MAKING AN APPOINTMENT WITH A DOCTOR IN ST. PETERSBURG
+7 or +7
Ulcerative colitis, or nonspecific ulcerative colitis (UC)
IBD is a chronic autoimmune inflammatory bowel disease (IBD) that causes ulcers in the human digestive tract. Ulcerative colitis affects the intestinal mucosa, its deepest layers, which leads to blood loss, dehydration, loss of iron, magnesium, potassium, calcium, and exhaustion of the body. Ulcerative colitis usually develops in people under 30 years of age, equally in both sexes.
One of the reasons for the appearance of ulcerative colitis is a malfunction of the immune system, when it gives an abnormal response to attempts to invade the infection. As a result of this abnormal response, cells in the digestive tract are affected, leading to lesions of ulcerative colitis. The autoimmune process in ulcerative colitis also causes arthritis, conjunctivitis, chronic hepatitis, and erythema nodosum.
Ulcerative colitis can cause life-threatening complications such as:
- toxic megacolon,
- colon perforation,
- colorectal cancer
, - bleeding or thrombosis;
- pyoderma gangrenosum.
Clinical symptoms of ulcerative colitis
At the initial appointment, the gastroenterologist conducts a survey of the patient, clarifying the presence of clinical symptoms typical for ulcerative colitis. Adult patients may present with one or more symptoms that are highly likely to indicate ulcerative colitis, including:
- recurrent diarrhea, which cannot be cured by conventional remedies;
- rectal pain and rectal bleeding (bloody stools);
- abdominal pain and cramps (mainly before bowel movements);
- tenesmus (false urge to defecate);
- nocturnal stools awakening from sleep;
- urgency (fecal incontinence);
- fever of unknown etiology, weight loss, general weakness;
- joint pain and other extraintestinal symptoms (skin lesions in the form of red, bumpy, painful rashes, inflammation of the eyes, discomfort and pain in the lumbar region, etc.).
In young patients, parents should suspect something is wrong if the child is not eating well, is not active enough, is losing weight, and is stunted. Children's stool is also unformed.
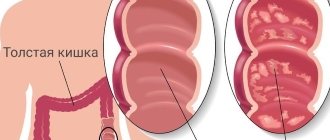
Types of Ulcerative Colitis
Montreal classification according to the extent of the lesion:
- Proctitis
, in which the source of inflammation is located in the rectum, closer to the anus. In this case, the only symptom that may indicate the disease is rectal bleeding. - Left-sided colitis
, including
proctosigmoiditis
. In this form of ulcerative colitis, inflammation extends from the rectum up to the left (splenic) flexure of the colon, affecting the sigmoid colon and often the descending colon. Symptoms of left-sided colitis include bloody diarrhea, abdominal cramps and pain on the left side, and a urge to defecate (tenesmus) that does not lead to a bowel movement. - Total colitis
, or
pancolitis
. It is characterized by inflammation of the entire colon. Signs of pancolitis include frequent bouts of bloody diarrhea, cramping abdominal pain, anemia due to bleeding, and significant weight loss.
general description
Ulcerative colitis or nonspecific ulcerative colitis is a chronic inflammatory disease of the mucous membrane of the large intestine, resulting from an imbalance of the immune system (antibodies are released to the own epithelium of the mucous membrane).
Cases of morbidity are registered in 0.3-0.5% of people, which is approximately 3-5 cases per 100 thousand population. The disease occurs in both men and women.
Ulcerative colitis can affect people of any age, most often occurring in the 25-35 and 60-80 age groups.
The nature of the course of ulcerative colitis
- Acute course
(less than 6 months from the onset of the disease):- a disease with a fulminant (sudden and rapidly developing) onset;
- a disease that develops gradually.
- Chronic continuous course
(absence of more than 6-month periods of remission against the background of adequate therapy). - Chronic relapsing course
(presence of more than 6-month periods of remission):- rarely recurrent (once a year or less);
- often recurrent (2 or more times a year).
Screening and diagnosis of ulcerative colitis
stool test for calprotectin is used as a screening
. With fecal calprotein (FC) values below 50 mcg/g, the probability of having an active inflammatory disease in the intestine (ulcerative colitis or Crohn's disease) is less than 1%, and with a value above 150 mcg/g, it makes sense to carry out a differential diagnosis of ulcerative colitis.
There are no clear diagnostic criteria for ulcerative colitis. The diagnosis is made on the basis of anamnesis, clinical picture, laboratory results, endoscopic and histological changes in the intestine.
Stool tests
- General analysis of stool (coprogram)
. The doctor will prescribe a coprogram to assess the functional capacity of the gastrointestinal tract. In addition, a large number of leukocytes in the stool indicates an inflammatory process in the intestines, caused, as an option, by ulcerative colitis. A stool test from a patient with ulcerative colitis usually shows blood, pus, and mucus. - Fecal calprotectin (FC)
. During the initial diagnosis and/or to assess the activity of the inflammatory process, a study of the FC level is required. FC is also a reliable marker for assessing the effectiveness of UC treatment. - Fecal occult blood test (Gregersen test)
. Examination of feces for occult blood allows one to suspect the earliest stages of ulcerative processes. The analysis makes it possible to detect altered hemoglobin in erythrocytes even if the erythrocytes themselves are not detected during microscopic examination of stool. - Fecal tests for helminth eggs
. A standard stool test for worm eggs will help rule out enteritis and colitis of a parasitic nature, or at least avoid complications. - Smear for pathogenic microflora
. During bacteriological tests, the presence of Shigella, Salmonella, Yersinia, Campylobacter, and tubercle bacilli is determined. Pathogenic microflora is often sown in the stool of patients with ulcerative colitis. - Stool analysis for amebodiasis (optional).
According to WHO, about 10% of people on Earth are carriers of dysentery amoebas, mainly residents of countries with hot climates (Mexico, India, etc.). Dysenteric amoebas can cause prolonged diarrhea with pathological impurities in the stool, abdominal pain, dehydration, which can ultimately lead to death. Tell your doctor if you have returned from southern countries. - Determination of toxins A and B (optional)
. Patients who have undergone a course of antibiotics and/or hospital treatment are prescribed a stool test for clostridial toxins. The analysis will exclude/identify pseudomembranous colitis caused by this hospital infection, which can negate all treatment.
Blood tests
- General blood analysis
. The analysis is necessary for the doctor to evaluate the metabolic disorders that often accompany ulcerative colitis (anemia, hypoproteinemia, electrolyte imbalance), systemic disorders (changes in blood composition and coagulation). A low number of red blood cells and hemoglobin will indicate anemia, an increased level of platelets (>350*109/l) will indicate activation and progression of the disease, the risk of thrombolic complications, and an increased level of leukocytes will indicate chronic inflammation and poisoning of the body with endotoxins. It is assumed that endotoxemia is involved in the pathogenesis of ulcerative colitis, Crohn's disease, and colorectal cancer. - Erythrocyte sedimentation rate (ESR)
. An increase in ESR is an indirect sign of current inflammation. For example, with a moderate form of ulcerative colitis, the ESR reaches 30 mm/h. In severe cases, this figure is even higher. With increasing endoscopic activity of the disease and the extent of the lesion, the ESR also increases. - C-reactive protein (CRP)
. Protein of the acute phase of inflammation naturally increases in inflammatory bowel diseases. A slight increase or normal levels are characteristic of nonspecific ulcerative colitis, high levels are characteristic of Crohn’s disease with similar symptoms. Due to the property of CRP to rapidly decrease during remission, the study allows us to evaluate the effectiveness of treatment. - Biochemical blood test: ALT and AST, total bilirubin, total protein, glucose, total cholesterol, creatinine, urea, electrolytes
.
Additionally, the doctor may prescribe biochemical blood tests for albumin
(for severe diarrhea),
iron
(for anemia). A biochemical blood test is included in the “clinical minimum”, allowing one to assess the involvement of other organs (liver, kidneys) in the pathological process. A decrease in the level of total protein, glucose, cholesterol, and electrolytes (potassium, magnesium, calcium) helps determine malabsorption in the intestine. In addition, the results of the analysis for total protein will show a decrease in the concentration of albumin (less than <35 g/l) and an increase in the concentration of gammaglobulins, which is associated with the active production of antibodies. - Hemocoagulogram
. The presence of chronic inflammation and increased bleeding of the intestinal wall in ulcerative colitis initiates activation of the coagulation system, impairs the process of dissolution of blood clots and blood clots, and also reduces the activity of natural anticoagulation mechanisms. In turn, hypercoagulability may support the activation of the inflammatory response. The results of a coagulogram can identify various disorders in the blood coagulation system and break the vicious circle between chronic inflammation and thrombosis, as well as reduce the risk of bleeding and blood clots. - Immunological blood test pANCA and ASCA (optional)
. Detection of antibodies to the cytoplasm of neutrophils and to Saccharomyces (they appear due to an abnormal immune response) can be useful in the differential diagnosis of UC with Crohn's disease. p-ANCA are present more often in ulcerative colitis, and ASCA are more often present in Crohn's disease. Under the influence of antibodies, neutrophils are destroyed, which promotes inflammatory reactions, and as we remember, ulcerative colitis has a specific autoimmune nature of the disease. But not all people with Crohn's disease or ulcerative colitis have elevated levels of these antibodies.
Urine tests
A general urine test is necessary to assess the involvement of other organs in the pathological process. Ulcerative colitis is caused by immune disorders, and these same disorders can cause kidney damage and the formation of kidney stones.
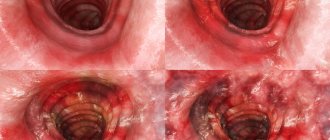
Endoscopic studies
When diagnosing IBD, the following types of endoscopy may be prescribed:
- Colonoscopy
is an endoscopic examination of the entire colon (1.5 meters) using a flexible long endoscope. - Sigmoidoscopy
is a more gentle endoscopic examination of the rectum and lower parts of the large intestine (sigmoid colon). A sigmoidoscope is a short colonoscope (50-60 cm). - Rectoscopy
is an endoscopic examination of the rectum and the distal third of the sigmoid colon to a level of 20-35 cm from the anus using a tube rectoscope. - Gastroscopy
is an endoscopic examination of the stomach and duodenum.
rectoscopy is performed first.
with multiple biopsies. The procedure is gentle and does not require special preparation. The doctor inserts a rigid tube, usually no more than 35 cm long, into the rectum and assesses the condition of the intestinal mucosa, vascular network, the presence of ulcers, erosions and narrowing of the lumen. Modern sigmoidoscopes can be equipped with a fiber-optic video system and a device for taking biopsies and removing tumors. Colonileoscopy (total colonoscopy with examination of the sigmoid colon) is postponed until the condition has stabilized.
The most informative method of endoscopic examination, as you may have guessed, in patients with intestinal problems is colonileoscopy
.
With this method, the rectum, colon and ileum are examined using a thin flexible tube. A camera with an LED is installed at the end of the probe, and a fiber-optic cable is built into the tube itself, through which the image is transmitted to the doctor’s computer. The study is carried out in real time under anesthesia. Colonoscopy is contraindicated for patients with active inflammation and acute intestinal complications
, therefore, despite the high information content of the method, it is not always prescribed (mainly when the issue of surgical treatment of ulcerative colitis with removal of the colon is being decided).
If there are symptoms from the upper gastrointestinal tract and doubts about the diagnosis, the doctor may prescribe gastroscopy with biopsy
.
Histological studies
In case of initial diagnosis, doubts about the correctness of a previously made diagnosis, or with a long history (to exclude dysplasia and colorectal cancer), a biopsy of tissue from the mucous membrane of the rectum, colon and/or ileum is taken during an endoscopic examination and sent for histology. Histological examination of a biopsy (a piece of intestinal mucosa taken during an endoscopic examination) usually allows one to finally determine the diagnosis.
Radiography
X-ray examinations of the colon are carried out when endoscopic examination is impossible or insufficiently informative (for strictures, deformities of the colon). There are also two types of X-ray studies:
- X-ray of the large intestine with contrast.
As an alternative, your gastroenterologist will primarily suggest this option, also known as
double-contrast barium enema
. On the eve of the study, the patient takes a laxative and undergoes cleansing enemas. Immediately before the test, the patient will receive an enema with a contrast agent containing barium. The solution settles on the walls, which makes it possible to examine the relief of the mucosa. After a bowel movement, air is injected into the bowel to inflate it, and x-rays are taken again. The resulting images can reveal areas of inflamed and ulcerated colon mucosa, as well as narrowing and dilation. - Plain radiography of the abdominal cavity.
In case of a severe attack, to exclude toxic dilatation (megacolon) and perforation of the colon, the doctor may prescribe a plain radiography of the abdominal cavity. No special preparation is required. - X-ray of the chest organs.
When deciding whether to prescribe biological therapy. Alternatively, the doctor may prescribe the Mantoux test, Diaskin test or Quantiferon test.
Ultrasound examinations
If everything is so bad that the injection of contrast is contraindicated for the patient, in the arsenal of modern doctors there is a transabdominal ultrasound of the intestine, ultrasound of the abdominal organs, ultrasound of the retroperitoneal space, ultrasound of the pelvis
. You don’t even need indications to undergo an ultrasound: it is advisable for everyone to undergo it as a screening test. Ultrasound has low specificity in differentiating ulcerative colitis from colitis of other origins (and therefore is not a first-line study), but the inflammatory process in the intestine will show.
In everyday practice, simple criteria will help the doctor determine the severity of the disease with a confirmed diagnosis (mild, moderate or severe): frequency and consistency of stool during the last exacerbation, temperature, pulse, blood test results, the presence of extraintestinal manifestations and complications, the presence of hormonal dependence or resistance to medications.
In order to clarify the diagnosis and select therapy for extraintestinal manifestations of UC and concomitant diseases, consultation with the following specialists may be required:
- endocrinologist
(steroid diabetes mellitus, adrenal insufficiency with long-term hormonal therapy); - dermatologist
(differential diagnosis of erythema nodosum, pyoderma); - rheumatologist
(arthropathy, sacroiliitis); - surgeon
(toxic dilatation of the colon; severe attack or bleeding that does not respond to conservative therapy, continuous course of the disease); - oncologist
(dysplasia of the intestinal mucosa).
What is the range of possible surgical interventions?
The range of surgical interventions in case of ineffectiveness of drug treatment and diet for nonspecific ulcerative colitis includes several types of operations. In our clinic you can receive high-quality treatment, whatever the causes of UC and its consequences in a particular case. Doctors will choose the most appropriate type of intervention for each patient. One operation is enough to completely eliminate the disease.
Sometimes the doctor will consider removing the colon while preserving the rectum and anus. At the same time, holding the chair is maintained. The disadvantage of this method is that it maintains the risk of developing colitis and cancer in the remaining part of the rectum.
Treatment of ulcerative colitis
Conservative therapy (drugs)
A cure for ulcerative colitis has not yet been invented, but doctors have successfully put this disease into remission with anti-inflammatory drugs 5-aminosalicylic acid: sulfasalazine or mesalazine. Sometimes - in combination with hormonal drugs: prednisolone, dexamethasone. Hormones are used to treat ulcerative colitis when 5-ASA drugs are not effective enough or when the attack is severe. It should be noted that in severe attacks of ulcerative colitis, the patient should be treated in a hospital. Microenemas, rectal suppositories, antibiotics, etc. can also be used in the treatment of ulcerative colitis.
Hormonal drugs do not heal the colon mucosa, but only reduce the activity of exacerbation of ulcerative colitis. The goal of conservative therapy in the treatment of UC is the emergence of stable remission with cessation of glucocorticoids. The non-operated patient must constantly take maintenance therapy to avoid relapse.
Surgery
Complete cure of ulcerative colitis is possible by removing the substrate of the disease (colproctectomy). Despite the effectiveness of drug therapy, surgery will still be needed sooner or later, and it is better not to delay it. Surgery will be required if the patient has hormonal dependence or resistance to treatment. Up to 80% of these conditions can be overcome with drugs that suppress the immune system.
Intestinal complications that require emergency surgery in any case include: intestinal bleeding, deep ulcerations, toxic megacolon, colon perforation, colorectal cancer or a high risk of its occurrence.
Diagnostics
Mandatory:
- general and biochemical, immunological blood tests. Signs of inflammatory changes, anemia, and an increase in the number of immune complexes are detected;
- stool examinations for pathogenic intestinal microflora (bacteria culture), analysis for helminthic infestations. Necessary to exclude diseases with similar manifestations - dysentery, amoebiasis, helminthiases;
- PCR of stool, detection of antibodies in the blood - also to exclude bacterial and protozoal infections;
- FCC. Fibroileocolonoscopy is the most informative method of examination for ulcerative colitis. During the examination, samples of changed tissues are taken (biopsy). Based on the results, a final diagnosis is made. The study allows us to exclude Crohn's disease, malignant tumors, etc.
According to indications, to establish a diagnosis of ulcerative colitis and assess the depth and area of the lesion, you may need:
- CT or MRI of the abdominal cavity;
- Rhography of the intestine with contrast (clarifies the presence or absence of intestinal perforation);
- Detection of the level of fecal calprotectin in the stool is a new method for determining the degree of inflammatory changes in the intestine, helping to exclude irritable bowel syndrome (IBS) in the diagnosis of UC. It also allows you to evaluate the effect of treatment for ulcerative colitis.