Urolithiasis (UCD) is a term that is familiar to a huge number of people. This disease is characterized by the appearance of various types of stones in the organs of the urinary system. Most often, the disease occurs in people of working age - from 22 to 55 years. In the absence of timely treatment, 6% of patients suffering from it risk receiving 2nd degree disability.
Scientists believe that the presence of stones in the genitourinary system is a manifestation of an imbalance in the entire body. It is impossible to say that only one factor led to the appearance of this disease.
Causes of urolithiasis development
Factors that provoke the development of kidney urolithiasis in women and men can be very diverse. There are reasons that contribute to the appearance of stones in the organs of the genitourinary system, and mechanisms that directly result in the appearance of stones.
The reasons contributing to the development of urolithiasis include:
1) congenital abnormalities of the kidney structure. In most cases, stones appear in the kidneys and from there descend into the ureters, bladder, and urethra. Congenital anatomical narrowing of these organs contributes to the appearance of stones;
2) metabolic disorders in the body. Congenital or acquired malfunctions in the metabolic system most often lead to the appearance of the disease. These include: oxaluria, galactosuria, uraturia, cystinuria, aminoaciduria. With all these pathologies, excessive amounts of oxalates, urates, galactose, and cysteine are produced, which are deposited in the renal tubules. They are the basis of future kidney stones;
3) genetic predisposition. According to reviews from patients of our medical center in St. Petersburg, whose relatives suffered from urolithiasis and had many stones or single coral stones, this disease can indeed be inherited;
4) exogenous factors, or factors that are outside the body. These include gender, age, geographic location and climate in the region. Thus, middle-aged people with sedentary jobs living in hot climates suffer from impaired urine flow and urolithiasis three times more often than people leading an active lifestyle and living in cool climates. This effect on the body is quite simple to explain - in a hot climate, with a passive body position, urine stagnates in the genitourinary organs. The high concentration of salts, which arises due to the climate, leads to the formation of disease.
There are also general and local processes within the body that contribute to the development of ICD. Common factors include:
- violation of the metabolism of vitamins A and D;
- long-term immobilization of injured limbs using a plaster cast (more than 3 months);
- excessive amounts of calcium salts in the body;
- the presence of a bacterial infection in the body, including bacterial pyelonephritis;
- long-term use of certain medications (antacids for chronic gastritis and ulcers, tetracyclines for bacterial diseases, sulfonamides for autoimmune diseases, ascorbic acid for vitamin deficiencies, glucocorticoids after transplantations, for multiple sclerosis and a number of other diseases) can also cause the development of urolithiasis.
Local factors include various diseases and conditions of the genitourinary system:
- anatomical structural disorders;
- long-term presence of catheters in the bladder and genitourinary tract;
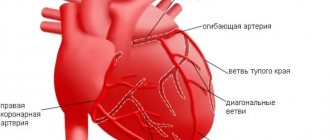
- insufficient blood supply to the genitourinary organs;
- vesicoureteral reflux;
- spinal cord injuries that impair the flow of urine;
- nephroptosis, or kidney prolapse.
The presence or absence of one or more factors does not mean the appearance of the disease. Only the individual characteristics of the body and a person’s way of life determine the development of this disease.
Complications
Urolithiasis, if the patient is not treated in time, can lead to more serious consequences:
- penetration, development and spread of infections in the urinary tract;
- pyelonephritis and other kidney diseases;
- nephrosclerosis. These are transformations of kidney tissue that are associated with degenerative processes;
- problems with the intestines - in particular, paresis;
- accumulation of purulent formations;
- renal failure and bacterial shock.
If the stone is not removed, then as the disease develops the kidney may even die - this is extremely dangerous and risky, so the disease requires effective and thorough treatment.
Formation and types of stones in urolithiasis
The mechanism of formation is quite simple - congenital and acquired diseases lead to an imbalance of various substances in the body.
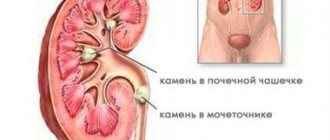
As a result, the amount of minerals that settle in the kidney tubules increases. Constrictions in the renal collecting system, stagnation of urine, and a sedentary lifestyle create ideal conditions for the formation of stones. Small stones manage to pass through the hilum of the kidney into the ureter, where they can become stuck, or move further into the bladder or urethra. There are different types of urinary stones. In most cases, stones in the genitourinary organs are polymorphic in structure - they contain various substances. And only the predominance of one of them determines the name of a particular stone: 1) calcium-containing. In men and women suffering from urolithiasis, such stones are found in most cases. They are most often found in the kidneys. They are divided into calcium phosphate and calcium oxalate stones.
2) pure oxalate. Most often found in the urinary tract. These include varieties such as wewellite and weddellite. Such stones are formed due to prolonged dehydration of the body - these can be chronic infectious diseases, autoimmune diseases, alcoholism.
3) urate. They are formed due to excessive amounts of uric acid salts in the body. They are often found in people suffering from gout and obesity.
4) phosphate. These are hydroxyapatite, struvite, carbonate apatite. The formation of these stones is associated with substances released by bacteria. That is why it is extremely important to treat bacterial diseases in a timely manner.
5) cystine. Observed in the body when the metabolism of the amino acid cysteine is disturbed. Such stones are quite rare.
6) the most rare occurrence in patients with urolithiasis is the appearance of cholesterol stones. As a rule, they contain a high percentage of oxalates and phosphates. In addition to the variety of morphological structure, each stone has its own color and shape. Thus, oxalates are dark in color with a prickly surface, phosphates are light gray and almost smooth. Urates are yellowish in color with an uneven surface.
Symptoms of urolithiasis
The symptoms of the disease depend on the shape, size, location of stones, quantity and mobility. Fixed small stones can form in the kidneys for years without causing any inconvenience to a person. At the same time, one stone with an uneven surface can pass into the ureters, where it will irritate the membranes and nerve receptors, disrupt the outflow of urine, thereby causing severe pain.
There are three main symptoms that characterize the presence of urolithiasis in a person:
- pain;
- hematuria (the appearance of blood in the urine - determined by urine analysis or visually);
- passage of stones or their fragments in the urine.
In most cases, the first two symptoms occur. The third is typical for small stones that can pass through the genitourinary tract. The main symptom of urolithiasis is pain. Its appearance, nature, intensity, localization depend on the location of the stone and its passage through the genitourinary tract. Thus, kidney stones most often cause pain in the lumbar region. If the stone is in the ureter, it can be either in the corresponding part of the back or in the abdomen. When small stones get into the ureter, sometimes its lumen is completely blocked. This causes pain of characteristic intensity and duration, which is called “renal colic”.
Symptoms in patients with extrarenal urolithiasis
Stones that are located in the lower parts of the ureters appear a little differently. In particular, pain will be localized to the side of the midline of the abdomen on the right or left, depending on the affected ureter. The level of pain will depend on the location of the stone - above the navel if the stone is in the upper third of the ureter, on the side of the belly if the stone is in the middle third, below the navel - in the lower third.
Pain in the pubic and suprapubic areas may indicate a stone in the bladder or urinary tract. As a rule, the presence of a stone in the bladder is accompanied by the development of severe pain, the intensity of which intensifies during urination. In this case, drops of blood may be released during or after urination. Scarlet blood before and during urination is a diagnostic indicator of the presence of a stone in the bladder or lower parts of the ureter.
Laboratory criteria
It is not too difficult to identify urolithiasis if a person has at least once had renal colic or a feeling of discomfort in the lumbar region. Objective signs of the disease, together with data from laboratory and instrumental tests, help the doctor make the correct diagnosis and proceed to treatment of the disease.
To diagnose the disease, urine analysis is of great importance. It allows you to determine the nature of the stones and, accordingly, choose the right treatment paths. The pH value of urine is of great importance. If it is 6.0, it means that urate and calcium oxalate stones are likely to form. If the pH reaches 7.1, there is a high probability of formation of phosphate stones with the addition of magnesium. A urine pH of 6.5 will indicate the formation of calcium phosphate stones. When urine pH values between 5.5 and 6.0 appear, uric acid stones may form.
This method is inaccurate and only allows us to guess what the mechanism of stone formation is. It must be used in complex diagnostics of the body. Healthy people and those who have previously been diagnosed with urolithiasis are recommended to take a urine test every three months.
When identifying a disease, it is also important to find the cause of the disease. Therefore, it is necessary to add tests for hormones and microelements to general tests. So, it is necessary to check the activity of parathyroid hormone, thyroid hormones, vitamin D, and catecholamines. It is also necessary to find out the amount of calcium and sodium in the body. An analysis of the amount of uric acid in urine and blood is mandatory.
Instrumental diagnostic methods
Quite relevant methods for diagnosing urolithiasis, which are used in our medical center in St. Petersburg, are ultrasound and excretory urography. Each of these methods has its own advantages and disadvantages. Ultrasound diagnostics allows you to detect stones of any size and any morphological structure. This method can be used by pregnant women; it is also perfect for people with allergies to contrast agents. The disadvantage of the study is the impossibility of examining the entire genitourinary tract, as a result of which a stone may simply not be found. An ultrasound can accurately show the presence or absence of any bladder stones. This procedure is performed only when the bladder is full.
Excretory urography is an x-ray method for detecting stones. Unfortunately, not all stones are visualized radiographically. Thus, oxalate stones will be clearly visible when using this research method, but urate and cysteine stones are not visualized. The essence of excretory urography is the administration of a special contrast agent. In this case, several photographs are taken that allow one to visualize the passage of this substance through the genitourinary tract. Thus, you can see a narrowing in one of the areas of the genitourinary system, which will correspond to the location of the stone.
Excretory radiography has a number of disadvantages and contraindications. So, it could be an allergic reaction to the contrast agent. X-rays are also contraindicated for children and pregnant women due to exposure to radiation to the body. This procedure also cannot be performed during an attack of renal colic and some diseases of the genitourinary system. In the absence of contraindications, excretory urography is best combined with ultrasound examination. This will make it more likely to detect the stone and establish its exact location.
Cystography, an X-ray examination of the bladder, is used to detect stones in the bladder. To do this, a catheter is inserted into the bladder, through which the bladder is filled with contrast. After contrast is administered, a picture is taken that shows the presence or absence of stones. An alternative to these methods is multislice magnetic resonance imaging. This method does not require the administration of contrast, it can be used during an attack of renal colic and it does not irradiate the patient. At the same time, stones of different densities are perfectly visualized in the pictures. The disadvantages of this research method include the high cost of this procedure.
Diagnostic methods
Urolithiasis can be diagnosed only after instrumental studies. The fact is that its symptoms are similar to various pathologies of the abdominal organs.
Diagnostics implies:
- Anamnesis collection. This is the initial stage of diagnosis, during which the doctor studies the patient’s lifestyle, dietary habits, the presence of chronic diseases, symptoms, as well as the medications he is taking.
- Ultrasonography. Allows you to identify X-ray positive and X-ray negative stones. An ultrasound of the kidneys or bladder is performed.
- X-ray. Most stones are detected during survey urography. It should be noted that X-ray negative stones cannot be detected using X-rays because they do not produce shadows on the images.
- CT. Computed tomography is the most informative diagnostic method, allowing to identify the exact number, location and size of stones.
How to treat urolithiasis?
Treatment of urolithiasis has several principles. This:
- elimination of pain (mainly with renal colic);
- restoration of the normal outflow of urine, which is disrupted due to blockage of the ureter or urethra by a stone;
- stone removal; preventing stagnation of urine in the genitourinary organs and the development of infection.
There are drug treatments for urolithiasis, as well as surgery to remove stones from the urinary tract.
1) Conservative or drug therapy is aimed at eliminating pain, destroying and removing stones. To relieve a painful attack, antispasmodics are best suited.
2) Stone expulsion therapy will be effective in 80% of cases in the presence of stones no more than 6 mm in diameter. Along with drug therapy, therapeutic exercises are actively used to remove the stone. It is aimed at changing the position of the body in space. Therapeutic gymnastics is aimed at placing patients in special positions that facilitate the passage of stones through the urinary system.
3) Drug destruction of stones is effective only in the presence of urate stones. Therapy is aimed at eliminating the cause of stones - removing excess uric acid from the body. Unfortunately, this method is more preventive - it prevents the appearance of new stones rather than destroying existing ones.
4) The most effective treatment for urolithiasis is surgery to remove stones. During this procedure, stones of any morphological structure, any size and shape, and any location can be removed.
Postoperative period
An important part of treatment is metaphylaxis in the postoperative period. This is a set of measures that are aimed at removing invisible stones with a diameter of up to 0.5 mm and the remains of crushed stone. Metaphylaxis includes a drinking regimen of at least 3 liters of liquid per day, with control of daily diuresis in a volume of about 2 liters. In this case, special nutrition is prescribed with a reduction in the amount of table salt in the diet to 4.5 g/day. The amount of animal protein should also be limited - 0.8 g per kilogram of the patient’s body weight. In the postoperative period, it is recommended to eat easily digestible meat - boiled or steamed beef. Fried and fatty foods should be strictly excluded from the patient’s diet.
Throughout the postoperative period, the patient must actively engage in physical therapy, which will also facilitate the release of residual stone fragments. Each patient is prescribed an individual diet, which is selected depending on the morphological composition of the stone and the presence of changes according to the results of blood tests.
Effective treatment
Treatment of urolithiasis is a guarantee of receiving highly qualified medical care. Modern diagnostic methods at the Union Clinic multidisciplinary medical center in St. Petersburg allow us to conduct all necessary types of research. These include blood tests, urine tests (including the Nechiporenko urine test), as well as instrumental research methods.
To fully diagnose the presence of sludge and the absence of stones in the organs of the genitourinary system, the clinic has installed modern equipment that allows for ultrasound examination of the kidneys, ureters, and bladder. Patients also have access to X-ray examination methods, such as radiography of the abdominal and pelvic organs and excretory urography.
A complete examination of the patient allows highly qualified medical personnel to more accurately assess the patient’s condition and make the correct diagnosis. Moreover, preliminary studies inform the doctor about the size and shape of the stones and the functional state of the kidneys. This determines the scope of medical intervention.
To reduce the trauma that, one way or another, the body is exposed to when removing stones, experts recommend using conservative treatment. However, the approach to each patient is always purely individual. And the scope of intervention depends on the condition of the human body, the size, number and shape of stones, the presence or absence of complications.
Prevention of recurrent stone formation
- Preventing urolithiasis is the best way to prevent stones from appearing. It consists of fairly simple steps:
- treatment of chronic diseases of the body;
- treatment of diseases of the genitourinary system;
- playing sports 3 times a week;
- eliminating inactivity at work - changing posture and walking during breaks;
- therapeutic exercises in the postprenatal period;
- normalization of nutrition - eliminating fatty, excessively salty and sour foods from the diet;
- patients who have had urolithiasis must adhere to the diet prescribed by their doctor;
- determination of calcium and vitamin D levels at least once a year;
- preventive visits to a urologist every six months to a year;
- taking urine and blood tests every three months;
- undergoing an ultrasound examination of the genitourinary organs for people who have had urolithiasis every six months.
Such simple actions help to significantly reduce the risk of stones in the genitourinary system and get rid of all the troubles of this disease.
| Make an appointment | Make an appointment by calling +7 (812) 600-67-67 or filling out the online form - the administrator will contact you to confirm your appointment |
UNION CLINIC guarantees complete confidentiality of your request.
Prevention
Measures to prevent urolithiasis are the following:
- Consult a doctor if colic occurs even very rarely and does not particularly bother you. It is better to study the problem at the very beginning and prescribe effective treatment;
- undergo routine examinations if you have already had any urological diseases;
- eat healthy foods, reducing the amount of spicy, salty, fatty foods;
- eliminate or minimize alcohol consumption as much as possible;
- drink the daily amount of water, do not violate the drinking regime. The water must be of high quality, purified through a filter;
- move every day, devote time to physical activity.
These simple recommendations for the prevention of urolithiasis will help significantly reduce your risks.
Drug treatment
The use of medications is primarily aimed at relieving pain in renal colic. Various antispasmodic and analgesic medications are prescribed.
There is another category of drugs used in treatment - these are drugs that help dissolve stones. They are prescribed based on the chemical composition of the stones. Again, this treatment regimen is only possible if the patient is diagnosed with stones, a condition of uric acid derivatives. All other stones cannot be dissolved with medications, so surgical treatment is performed.
Surgery
When choosing surgical treatment, preference should be given to the least traumatic methods. There are two types of operations - endoscopic and laparoscopic. The essence of endoscopic surgery is to crush stones using medical instruments. Most often used:
- Cystolithotripsy. It is carried out for stones localized in the bladder. First, the stone is crushed, and then it is removed.
- Ureterolithotripsy. Used for stones in the ureter. To carry it out, a ureteroscope is used.
- Flexible retrograde nephrolithotripsy. Used to remove kidney stones (diameter at least 2 cm).
Laparoscopy is a modern surgical treatment method that involves performing surgery through small holes.
Urolithiasis is a serious pathological condition, so treatment is carried out immediately after the first symptoms are identified. It should be borne in mind that relapse is possible even after surgery. Therefore, long-term observation by a urologist is required, as well as following his recommendations.
Prevention involves changing your diet, excluding “junk” foods (fast food, processed foods), engaging in some kind of active hobby (especially during sedentary work), and drinking enough water per day.