Losartan canon 50 mg 30 pcs. film-coated tablets
pharmachologic effect
Antihypertensive drug.
Selective angiotensin II receptor antagonist (type AT1). Angiotensin II is a powerful vasoconstrictor, the main active hormone of the RAAS, and also a decisive pathophysiological link in the development of arterial hypertension. Angiotensin II selectively binds to AT1 receptors found in many tissues (vascular smooth muscle, adrenal glands, kidneys and heart) and performs several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates the proliferation of smooth muscle cells. Losartan and its pharmacologically active metabolite (E-3174), both in vitro and in vivo, block all physiological effects of angiotensin II, regardless of the source or route of synthesis. Unlike some peptide angiotensin II antagonists, losartan does not have agonist effects. Losartan selectively binds to AT1 receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in regulating the function of the cardiovascular system. In addition, losartan does not inhibit ACE, which is responsible for the destruction of bradykinin. Therefore, effects not directly related to AT1 receptor blockade, including bradykinin-mediated effects and the development of peripheral edema (losartan - 1.7%, placebo - 1.9%), are not related to the action of losartan.
Reduces peripheral vascular resistance, blood concentrations of norepinephrine and aldosterone, blood pressure, pressure in the pulmonary circulation; reduces afterload and has a diuretic effect. Prevents the development of myocardial hypertrophy, increases exercise tolerance in patients with chronic heart failure (CHF). When losartan is taken orally, plasma renin activity increases, which leads to an increase in the content of angiotensin II in the blood plasma.
After a single dose, the antihypertensive effect (systolic and diastolic blood pressure decreases) reaches a maximum after 6 hours, then gradually decreases over 24 hours. During treatment, antihypertensive activity and a decrease in plasma aldosterone concentrations appeared after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. However, after replacing losartan, plasma renin activity and angiotensin II levels decreased after 3 days to the initial values observed before the start of the drug.
Both losartan and its active metabolite have a higher affinity for AT1 receptors than for AT2 receptors. The active metabolite is 10-40 times more active than losartan.
Composition and release form Losartan canon 50 mg 30 pcs. film-coated tablets
Tablets - 1 tablet:
- Active substance: losartan potassium 50 mg.
- Excipients: corn starch, croscarmellose sodium, mannitol, magnesium stearate, povidone, microcrystalline cellulose.
- Film shell composition: opadry white (hypromellose (hydroxypropyl methylcellulose), hyprolose (hydroxypropylcellulose), talc, titanium dioxide).
10 pieces. — cellular contour packages (3) — cardboard packs.
Description of the dosage form
White or almost white, film-coated tablets, round, biconvex; on a cross section it is almost white.
Directions for use and doses
The drug is taken orally, 1 time/day, in the morning (preferably at the same time), regardless of meals. The tablets should be swallowed without chewing and washed down with water.
For arterial hypertension, the initial and maintenance dose is 50 mg/day. If necessary, the daily dose can be increased to a maximum of 100 mg. If a single dose of the drug does not provide the target blood pressure level, the daily dose should be divided into 2 doses: 25 mg (losartan can be used in 25 mg tablets or scored 50 mg tablets) 2 times a day or 50 mg 2 times a day .
When prescribing the drug to reduce the risk of developing cardiovascular diseases and mortality in patients with arterial hypertension and left ventricular hypertrophy, the initial dose of the drug is 50 mg 1 time / day. In the future, hydrochlorothiazide may be added in low doses or the dose of Losartan Canon may be increased to a maximum of 100 mg in 1 or 2 doses, taking into account the reduction in blood pressure.
For chronic heart failure, the initial dose is 12.5 mg (it is possible to use losartan in tablets of 25 mg with a score) 1 time / day. The dose is titrated 2 times, depending on the patient’s tolerability of the drug, at weekly intervals, i.e. 12.5 mg/day, 25 mg/day, 50 mg/day up to an average maintenance dose of 50 mg/day.
In patients with type 2 diabetes mellitus with proteinuria, to slow the progression of renal failure, the initial dose is 50 mg 1 time / day with a further increase in the dose to a maximum of 100 mg / day (taking into account the degree of blood pressure reduction) in 1 or 2 doses.
In patients with reduced blood volume (for example, when taking diuretics in high doses), the recommended initial dose of Losartan Canon is 25 mg (it is possible to use losartan in 25 mg tablets or in scored 50 mg tablets).
In elderly patients with renal failure, no dose adjustment is required.
For patients with liver failure (less than 9 points on the Child-Pugh scale), during hemodialysis, as well as for patients over 75 years of age, a lower initial dose of 25 mg is recommended (it is possible to use losartan in 25 mg tablets or 50 mg scored tablets) 1 time/day
There is insufficient experience with the use of the drug in patients with severe liver failure, so the drug is not recommended in this category of patients.
In patients with moderate renal impairment (creatinine clearance 20-30 ml/min), no dose adjustment is required.
Pharmacokinetics
Suction
When taken orally, losartan is well absorbed from the gastrointestinal tract and is metabolized during the “first pass” through the liver by carboxylation with the participation of the CYP2C9 isoenzyme to form an active metabolite.
The systemic bioavailability of losartan is approximately 33%. Cmax of losartan and its active metabolite is achieved in the blood serum approximately 1 hour and 3-4 hours after oral administration, respectively. Food intake does not affect the bioavailability of losartan.
Distribution
Losartan and its active metabolite are more than 99% bound to plasma proteins (mainly albumin). Vd of losartan is 34 l. Losartan practically does not penetrate the BBB.
Losartan and its active metabolite demonstrate linear pharmacokinetics when administered orally in doses up to 200 mg. With a dosage regimen of 100 mg 1 time/day, there is no significant accumulation of either losartan or its active metabolite in the blood plasma.
Metabolism
Approximately 14% of a dose of losartan administered intravenously or orally is converted into its active metabolite. After oral or intravenous administration of losartan labeled with radioactive carbon 14C, the radioactivity of circulating blood plasma is due to the presence of losartan and its active metabolite. In addition to the active metabolite, biologically inactive metabolites are formed, incl. two major ones, formed as a result of hydroxylation of the butyl side chain, and one minor one, N-2-tetrazole glucuronide.
Removal
Plasma clearance of losartan and its active metabolite is about 600 ml/min and 50 ml/min, respectively. The renal clearance of losartan and its active metabolite is approximately 74 ml/min and 26 ml/min, respectively. When losartan is taken orally, about 4% of the dose is excreted unchanged by the kidneys and about 6% of the dose is excreted by the kidneys in the form of an active metabolite.
After oral administration, plasma concentrations of losartan and its active metabolite decrease polyexponentially with a final T1/2 of approximately 2 and 6-9 hours, respectively. Excretion of losartan and its metabolites occurs through the intestines with bile and kidneys. After oral administration of losartan labeled with radioactive carbon 14C, about 35% of the radioactivity is found in the urine and 58% in the feces. After intravenous administration of losartan labeled with radioactive carbon 14C, approximately 43% of the radioactivity is detected in the urine and 50% in the feces.
Pharmacokinetics in special groups of patients
Plasma concentrations of losartan and its active metabolite in elderly male patients with arterial hypertension do not differ significantly from the values of these parameters in younger male patients with arterial hypertension.
The values of plasma concentrations of losartan in women with arterial hypertension were 2 times higher than the corresponding values in men with arterial hypertension. Concentrations of the active metabolite did not differ between men and women. This apparent pharmacokinetic difference is, however, not clinically significant.
When losartan was taken orally by patients with mild to moderate alcoholic cirrhosis, the concentrations of losartan and its active metabolite in the blood plasma were 5 and 1.7 times, respectively, higher than in young healthy male volunteers.
Plasma concentrations of losartan in patients with creatinine clearance above 10 ml/min did not differ from those in individuals with unchanged renal function. When compared with the AUC in patients with normal renal function, the AUC of losartan in patients on hemodialysis was approximately 2 times greater. Plasma concentrations of the active metabolite did not change in patients with impaired renal function or on hemodialysis. Losartan and its active metabolite are not eliminated by hemodialysis.
Indications for use Losartan canon 50 mg 30 pcs. film-coated tablets
- Arterial hypertension;
- reducing the risk of developing cardiovascular diseases and mortality in patients with arterial hypertension and left ventricular hypertrophy;
- chronic heart failure (as part of combination therapy, with intolerance or ineffectiveness of therapy with ACE inhibitors);
- in patients with type 2 diabetes mellitus with proteinuria to slow the progression of renal failure, manifested by a decrease in the incidence of hypercreatininemia, the incidence of end-stage chronic renal failure requiring dialysis or kidney transplantation, mortality rates, and a decrease in proteinuria.
Contraindications
- Arterial hypotension;
- severe liver failure (more than 9 points on the Child-Pugh scale);
- primary hyperaldosteronism;
- simultaneous use with aliskiren in patients with diabetes mellitus and patients with renal failure (creatinine clearance less than 60 ml/min);
- pregnancy;
- lactation period (breastfeeding);
- age under 18 years (efficacy and safety have not been established);
- hypersensitivity to the active substance or to other components of the drug.
The drug should be prescribed with caution in cases of water-electrolyte imbalance (hyponatremia, hypochloremic alkalosis, hypomagnesemia, hypokalemia, hyperkalemia); decrease in blood volume; bilateral renal artery stenosis or stenosis of the artery of a single kidney; renal failure; condition after kidney transplantation (no experience of use); aortic and mitral stenosis; hypertrophic obstructive cardiomyopathy; heart failure with concomitant severe renal failure; severe chronic heart failure (IV functional class according to the NYHA classification); heart failure with life-threatening arrhythmias; IHD; cerebrovascular diseases; liver failure (less than 9 points on the Child-Pugh scale); history of angioedema.
Application Losartan canon 50 mg 30 pcs. film-coated tablets during pregnancy and breastfeeding
The drug Losartan Canon is contraindicated during pregnancy. At the same time, the degree of risk to the fetus in the first trimester is lower compared to the second and third trimesters, since renal perfusion in the fetus, depending on the RAAS, appears in the second trimester.
It is not recommended to prescribe the drug Losartan Canon in the first trimester. However, in those extremely rare cases (less than 1 in 1000 women) when the use of all other antihypertensive drugs is not possible, the drug can be prescribed under close medical supervision, including weekly fetal ultrasound. If signs of oligohydramnios are detected, treatment with an angiotensin II receptor antagonist should be discontinued.
The use of angiotensin II receptor antagonists in the second or third trimesters of pregnancy has a toxic effect on the fetus (decreased renal function, development of oligohydramnios, delayed ossification of the skull bones) and the newborn (renal failure, arterial hypotension, hyperkalemia).
Since drugs acting on the RAAS in the second and third trimesters of pregnancy can lead to impaired development and/or fetal death, if pregnancy is established, the use of the drug Losartan Canon should be stopped immediately.
For newborns and infants who were exposed in utero to an angiotensin II receptor antagonist, it is recommended to conduct careful monitoring for timely detection of a pronounced decrease in blood pressure, oliguria, and hyperkalemia.
It is unknown whether losartan is excreted in breast milk, therefore Losartan Canon is contraindicated during breastfeeding. If it is necessary to use the drug, breastfeeding should be stopped.
Use in children
The use of the drug in children and adolescents under 18 years of age is contraindicated.
special instructions
In patients with reduced blood volume (for example, receiving diuretics in high doses), symptomatic arterial hypotension may occur, therefore, before starting treatment, it is necessary to replenish the blood volume or begin treatment with Losartan Canon at a lower dose.
In patients with liver cirrhosis, the concentration of losartan in the blood plasma increases significantly, and therefore, in the presence of a history of liver disease, it should be prescribed in lower doses.
During the treatment period, potassium levels in the blood plasma and CK should be regularly monitored, especially in elderly patients, patients with impaired renal function, patients with type 1 diabetes mellitus complicated by nephropathy; These indicators should be monitored especially carefully in patients with heart failure with concomitant renal impairment.
Drugs that affect the RAAS may increase blood urea and serum creatinine concentrations in patients with bilateral renal stenosis or arterial stenosis of a solitary kidney.
There is no experience with the use of losartan in patients after kidney transplantation.
In patients with severe chronic heart failure, the use of drugs that affect the RAAS can lead to severe arterial hypotension and acute renal failure. There are isolated reports of the development of oliguria and/or increasing azotemia and acute renal failure, incl. with fatal outcome.
There is insufficient experience with the use of losartan in patients with heart failure with concomitant severe renal failure, in patients with severe chronic heart failure (NYHA functional class IV), in patients with heart failure with life-threatening arrhythmias. In these groups, the drug Losartan Canon should be used with beta-blockers with caution.
Like all drugs that have a vasodilating effect, Losartan Canon should be prescribed with caution to patients with aortic or mitral stenosis, or obstructive hypertrophic cardiomyopathy.
In patients with ischemic cerebrovascular diseases, an excessive decrease in blood pressure can lead to stroke. Medical supervision is recommended when titrating the dose.
Caution should be exercised when prescribing Losartan Canon to patients with a history of angioedema, incl. when taking other medications, including ACE inhibitors.
Patients with primary hyperaldosteronism usually do not respond to antihypertensive agents that act through RAAS inhibition. Therefore, it is not recommended to use the drug Losartan Canon to treat such patients.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted to evaluate the effect of the drug on driving vehicles and machinery. The possibility of drowsiness and dizziness should be borne in mind, so care must be taken when performing work that requires increased attention, especially at the beginning of treatment, when increasing the dose of the drug and when driving.
Overdose
Symptoms: excessive decrease in blood pressure, tachycardia. Bradycardia may occur due to parasympathetic (vagal) stimulation.
Treatment: forced diuresis, symptomatic therapy. Hemodialysis is not effective.
Side effects Losartan canon 50 mg 30 pcs. film-coated tablets
WHO classification of the incidence of side effects: very often - ≥1/10 prescriptions (>10%), often - from ≥1/100 to 1% and 0.1% and 0.01% and
From the hematopoietic system: rarely - anemia, thrombocytopenia.
From the nervous system: often - dizziness, headache, sleep disturbance, insomnia; uncommon - anxiety, drowsiness, memory impairment, peripheral neuropathy, paresthesia, hypoesthesia, migraine, tremor, ataxia, depression, syncope, acute cerebrovascular accident.
From the side of the organ of vision: infrequently - impaired visual acuity, conjunctivitis.
On the part of the hearing organ: infrequently - ringing in the ears.
From the cardiovascular system: often - palpitations, tachycardia, bradycardia, arrhythmia; infrequently - angina pectoris, orthostatic hypotension (dose-dependent).
From the respiratory system: often - cough, upper respiratory tract infections (pharyngitis, rhinitis, sinusitis, bronchitis), swelling of the nasal mucosa; infrequently - dyspnea.
From the digestive system: often - nausea, diarrhea, abdominal pain, dyspeptic disorders; uncommon - taste disturbance, anorexia, dry mouth, vomiting, flatulence, constipation, gastritis, liver dysfunction; rarely - hepatitis.
From the urinary system: uncommon - urinary tract infections, impaired renal function, urinary urgency, acute renal failure.
From the genital organs and mammary gland: infrequently - decreased libido, impotence.
From the skin and subcutaneous tissues: uncommon - dry skin, erythema, skin hyperemia, photosensitivity, increased sweating, alopecia.
From the musculoskeletal system: often - muscle cramps in the lower extremities, myalgia, pain in the back, chest, legs; uncommon - arthritis, arthralgia, fibromyalgia, rhabdomyolysis.
Allergic reactions: rarely - skin rash, urticaria, itching, angioedema (including swelling of the larynx and tongue), Quincke's edema, allergic vasculitis, Henoch-Schönlein purpura.
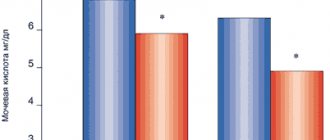
From laboratory and instrumental data: often - hyperkalemia; infrequently - moderate increase in the concentration of urea and creatinine in the blood serum, hypoglycemia, hyponatremia, hyperuricemia; very rarely - increased activity of liver enzymes, hyperbilirubinemia.
Other: often - asthenia, increased fatigue.
Drug interactions
Losartan can be used concomitantly with other antihypertensive drugs.
There were no clinically significant drug interactions between losartan and hydrochlorothiazide, digoxin, warfarin, cimetidine, phenobarbital, ketoconazole and erythromycin.
Rifampicin and fluconazole have been reported to reduce plasma concentrations of the active metabolite. The clinical significance of this interaction is not yet known.
As with the use of other drugs that block the formation of angiotensin II and its effects, the concomitant administration of potassium-sparing diuretics (spironolactone, triamterene, amiloride), potassium supplements and salts containing potassium may lead to an increase in the content of potassium ions in the blood serum.
Antihypertensive drugs may enhance the hypotensive effect of losartan.
Tricyclic antidepressants, antipsychotics, baclofen, amifostine, which reduce blood pressure as a main or side effect, can enhance the hypotensive effect of losartan and increase the risk of developing arterial hypotension.
With the simultaneous use of angiotensin II receptor antagonists and NSAIDs (including selective COX-2 inhibitors, acetylsalicylic acid as an anti-inflammatory agent), the hypotensive effect of losartan may be reduced. In patients with impaired renal function, the simultaneous use of angiotensin II antagonists or diuretics and NSAIDs may cause further deterioration of renal function, incl. acute renal failure and increased potassium levels in the blood serum. This combination should be used with caution, especially in elderly patients.
With simultaneous use of lithium with ACE inhibitors, a reversible increase in the concentration of lithium in the blood serum and the development of toxicity were recorded; in very rare cases this has been observed with the use of angiotensin II receptor antagonists. Caution should be used when lithium is used concomitantly with losartan. If this combination is necessary, it is recommended to monitor the concentration of lithium in the blood serum.
Mutually enhances the effect of beta-blockers and sympatholytics; combined use of losartan with diuretics causes an additive effect.
Dual blockade of the RAAS (eg, by combining an angiotensin II receptor antagonist with an ACE inhibitor or aliskiren) in patients with established atherosclerosis, heart failure, or diabetes mellitus with end-organ damage is associated with a higher incidence of hypotension, syncope, hyperkalemia, and renal dysfunction. (including the development of acute renal failure) compared with the use of a single-component blockade of the RAAS. The issue of using double blockade of the RAAS should be decided in each case individually and with careful monitoring of blood pressure, water-electrolyte balance of the blood and renal function.
Losartan-H Canon
Hydrochlorothiazide
Arterial hypotension and water-electrolyte imbalance
As with any other antihypertensive drug, symptomatic hypotension may develop in some patients. Patients should be monitored for clinical signs of fluid and electrolyte imbalance, such as hypovolemia, hyponatremia, hypochloremic alkalosis, hypomagicemia, or hypokalemia, which may develop with concomitant diarrhea or vomiting. In such patients, it is necessary to periodically (at appropriate intervals) monitor the content of electrolytes in the blood plasma. Patients with edema in hot weather may develop hypervolemic hypopatremia.
Endocrine and metabolic effects
Treatment with typhoids can lead to impaired glucose tolerance. Dosage adjustment of hypoglycemic agents, including insulin, may be required. During treatment with thiazides in patients with impaired glucose tolerance, the manifestation of diabetes mellitus is possible.
Thiazides may reduce renal excretion of calcium and cause small intermittent increases in plasma calcium concentrations. Severe hypercalcemia may be a sign of hidden hyperparathyroidism. Before testing the function of the parathyroid glands, treatment with thiazides should be discontinued. Treatment with thiazide diuretics may be accompanied by an increase in the concentration of cholesterol and triglycerides in the blood plasma.
In some patients, treatment with thiazides may provoke the occurrence of hyperuricemia and/or gout. Because losartan reduces uric acid concentrations, use of losartan in combination with hydrochlorothiazide may slow the development of diuretic-induced hyperuricemia.
Liver dysfunction
Thiazides should be prescribed with caution to patients with impaired liver function or progressive liver diseases due to the risk of developing intrahepatic cholestasis, as well as due to the fact that minor disturbances in water and electrolyte balance may be a prerequisite for the development of hepatic coma. Hydrochlorothiazide is contraindicated in patients with severe hepatic impairment (see section "Contraindications").
Non-melanoma skin cancer
Two pharmacoepidemiological studies using data from the Danish National Cancer Registry demonstrated an association between hydrochlorothiazide use and an increased risk of non-melanoma skin cancer (NMSC) basal cell carcinoma and squamous cell carcinoma. The risk of developing NMSC increased with increasing total (cumulative) dose of hydrochlorothiazide. A possible mechanism for the development of NMSC is the photosensitizing effect of hydrochlorothiazide.
Patients taking hydrochlorothiazide as monotherapy or in combination with other drugs should be aware of the risk of developing NMSC. It is recommended that such patients undergo regular skin examination to identify any new suspicious lesions as well as changes in existing skin lesions.
Any suspicious skin changes should be reported to your doctor immediately. Suspicious areas of skin should be examined by a specialist. To clarify the diagnosis, histological examination of skin biopsies may be required.
To minimize the risk of developing NMSC, patients should be advised to follow preventive measures, such as limiting exposure to sunlight and UV rays, and using appropriate protective equipment.
In patients with a history of non-melanoma skin cancer, it is recommended to reconsider the use of hydrochlorothiazide.
Other
Cases of transient myopia and acute attacks of angle-closure glaucoma have been reported with the use of hydrochlorothiazide. Risk factors for the development of an acute attack of angle-closure glaucoma may include anamnestic data on allergic reactions to sulfonamide and penicillin derivatives.
Symptoms
: Sudden onset, sudden decrease in visual acuity, or eye pain, usually occurring within a few hours to a week after starting therapy. An uncontrolled attack of angle-closure glaucoma can lead to permanent vision loss. The first step is to stop taking hydrochlorothiazide. If intraocular pressure does not decrease after discontinuation of hydrochlorothiazide, medical or surgical treatment may be required.
While taking thiazides, hypersensitivity reactions may develop in patients with a history of bronchial asthma, as well as in patients with a burdened allergic history. Cases of the occurrence or exacerbation of systemic lupus erythematosus during treatment with thiazides have been described.
Losartan
Angioedema
Patients with a history of angioedema (swelling of the face, lips, pharynx and/or tongue) should be closely monitored.
Arterial hypotension and decreased circulating blood volume
In patients with hypovolemia and/or reduced sodium levels in the blood plasma resulting from intensive use of diuretics, restriction of dietary salt intake, diarrhea or vomiting, symptomatic arterial hypotension may develop (especially after taking the first dose). It is necessary to correct such conditions before starting to take losartan.
Water-electrolyte imbalance
Water-electrolyte imbalances often occur in patients with impaired renal function, so the potassium content in the blood plasma and creatinine clearance should be carefully monitored, especially in patients with heart failure and creatinine clearance in the range of 30-50 ml/min. The simultaneous use of losartan with potassium-sparing diuretics, potassium supplements and potassium-containing salt substitutes is not recommended.
Liver dysfunction
Pharmacokinetic data indicate a marked increase in plasma concentrations of losartan in patients with liver cirrhosis. Based on these data, losartan should be used with caution in patients with a history of mild or moderate hepatic impairment. There is no experience with the use of losartan in patients with severe hepatic impairment, therefore the drug is contraindicated in patients with severe hepatic impairment.
Renal dysfunction
Impaired renal function has been reported due to inhibition of the RAAS, including renal failure (particularly in patients whose renal function is dependent on the RAAS, for example, with severe heart failure or existing renal impairment). As with the use of other drugs that affect the RAAS, cases of increased concentrations of urea and creatinine in the blood plasma have been described in patients with bilateral renal artery stenosis or with renal artery stenosis of a single kidney. These changes in renal function may be reversible and decrease after treatment is discontinued. Losartan should be used with caution in patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney.
Kidney transplant
There is no experience with the use of losartan in patients who have recently undergone kidney transplantation.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism typically do not respond to treatment with antihypertensive drugs that inhibit the RAAS. For this reason, the use of losartan is not recommended.
Coronary heart disease and cerebrovascular disease
As with any other antihypertensive drugs, an excessive decrease in blood pressure in patients with coronary heart disease or cerebrovascular disease can lead to the development of myocardial infarction or stroke.
Heart failure
As with other drugs that affect the RALS, patients with heart failure (with or without renal impairment) are at risk of developing severe hypotension as well as renal impairment (often acute).
Aortic and mitral valve stenosis, hypertrophic obstructive cardiomyopathy
As with other vasodilators, special caution should be exercised when treating patients with aortic or mitral stenosis or hypertrophic obstructive cardiomyopathy.
Differences due to ethnicity
By analogy with other ACEIs, losartan and other ARB II are noticeably less effective in lowering blood pressure in blacks compared to patients of other races. This may be due to more frequent cases of low renin levels in the black population with arterial hypertension.
Dual blockade of the renin-angiotensin-aldosterone system
There is evidence that the simultaneous use of ACE inhibitors, ARB II or aliskiren increases the risk of arterial hypotension, hyperkalemia and renal dysfunction (including acute renal failure).
The use of losartan concomitantly with aliskiren is contraindicated in patients with diabetes mellitus or patients with moderate to severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) (see section "Contraindications"). The use of losartan in combination with ACE inhibitors is contraindicated in patients with diabetic nephropathy (see section "Contraindications").