Mononucleosis is an acute infectious disease that affects the lymphatic system. With mononucleosis, the throat hurts and becomes inflamed, the patient is constantly tired, restless, and has an enlarged liver and lymph nodes. Mononucleosis is characterized by an increase in monocytes in the circulating blood.
The source of infection is an infected person. The infection is transmitted by airborne droplets, often with human saliva (through kissing), and through blood transfusions.
50% of the population gets this infection in adolescence: girls at 14-16 years old, boys at 16-18 years old. People over 40 years of age are less likely to become infected with this disease. But in HIV-infected people, the disease can occur at any age.
Infectious mononucleosis (also called glandular fever, monocytic tonsillitis) is characterized by fever, lymphadenopathy, tonsillitis, an increase in the size of the liver and spleen, and can become chronic. The causative agent of the disease is the Epstein-Barr virus, EBV (a group of herpes viruses).
In addition to an increase in the size of the liver and spleen, the disease is manifested by abdominal pain, dyspepsia, and slight impairment of the functional abilities of the liver. In the first days of the disease, changes occur in the blood, leukocytosis, and an increase in mononuclear cells: lymphocytes and monocytes. ESR increases. Atypical cells with one nucleus of medium and large size appear - atypical mononuclear cells.
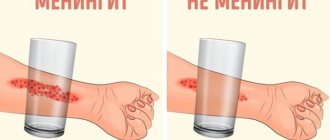
1
Throat examination
2 Examination of the throat
3 Throat examination
Symptoms of mononucleosis
Infectious mononucleosis is characterized by damage to the lymphoid tissue of the nose, pharynx, and tonsils.
Other symptoms of the disease:
- enlargement of the submandibular, axillary, elbow, inguinal, posterior cervical, tracheobronchial lymph nodes;
- a large number of wide-plasma monoculars;
- fever, swollen lymph nodes, tonsillitis;
- a sore throat;
- difficulty breathing through the nose;
- voice with a nasal tint, etc.
The disease is accompanied by follicular, lacunar or catarrhal sore throat, an unpleasant sweetish-sweet odor from the mouth.
Classification
According to the nature of the course, infectious mononucleosis is of two types:
- Typical, with characteristic symptoms and the presence of mononuclear cells in the blood.
- Atypical, occurring in a latent or low-symptomatic form.
Taking into account the duration of EBV, it is classified into 5 types, including:
- acute – symptoms persist for up to 3 months;
- protracted – from 3 months to six months;
- recurrent - symptoms appear again a month or less after recovery;
- chronic – the disease lasts more than six months.
Based on the severity of the course, there are mild, moderate and severe forms of EBV, as well as complicated and uncomplicated.
In addition, against the background of infectious mononucleosis, chronic diseases can worsen, and therefore EBV is distinguished with and without exacerbation of chronic diseases.
Pathogenesis of mononucleosis
The Epstein-Barr virus appears in the human body through the mucous membranes of the nasopharynx, then spreads throughout the body and accumulates in the lymph nodes. The virus is supported by B lymphocytes that have surface receptors for the virus.
At the very peak of the disease, specific viral antigens can be detected in more than 20% of the nuclei of B lymphocytes.
When the infectious process has subsided, mononucleosis viruses are observed only in single B-lymphocytes and epithelial tissues of the nasopharynx. When some of the affected cells die and the released virus infects new cells, cellular and humoral immunity begins to malfunction. Therefore, a super-infection may form and a secondary infection may develop (most often caused by staphylococci or streptococci).
In mononucleosis, the virus affects the lymphoid and reticular tissue, this leads to enlargement of the lymph nodes, and the liver and spleen also enlarge.
Immunity against mononucleosis is stable. The infection can spread in the form of asymptomatic and erased forms; antibodies to this virus are found in 50-80% of the population.
Infectious mononucleosis in children: what kind of disease it is, its signs, symptoms and treatment
Disease statistics
If a child often experiences diseases of the upper respiratory tract, this indicates reduced immunity. The immune system prevents the penetration of viral and bacterial infections, and its weakening opens the way for pathogens to enter the body. In the article we will talk about infectious mononucleosis in children, what kind of disease it is, what symptoms appear, how treatment is prescribed, and also show a photo of the throat at the initial stage.
The second name that has spread among doctors is “disease of the young.” It is called that because the majority of those infected are people under the age of 35. Accordingly, a large proportion of them are young patients with fragile bodies and increased curiosity about the world around them. Due to the child’s lack of personal space boundaries, children often use other people’s personal hygiene products and may not wash their hands after using the toilet or walking outside. Pathogens enter by airborne droplets.
For adults, the virus is not so dangerous, since, according to statistics from the Ministry of Health, about 90% of the population is resistant to the pathogen because they were ill in childhood.
Epidemics begin in the autumn-winter period. Although the patient could have become infected in the summer, for example, while swimming in a pond. But the immune system increases the incubation period of the infection, and with the onset of cold weather it weakens, allowing the first symptoms to appear. It is for this reason that in the fall it is imperative to give children the immunomodulator “Cytovir-3” in the form of a syrup or suspension for children over one year old or in capsules for children over 6 years old.
Infectious mononucleosis in a child - what is it?
The inflammatory process is also called:
- benign lymphoblastosis;
- Filatov's disease;
- "kissing disease"
In the medical literature, the disease is assigned an ICD 10 code: B27.
This is an acute infectious inflammation caused by the Epstein-Barr virus. The pathogen enters the body through the respiratory tract or mucous membranes. It may lie dormant for a short time in the latent stage, and then manifest itself, affecting the pharynx, larynx, nasal cavities, disrupting the functioning of the spleen and kidneys, changing the composition of the blood. The appearance of atypical mononuclear cells in the blood supply leads to widespread distribution in the body and possible manifestations on the skin in the form of pustules or abscesses.
Signs can manifest themselves as a severe cold or sore throat, and if the level of immune response is very good, then they go almost unnoticed. But at the age of 13 to 16 years, when a hormonal surge occurs and all the corresponding changes in the body, protective functions are usually weakened, then the patient will feel severe symptoms.
Epstein-Barr virus is considered one of the subtypes of herpes infection, therefore inf. mononucleosis in children can, like herpes, be transmitted to the body through the mother, as well as any other close contacts. The main impact that the pathogen has is focused on:
- lymphoid tissue - therefore the lymph nodes become significantly inflamed, first the cervical ones, and then all the others;
- blood flow - in addition to the appearance of atypical mononuclear cells, changes in leukocytes and lymphadenopathy are expressed.
Routes of transmission
The method of penetration of the pathogen into the body is airborne droplets. The pathogen enters the mucous membrane (of the nose, if infection occurred through inhalation, or the oral cavity, if there was contact through saliva), creates an inflammatory process in the nasopharynx, and then is absorbed into the blood. Together with blood elements, it first reaches local lymph nodes, and then descends to vital organs. When Epstein-Barr attacks the liver and spleen, they, in turn, increase in size, which an experienced doctor will easily notice on an ultrasound or even by palpation during the diagnostic process.
The disease viral mononucleosis in children can be obtained if the child:
- do not observe the rules of personal hygiene;
- be in the same room with an infected person;
- have close contact with a carrier of infection;
- go out into public places during epidemics;
- use the patient’s personal belongings – dishes, cutlery, towels.
Is it possible to get sick a second time?
Formally, the patient always remains sick after the first contact, because the virus does not go away, but is only stopped by developing its own specific immunity to the pathogen. You can experience similar symptoms only if the pathogen mutates.
Cases of relapse have been recorded in adults diagnosed with HIV infection. Their protective functions of the body as a whole are very weakened, so for them the disease suffered in adolescence can become significant when it reappears.
Causes of mononucleosis infection in children
We have already spoken about external influence. Epstein-Barr is transmitted through the air. But in open conditions, especially in winter at sub-zero temperatures, it does not live long. A warm environment and a short stay in the atmosphere are acceptable for it. Thus, you can only become infected indoors with fairly close contact - tactile or through communication.
The biggest breeding ground for infection is kindergarten. It is here that kids constantly catch the disease, which is understandable. If the child did not get sick in kindergarten, then a threat awaits him at school. You shouldn’t be too afraid of this, but you should be given a disposable medical mask if an epidemic breaks out, or even give a couple of days of rest.
Transmission method - various contacts:
- sneezing and coughing;
- kisses;
- eating with one spoon or drinking from one glass.
The manifestation of symptoms is less common for girls; according to statistics, boys get sick 2 times more often, but representatives of the fairer sex can be carriers.
When infected, the first signs of mononucleosis in children appear after 7-10 days. During this period, infection seeps into the bloodstream, causing inflammation and enlargement of internal organs.
The duration of the disease in some cases can reach one or one and a half months. This is due to late consultation with a doctor and a low level of immune protection.
The following forms are distinguished:
- atypical - it’s bright, sharp - can appear quickly, but usually goes away in a short period of time;
- chronic - the clinical picture is blurred, the disease progresses sluggishly, as do the symptoms, but the baby may feel unwell for a long time.
Symptoms of infectious mononucleosis in a child
If contact with an infected person occurs, the first signs may appear within 5 days. If this does not happen in the next two weeks, then we can talk about a good immune system and an asymptomatic disease. Since there is no vaccine or special preventive measures, there is only one piece of advice for parents - throughout the year they need to strengthen the baby’s immunity. Already from the first year of life, when the mother stops breastfeeding, Cytovir-3 should be given in syrup or suspension. This product is sold without a prescription, it is absolutely safe and recommended for use from 12 months. The course consists of only 4 days, but such prevention will help not to become infected with mononucleosis.
But if the infection has already settled in the body, then there will be the following symptoms of atypical mononucleosis in children:
- increased body temperature - fever in acute form or with complications can reach 39.5 degrees;
- fever and chills;
- active sweating, cold and sticky sweat;
- rash, redness of the skin, the appearance of small lesions on the arms, back, abdomen;
- general weakness, drowsiness;
- enlargement and tenderness of the cervical lymph nodes;
- sore throat, red mucous membrane of the larynx, swelling;
- nasal congestion due to vasodilation and swelling of the nasal ducts;
- inflammation and increase in the size of the tonsils;
- headache and dizziness;
- loss of appetite.
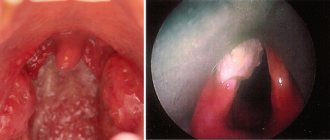
The pharynx looks the same as with catarrhal tonsillitis, hyperemia of the mucous membranes appears, that is, accumulation of blood in the vessels, followed by granular redness.
When treating mononucleosis in a child, you should not pay special attention to the rashes on the skin - they do not itch, and with recovery they will go away on their own. But if itching appears, then this may become a symptom of the development of an allergic reaction, then antihistamines will be needed.
The main symptom is inflammation of the lymph nodes, which is called polyadenitis. At first, the inflammation affects only the cervical lymph nodes, this can be felt and detected independently, since when turning the head a feeling of discomfort will appear. Then the inflammatory process will begin in the abdominal lymph nodes, they, in turn, press on the peritoneum and can cause acute pain in the abdomen.
A small yellowish coating may form on the tonsils. It also does not require special care and will go away along with the main manifestations.
Diagnosis of the disease
For the doctor, not only external symptoms are important, but also the condition of the internal organs - the liver and spleen, which increase in size, as can be seen on ultrasound. After a routine examination of the oral cavity, palpation of the abdomen and lymph nodes, the specialist prescribes the following procedures:
- Blood test - may contain antibodies that indicate the presence of the Epstein-Barr virus.
- Biochemistry.
- Ultrasound of internal organs.
The doctor will then prescribe medication.
How and with what to treat infectious mononucleosis in children
Therapy mainly takes place at home; hospital care is rarely prescribed, only in severe cases, for example, if the baby is very small. Hospitalized in the following cases:
- when complications appeared;
- fever more than 39.5 degrees;
- labored breathing;
- severe dehydration or other manifestations of increased intoxication.
Treatment is generally prescribed symptomatically, since there is no antiviral drug that would kill the pathogen, the Epstein-Barr virus. Home remedies are also used in combination with medications, but only after being prescribed by a specialist.
How to treat mononucleosis in a child with medications
- Antipyretics based on paracetamol - they are softer than their analogues, they are taken only after the mark on the thermometer is exceeded 38 degrees. Until this period, the body must fight on its own.
- Antiperspirants with an antiseptic agent, sprays should be sprayed on the tonsils so that a focus of infection does not develop there.
- Boosting your immunity with the help of Cytovir-3 - a four-day course will help you cope with the virus in a short time and without exacerbations or complications.
- Choleretic medications. They are introduced into therapy when there is a significant enlargement of the liver.
- Antibiotics will help when the inflammatory bacterial process in the nasopharynx is actively manifested with the appearance of mucus on the tonsils, bad breath, and a runny nose.
- Probiotics – come complete with antibacterial drugs. Other remedies may be needed depending on the symptoms, for example, if redness on the skin begins to itch, then perhaps this is a reason to start antihistamines.
Prevention of mononucleosis in children
To avoid getting infected, you need to follow simple rules:
- Eat a large amount of fortified foods - vegetables, fruits, fish and meat, rich in protein.
- Do not leave home during epidemics without an individual protective medical mask.
- Wash your hands before eating and after visiting public places.
- Do not come into close contact with infected people.
- Maintain the immune system at a high level: harden yourself, play sports, take the immunomodulator Cytovir-3.
It is also worth taking walks in the fresh air more often with your child, sending him to a sports section, monitoring the environmental situation in his place of residence, as well as keeping his home in order. It is worth frequently doing wet cleaning and ventilating the room, especially the baby’s bedroom.
Diet No. 5
Young patients should adhere to a certain menu. It is designed specifically for those who need to restore the functions of the liver and spleen, as well as strengthen their strength after illness.
Main taboos:
- less fatty foods;
- fried, salted, smoked;
- chilled food;
- products that contain coarse fiber - it provokes bloating.
Appointed:
- low salt intake;
- clean water on an empty stomach;
- 4-5 meals a day.
In the article, we explained why mononucleosis is dangerous in children and how to treat it. Strengthen your child's immunity with Tsitovir-3.
How does the disease progress?
The incubation period for mononucleosis is about a week. The disease begins acutely. Days 2-4 are characterized by pronounced fever and general intoxication of the body.
From the first days a person feels weakness, headache, and a little later pain appears when swallowing. The temperature rises to 38 - 40 degrees. On day 5, the patient may develop tonsillitis. It can be catarrhal, lacunar or ulcerative-necrotic. Lymph nodes are affected. A rash may appear on the body, which disappears without a trace after 1-3 days. Changes in the liver are observed.
Leukocytosis can be observed in peripheral blood. The number of lymphocytes, monocytes and atypical mononuclear cells reaches 80-90% in the first week. After mononucleosis, the mononuclear reaction can last from six months to several years.
There are several possible outcome options for the acute infectious process of EBV (mononucleosis):
- recovery;
- asymptomatic virus carriers;
- chronic recurrent infection (chronic infectious mononucleosis);
- development of the oncological process (lymphoma, nasopharyngeal carcinoma, leukoplakia of the tongue and oral cavity, stomach and intestinal cancer);
- development of an autoimmune disease (rheumatoid arthritis, systemic lupus erythematosus ).
Epidemiology
The source of infection is a person with acute and chronic manifest or latent forms of EBVI. Infected individuals actively shed the virus from the last days of incubation and for 6-18 months after the initial infection. More than 90% of asymptomatic seropositive individuals harbor the virus in oropharyngeal secretions.
The main transmission mechanism is airborne, the transmission route is aerosol. EBV is mainly transmitted through direct close contact through saliva (kissing, toys with contaminated saliva) containing oropharyngeal epithelial cells. Infection is possible if sanitary and hygienic rules for handling utensils in the public catering system are not followed, as well as when using “shared” glasses, bottles, etc. Parenteral (during organ transplantation and blood transfusions) and sexual transmission are also possible. The possibility of vertical transmission of the pathogen with the development of congenital EBVI has been established. EBV is transmitted through blood transfusions and transplants. The entire non-immune population is susceptible to infection, regardless of age.
Complications after illness
Complications after infectious mononucleosis are not very common, but quite serious:
- hematological complications (autoimmune hemolytic anemia, thrombocytopenia, granulocytopenia);
- splenic rupture;
- neurological complications (encephalitis, paralysis of facial muscles, polyneuritis, transverse myelitis, psychosis);
- hepatitis;
- cardiac complications (pericarditis, myocarditis);
- complications of the respiratory system (interstitial pneumonia, airway obstruction).
1 Consultation with an otolaryngologist in MedicCity
2 Consultation with an otolaryngologist in MedicCity
3 Consultation with an otolaryngologist in MedicCity
Diagnosis of mononucleosis
Diagnosis of EBV and mononucleosis includes:
- examination by an otorhinolaryngologist, therapist, immunologist, infectious disease specialist;
- Ultrasound of lymph nodes, abdominal cavity, spleen;
- laboratory tests: clinical blood test, biochemical blood test, immunological examination to assess antiviral protection, serological tests (a criterion for the presence of the virus at the present time), DNA diagnostics using the PCR method.
1 ENT consultation in MedicCity
2 Laboratory diagnostics in MedicCity
3 Ultrasound of lymph nodes in MedicCity
Treatment of mononucleosis
Treatment of mononucleosis, if the course of the disease is uncomplicated and the patient is isolated, can be carried out at home. Treatment of patients with EBV with a complicated form of infection must be carried out in a hospital! For mononucleosis, restorative and symptomatic treatment is used. The patient is recommended to take vitamins C, P, and group B. At elevated temperatures, antipyretics are prescribed. Antibiotics for mononucleosis are prescribed in case of a secondary infection affecting the tonsils.
At the MedicCity multidisciplinary clinic, you can consult with highly qualified otolaryngologists and receive the necessary recommendations for various diseases of the ear, nose and throat. Remember that the disease is easier to cure in the early stages of development!
Causes and causative agent
The causative agent of MI is the Epstein-Barr virus (EBV) - a large enveloped DNA virus of type 4 from the family Herpesviridae, subfamily of Herpesviridae, genus Lymphocryptovirus.
Based on differences in the structure of the genome and the ability to cause a blast transformation reaction of B-lymphocytes, 2 strains of EBV are distinguished: the most active type 1(A) in the reaction and the less active type 2(B). Type 1(A) is widespread, type 2(B) is found mainly on the African continent and several countries in North America.
EBV has an oval shape with a diameter of 150-200 nm. The virus genome is represented by two DNA molecules enclosed in an icosahedral capsid consisting of 162 capsomers. The complex of virus capsid proteins (p150, p18, p23) is represented by its capsid antigen - VCA (Viral capsid antigen). The immunodominant proteins in this complex are p18 and p23.
At the earliest stages of EBV replication, a highly immunogenic complex of viral proteins (p54 and p138), called the early EA antigen, appears in the body of an infected person.
The targets for EBV are cells that have the CD21 receptor on their surface. These are epithelial cells of the mucous membranes of the nasopharynx and oropharynx, excretory ducts of the salivary glands; B-lymphocytes (primarily located in the follicular structures of the Pirogov-Langans lymphoid ring and peripheral lymphoid tissue); dendritic cells; epithelium of the cervix.
To learn more
|
The immunosuppressive effect of EBV, on the one hand, causes long-term (lifelong) persistence of the virus in the body with the possibility of periodic exacerbations of the disease, on the other hand, it explains the possible role of the virus in the development of immuno- and oncopathology. The virus is unstable to environmental factors and quickly dies under the influence of disinfectants when dried at room temperature.
EBV is extremely thermolabile - it “dies” at a temperature of 50-52°C for 30 minutes, at a temperature of 37.5°C for 20 hours, and is stable at a temperature of minus 70°C; tolerates lyophilization well and is stored in tissues for a long time in a 50% glycerol solution. On metal surfaces (coins, door handles, water taps) EBV survives for 2 hours, on plastic and wood - up to 3 hours, in damp medical cotton wool and gauze - until they dry at room temperature - up to 6 hours.