – up to 4-5 per day, in small portions;
- complete cessation of alcohol consumption;
- regular intake of caffeinated drinks;
- consumption of berries high in anthocyanins (strawberries, raspberries, currants);
- a decrease in vitamin D levels in Parkinson's disease requires constant intake of fish and seafood, as well as regular walks in sunny weather.
Great importance is given to doing exercises. Physical therapy for neurodegeneration helps:
- improve cerebral and peripheral blood flow;
- accelerate the production and action of dopamine;
- reduce oxidative stress;
- reduce the severity of tremor;
- strengthen muscle tissue and prevent its atrophy;
- prevent falls and injuries, normalize coordination.
The specialist selects certain exercises that should be performed regularly, for 20 minutes, 2-3 times a day, only in this case can you count on the formation of muscle memory. This complex includes stage plastique movements, training in relaxation and proper breathing. This takes into account the age and degree of endurance of the person, the presence of complications and other factors.
The frequency and duration of movements depends on the stage of the pathology and the person’s activity. They are selected in such a way that all muscle groups are trained, but with an emphasis on areas that require more correction.
Treatment of Parkinson's disease in Moscow involves the use of physiotherapy. Various methods of exposure can be used already in the first stages of the disease. They help reduce pain symptoms, remove hypertonicity of muscle fibers, and improve tissue trophism. The positive effect of physiotherapeutic treatment methods on the central, autonomic and peripheral nervous systems, as well as the condition of the musculoskeletal system, has been proven.
The following types of therapy are recommended for patients with parkinsonism:
- transcranial magnetic brain stimulation;
- pulsed electrotherapy on the cranial area;
- magnetic therapy;
- pulsed low-frequency electrostatic therapy on the lower leg muscles;
- pressotherapy in the lower extremities and lower back;
- electrophoresis with drugs to relieve spasms and pain;
- electrosleep;
- ultraviolet irradiation;
- balneotherapy and mud therapy.
If you make an appointment at Dr. Isaev’s clinic, you can not only significantly improve the condition of a loved one. An important aspect of the treatment of Parkinson's disease is family consultations with a psychologist. The patient’s relatives are explained the features, causes and signs of the disease, told how to care for a person with this problem, and taught how to properly communicate with him.
Complications
Restriction of muscle function in Parkinson's disease inevitably leads to a decrease in the intensity of blood flow and a decrease in the level of metabolism. Already in the middle stages of the development of the disease, the risk of blood clots and the development of dangerous conditions increases significantly:
- ischemic or hemorrhagic stroke;
- myocardial infarction, angina pectoris, heart failure;
- pulmonary embolism.
Bedridden patients often face severe complications associated with a recumbent position:
- congestive pneumonia;
- aspiration pneumonia (due to impaired swallowing, food enters the respiratory tract);
- bedsore infection and sepsis.
Most patients experience apathy and severe depression, which lead to suicidal thoughts. Some patients carry out plans and commit suicide.
Correctly selected treatment significantly reduces the risk of complications, which is why it is important to consult a doctor in a timely manner.
Prevention
Prevention of Parkinson's disease includes:
- proper nutrition with a minimum amount of preservatives and artificial additives, a sufficient amount of vitamin D, omega-3, antioxidants;
- regular physical activity to prevent physical inactivity;
- adequate sleep of at least 8 hours a day, adherence to a work and rest schedule;
- minimizing stress and fatigue;
- quitting smoking and drinking alcohol;
- regular medical examinations, compliance with all doctor’s recommendations;
- timely contact a specialist if any suspicious symptoms appear.
Make an appointment
Treatment at the Energy of Health clinic
Neurologists at the Energy of Health clinic will come to the rescue at any stage of Parkinson’s disease. We offer comprehensive treatment in accordance with modern standards:
- selection of drug therapy;
- physiotherapeutic procedures: magnetotherapy, laser treatment, etc.;
- therapeutic massage courses;
- Exercise therapy directly in the clinic;
- training in physical exercises for exercise at home;
- organization of sanatorium-resort treatment if indicated;
- training relatives in the rules of caring for the sick;
- work with a psychologist and psychiatrist if necessary.
Advantages of the clinic
The Health Energy Clinic has experienced doctors, skilled nurses and modern equipment for diagnosing and treating various diseases. We offer:
- diagnostics using instrumental, functional and laboratory studies;
- consultations with experienced specialists in various fields;
- obtaining the opinion of foreign colleagues if necessary;
- individual selection of treatment;
- complex therapeutic regimens using medications, physiotherapy and other methods;
- extensive screening programs for early diagnosis of diseases;
- detailed consultations on disease prevention;
- any certificates and conclusions.
Parkinson's disease begins very slowly, but it is almost impossible to stop the process. If you or your family have suspicious signs, do not delay contacting a doctor. Sign up for diagnostics at the Energy of Health clinic.