Medical Internet conferences
The lungs perform two main functions in the body: ensuring respiration and functioning of immune defense mechanisms. The correct performance of these functions is associated with pulmonary surfactant.
Surfactant in the lungs is synthesized by type II alveolar cells and secreted into the alveolar space. Surfactant covers the surface of the alveolar epithelium and consists of lipids (90%) and proteins (10%), making up the lipoprotein complex. Lipids are mainly represented by phospholipids. Deficiency and/or qualitative changes in the composition of pulmonary surfactant have been described in tuberculosis, neonatal respiratory distress syndrome, pneumonia and other diseases. [1-4].
Surfactant proteins are represented by proteins SP-A, (Surfactant Protein A, 5.3%), SP-D (0.6%), SP-B (0.7%), and SP-C (0.4%). [4-6].
The functions of the hydrophilic proteins SP-A and SP-D are associated with immune defense in the lungs. These proteins bind lipopolysaccharide of gram-negative bacteria and aggregate various microorganisms, affecting the activity of mast cells, dendritic cells, lymphocytes and alveolar macrophages. SP-A inhibits dendritic cell maturation, whereas SP-D increases the ability of alveolar macrophages to uptake and present antigens, stimulating adaptive immunity [7,8].
Surfactant protein A is the most abundant pulmonary surfactant protein. It has pronounced immunomodulatory properties. The SP-A protein affects the growth and viability of microorganisms by increasing the permeability of their cytoplasmic membrane. Moreover, SP-A stimulates macrophage chemotaxis, affects immune cell proliferation and cytokine production, increases the production of reactive oxidants, increases phagocytosis of apoptotic cells, and stimulates bacterial phagocytosis. Human SP-A consists of two gene products, SP-A1 and SP-A2, whose structure and function are different. The most important difference in the structure of SP-A1 and SP-A2 is amino acid position 85 of the collagen-like region of the SP-A protein, where SP-A1 has a cysteine and SP-A2 has an arginine. Functional differences between SP-A1 and SP-A2 include their ability to stimulate phagocytosis, inhibit surfactant secretion[7]. In all these cases, SP-A2 has greater activity than SP-A1. [8].
The functions of the hydrophobic proteins SP-B and SP-C are associated with ensuring the possibility of respiration. They reduce surface tension in the alveoli and promote uniform distribution of surfactant on the surface of the alveoli. [9].
Surfactant-BL (Surfaktant-BL)
Surfactant-BL is a highly purified natural surfactant from the lungs of cattle, is a complex of substances from a mixture of phospholipids and surfactant-associated proteins, has the ability to reduce surface tension on the surface of the pulmonary alveoli, preventing their collapse and the development of atelectasis.
Surfactant-BL restores the content of phospholipids on the surface of the alveolar epithelium, stimulates the involvement of additional areas of the pulmonary parenchyma in breathing and promotes the removal of toxic substances and infectious agents from the alveolar space along with sputum.
The drug increases the activity of alveolar macrophages and inhibits the expression and excretion of cytokines by polymorphonuclear leukocytes and eosinophils; it improves mucociliary clearance and stimulates the synthesis of endogenous surfactant by type II alveolocytes, and also protects the alveolar epithelium from damage by chemical and physical agents, and restores the functions of local innate and adaptive immunity.
The drug, when administered daily inhalation to experimental animals for 10 days, has no effect on the cardiovascular system, does not have a local irritating effect, does not affect blood composition and hematopoiesis, with the exception of short-term (1 day after stopping administration of the drug in doses of 200 and 400 mg/kg ) lymphopenia and granulocytosis due to an increase in the number of rod and segmented neutrophils. Subsequently, the composition of peripheral blood is completely normalized.
The drug does not affect the biochemical parameters of blood, urine and the blood coagulation system, does not cause pathological changes in the functions and structure of internal organs, and does not have teratogenic, allergenic and mutagenic properties.
After inhalation administration of the drug to rats 5 times a week for 6 months at total doses of 260 mg/kg, 520 mg/kg and 780 mg/kg and additional observation for another month without drug administration, no pathological changes were found in the morphology of the cardiovascular system. , central nervous and hematopoietic systems.
Multicenter randomized clinical trials were conducted in patients who received standard treatment with anti-tuberculosis drugs for 2-6 months before starting surfactant therapy and did not show positive dynamics.
Evaluation of the effectiveness of a two-month course of Surfactant-BL inhalations in the complex treatment of pulmonary tuberculosis showed the following: cessation of bacterial excretion after completion of the Surfactant-BL course was observed in 50% of patients and in 24.0% of patients in the control group. 16 weeks after the start of treatment, 80.0% of patients achieved abacillation compared to 62.0% of the control group; in 100% of patients in the main group and in 68.0% of patients in the control group, a decrease in infiltrative and focal changes was detected; In 70.0% of patients in the main group and in 36.0% of patients in the comparison group, closure of the cavity(s) was detected.
Thus, the effect of such combination therapy occurs much faster and in a significantly larger percentage of patients in comparison with accepted anti-tuberculosis therapy regimens.
Application of Kurosurf in neonatology
Currently, there is an intensive development of new medical technologies aimed at saving the lives of newborns. In recent decades, significant progress has been made in this direction, including due to the improvement of methods of care for very premature newborns [13]. If in the early 1980s. survival rate among children weighing less than 1500 g was 65–70%, then by the end of the 1990s. it increased to 85% [39]. According to Vaganov N.N., in Russia there is a steady increase in the number of children born with extremely low body weight. If in 1991 there were 144.1 per 10,000 live births, then after 5 years this figure increased to 197.6 per 10,000 live births [1]. Against the backdrop of a general increase in the number of premature infants and improved survival rates, there has been an increase in the significance of some pathological conditions characteristic of this group of patients. The above directly applies to lung diseases caused by surfactant deficiency.
Pulmonary surfactant is a surfactant that lines the alveolar space and prevents the development of alveolar collapse at the end of expiration.
The main stages of surfactant metabolism take place in the endoplasmic reticulum of second-order alveolocytes. Phospholipids and apoproteins are transported by the Golgi apparatus into lamellar bodies, where surfactant accumulation occurs. In the early fetal period (12–14 weeks of gestation), alveolar epithelial cells begin to synthesize phospholipids, and from the 20–24th week of gestation, lamellar bodies are detected in type II alveolocytes, but the secretion of phospholipids into the alveolar space occurs only after the 29–30th week gestation. Exocytosis of surfactant develops due to the fusion of membranes of lamellar bodies and alveolocytes of the second order and is regulated by catecholamines, corticosteroids, adenosine triphosphate (ATP), and cyclic adenosine monophosphate (cAMP) [46]. The greatest secretory activity of second-order alveolocytes is achieved only by the 35th week of gestation - during a normal pregnancy. Exocytosis of lamellar bodies into the alveolar space becomes more intense with the onset of labor and is maintained at this level throughout the entire period of postnatal adaptation. On the surface of the alveoli, surfactant is organized into tubular myelin, which is its extracellular reservoir and contributes to the formation of a monomolecular phospholipid layer. From the alveoli, surfactant components again enter second-order alveolocytes, where they are reutilized to a greater extent due to phagocytosis and destroyed in alveolar macrophages.
Surfactant consists of a complex of substances: lipids (80–90%), proteins (10%), apoproteins 5%, carbohydrates and ions. 80–90% of lipids are represented by phospholipids (phosphatidylcholine and lecithin 70%, phosphatidylglycerol 5–10%, phosphatidylinositol) [46]. Four surfactant-associated proteins (apoproteins) have been identified: SP-A, SP-B, SP-C, SP-D, synthesized by airway epithelial cells and Clara cells. Apoprotein SP-A plays an important role in the metabolism of surfactant, regulates its secretion, protects against bacterial endotoxins [42], herpes simplex viruses [43], and influenza [7], increases the phagocytic activity of macrophages and the production of free oxygen radicals [41]. Apoproteins SP-B and SP-C serve for adsorption and distribution of phospholipids in the alveolar space and the formation of tubular myelin. Apoprotein SP-D takes an active part in protecting the lungs from pathogenic microorganisms. These four surfactant proteins play an important role in increasing resistance to albumin and fibrinogen as they leak into the alveoli.
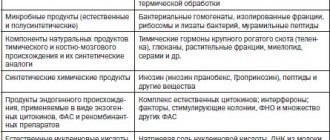
In 1980, Japanese scientists T. Fujiwara and co-authors published the first results of the successful clinical use of exogenous surfactant [11]. It was from this time that the active development of technologies for the production of both natural and artificial exogenous surfactants began (Table 1).
Clinical studies conducted between 1984 and 1993 objectively reflected the effectiveness of the use of various surfactant preparations depending on the time, mode and dose of administration, as well as the preventive and therapeutic effects of natural and synthetic surfactant preparations [32]. Close attention was paid to such nosological forms as RDS, meconium aspiration syndrome (MAS), and intrauterine pneumonia.
The scientific basis and experience of the clinical use of surfactant are most fully reflected in the book “Pulmonary Surfactant: from molecular biology to clinical practice” (Robertson B. et al., 1992) [30], which to this day is the main monograph on the role of surfactant and its application in clinical practice.
Kurosurf surfactant is prepared from ground pork lungs by washing, centrifugation, isolation in the presence of chloroform and methanol, and subsequent chromatography. It consists of 99% polar lipids (mainly phospholipids) and 1% hydrophobic, low molecular weight proteins (apoproteins B and C) [47].
The effectiveness of Kurosurf has been confirmed in a number of scientific studies. In 1987, GW Noack et al published the first clinical study on the use of Kurosurf in 10 children with severe RDS [24]. B. Robertson, T. Curstedt in 1988 demonstrated the positive effect of curosurf using the example of a model of RDS in premature laboratory animals [29]. After the administration of surfactant, there was a significant decrease in the oxygen concentration in the inhaled mixture and an increase in the alveolar-arterial oxygen gradient. Data from the European Multicentre Study Group demonstrate the effectiveness of even a single dose of Kurosurf in children, compared with data obtained in a control group where newborns did not receive surfactant. A decrease in neonatal mortality by the 28th day of life from 51 to 31%, a decrease in the incidence of interstitial pulmonary emphysema (IPE) and pneumothorax in the group of patients receiving surfactant therapy was proven [10].
Based on a meta-analysis of 11 controlled randomized clinical trials [27], it was found that the administration of natural surfactant (Curosurf) significantly reduced the incidence of pneumothorax (by 27%), severe forms of bronchopulmonary dysplasia (BPD) and mortality (by 13%), but increased incidence of intraventricular hemorrhage (IVH) [33]. However, based on a retrospective analysis of national studies conducted in the Netherlands, Sweden, France and Italy, it was proven that the risk of developing IVH in preterm infants is reduced with the prophylactic use of curosurf [45]. A series of scientific studies have demonstrated the more significant effectiveness of Kurosurf compared to other synthetic and natural surfactant preparations [6, 21, 26, 31, 36] in the treatment of various pathologies. Thus, the works of E. Herting (2000) [19] and P. Rauprich (2000) [28] show the effectiveness of Kurosurf for pneumonia caused by group B streptococcus, associated with the bactericidal activity of the drug against this pathogen. The first reports of the effective use of curosurf in MAS appeared [9, 23]. According to the researchers, in this case there was an improvement in oxygenation, a reduction in the duration of artificial pulmonary ventilation (ALV) and length of hospitalization [12, 16, 25].
Surfactant replacement therapy is an integral part of therapy in premature infants with respiratory distress syndrome (RDS).
RDS is a disease clinically manifested by tachypnea, cyanosis, retraction of the compliant areas of the sternum, and crepitating rales. These symptoms develop in the first hours of life; the patient's condition may become critical by about the 3rd day of life. As a result, the child suffers from severe hypoxia and acidosis. In the acute phase of the disease, the child develops atelectasis, caused by a primary deficiency of surfactant and the formation of hyaline membranes lining the surface of the alveoli. Insufficient negative pressure during inspiration during spontaneous breathing does not allow the collapsed alveoli to straighten, a progressive loss of gas exchange surface occurs, and, consequently, an increase in the work of breathing. This leads to an increase in the need for oxygen concentration in the inhaled air, an increase in respiratory and metabolic acidosis. Moreover, a functioning ductus arteriosus worsens the situation due to a significant increase in pulmonary blood flow, enrichment of the pulmonary circulation, increase in pulmonary edema and inactivation of its own surfactant. As a result, severe respiratory failure develops, requiring tracheal intubation and mechanical ventilation. The use of natural surfactant leads to clinical improvement in the condition of the newborn. It is more preferable to use Kurosurf for prophylactic purposes, however, repeated administration of the drug is effective.
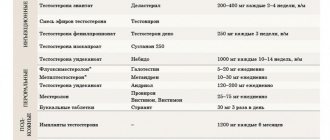
Tables 2 reflect the results of the main clinical studies on the use of Kurosurf, which were conducted in various years.
From the above data it follows that early administration of surfactant (within the first 2 hours of life) can reduce the duration of mechanical ventilation and oxygen therapy, reduce the incidence of air leak syndrome, BPD and mortality, and repeated administration of surfactant makes it possible to increase survival during the first 28 days life.
Administration of the drug during the first 30 minutes of life is considered prophylactic. The main indication for prescribing a prophylactic dose of surfactant is a high risk of developing RDS.
According to J. Tooley, published in 2003, in the UK, up to 98% of newborns with a gestational age of less than 28 weeks require mechanical ventilation after birth and 97% remain on mechanical ventilation during the first day of life [38]. Taking into account the above, it can be assumed that prophylactic administration of surfactant to premature newborns with extremely low body weight (ELBW) will be justified and cost-effective by reducing the duration of mechanical ventilation and the total time of hospitalization. Preventive and early administration of surfactant leads to a significant increase in survival rate among children with ELBW, and also reduces the number of cases of chronic bronchopulmonary pathology and the incidence of air leak syndrome [14, 34, 48].
Considering the fact that Kurosurf quickly and effectively restores lung mechanics, the main important point in the treatment of children on mechanical ventilation is a clear correction of ventilation parameters. It is the untimely reduction of mechanical ventilation parameters after surfactant replacement therapy that can lead to the development of severe complications - pneumothorax, interstitial pulmonary emphysema, and the development of severe intraventricular hemorrhages. An important factor during mechanical ventilation remains the constant expansion pressure during exhalation, which stabilizes the alveoli and increases the duration of action of the administered curosurf, preventing its destruction. The drug can be administered in two ways: by disconnecting the patient from the machine circuit and with ongoing mechanical ventilation.
For several years now, in clinical practice, the “INSURE” strategy (from the English intubation-surfactant-extubation - intubation-surfactant-extubation) has been used in the treatment of RDS in newborns. The essence of this method is that premature newborns are intubated immediately after birth, surfactant is injected into the trachea through an endotracheal tube, after which several forced breaths are taken with a self-expanding Ambu bag. As the children’s condition stabilizes (usually after 15–30 minutes, up to 2 hours), they are extubated and transferred to spontaneous breathing using positive pressure in the respiratory tract - CPAP (continuous positive airway pressure). A variety of systems can be used to administer CPAP—nasal cannulas, endotracheal tube, face mask, or nasal mask. In cases where nasal CPAP is not enough to maintain adequate gas exchange in the newborn, non-invasive methods of ventilation are used using the Infant Flow Advance device through nasal cannulas (VIASYS Healthcare Inc.). This strategy prevents prolonged mechanical ventilation and its complications in approximately 60% of preterm infants with RDS. Early replacement therapy with surfactant followed by transfer of children to nasal CPAP, compared with selective administration and mechanical ventilation of the lungs, more effectively reduces the need for prolonged mechanical ventilation and improves the absorption of exogenous surfactant. However, to date, there has been insufficient evidence of the impact of such a strategy on the incidence of BPD and chronic lung diseases (CLD) in preterm infants [37]. A study published in the journal Pediatrics in 2000 reported a clear effect of continuous expansion pressure compared with traditional mechanical ventilation on treatment outcome [22].
A Scandinavian study also demonstrated that nasal CPAP without surfactant was an effective form of respiratory therapy in only 30% of preterm infants with ELBW [20]. Other Scandinavian studies have shown that a single dose of curosurf before starting nasal CPAP can reduce the need for mechanical ventilation in preterm infants with LBW from 85 to 40%, and also improves the prognosis in these patients [40, 44]. As a result, this method of treating RDS in premature infants is the most cost-effective and most effective.
Also, one of the effective methods of respiratory therapy in neonatal practice is high-frequency oscillatory (HFO) mechanical ventilation. In essence, this method is close to CPAP, but ventilation is carried out through oscillations produced at a high frequency of 600 to 900 per minute. According to our clinic, complex treatment of RDS in premature newborns using high-chopper ventilation and replacement therapy with curosurf significantly improves survival and several times reduces the incidence of bronchopulmonary dysplasia in patients with severe respiratory failure [3].
In Russia, surfactant preparations appeared in the mid-1990s. Domestic scientists began to actively analyze the effectiveness of these drugs: V. A. Mikhelson [4], I. I. Ryumina [5], V. A. Grebennikov [2]. Currently, large Russian neonatal centers and maternity hospitals have the opportunity to use high-quality natural surfactant curosurf(r) (Chiesi Farmaceutici Parma, Italy).
The experience of using surfactants in clinical practice in St. Petersburg begins in 1993. Natural surfactant preparations began to be used in 1998. By the end of 2004, experience had been accumulated in the use of six different types of synthetic and natural surfactants (Exosurf, Curosurf, KL4, Survanta, HL, BL). It should be noted that our experience in using domestic exogenous surfactant (BL) does not make it possible to recommend it as a drug of choice for a number of reasons: low effectiveness in severe forms of RDS, unpredictability of action, high incidence of side effects.
In St. Petersburg, since 1999, there has been a city program for the centralized supply of surfactant to maternity hospitals and neonatal intensive care units. The use of Kurosurf in combination with new methods of respiratory therapy (trigger mechanical ventilation, high-frequency ventilation) led to a decrease in neonatal mortality, including in children with ELBW.
The above indicators demonstrate a clear trend in reducing mortality against the backdrop of the launch of a program for the centralized supply of Kurosurf to all maternity institutions in the city.
However, it must be emphasized that, despite a decrease in mortality, it is currently not possible to radically reduce the incidence of CLD. Antenatal therapy with steroids and surfactant in the early postnatal period has reduced the incidence of severe forms of RDS, but in 30–60% of children with ELBW, RDS is complicated by CLD. Therefore, RDS occupies a significant place in the structure of neonatal and infant mortality, and also leads to high disability in infants. Children with BPD more often suffer from respiratory tract infections and require repeated emergency hospitalizations, which leads to large financial costs for the purchase of medications, treatment and rehabilitation measures. Thus, effective prevention and treatment of RDS today remains a significant socio-economic problem.
For questions regarding literature, please contact the editor.
V. A. Lyubimenko , Candidate of Medical Sciences L. G. Pankratov A. V. Mostovoy , Candidate of Medical Sciences Children's City Hospital No. 1, St. Petersburg