Indications for use of the drug Inosine
Inosine - ischemic heart disease (in complex treatment), post-infarction period, heart rhythm disturbances caused by the use of cardiac glycosides, myocardial dystrophy. The use of inosine is also indicated for urocoproporphyria, hepatitis, and cirrhosis of the liver. Improves the function of the organ of vision in open-angle glaucoma with intraocular pressure normalized as a result of treatment. Inosine pranobex - viral infections in patients with normal immune status and in immunodeficiency states, including diseases caused by Herpes simplex types 1 and 2, measles, mumps, Epstein-Barr viruses and cytomegaloviruses, Varicella zoster ; viral bronchitis, viral hepatitis; diseases caused by the human papillomavirus; subacute sclerosing panencephalitis; chronic infectious diseases of the urinary and respiratory systems; stressful situations; postoperative period and convalescence period after serious illnesses; elderly age; radiation therapy.
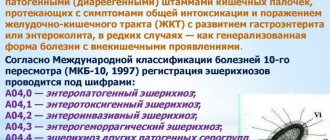
Introduction
The issues of antiviral therapy for respiratory infections in children are currently extremely relevant.
The pandemic of the new coronavirus infection caused by the SARS-Cov-2 virus has once again demonstrated that the use of drugs with antiviral effects in the first 48 hours from the onset of clinical manifestations of the infection reduces the severity of the disease and improves the outcome of the disease. The prescription of antiviral therapy for respiratory infections in children is determined by the patient’s age, the severity of the condition and the etiology of the disease. In addition to a large group of respiratory viruses, the cause of acute respiratory infections, including recurrent ones, can be viruses of the herpes group.
The role of active forms of herpesvirus infections (HVI) in the recurrence of respiratory tract infections in children and the formation of chronic foci of infection in the adenotonsillar zone has been shown. According to A.S. Levina et al., recurrent respiratory diseases in children from 1 year to 6 years are associated with GVI in 75% of cases [1]. The most frequently detected active forms of infection are those caused by human herpes virus (HHV) 6A/B, and somewhat less frequently by Epstein-Barr virus (EBV) and cytomegalovirus (CMV) [2]. Previous studies have shown that in a group of patients with monthly respiratory diseases, markers of HVI are detected in 91% of cases. Moreover, according to our research, in the group of children with monthly respiratory infections, the proportion of active forms is about 40%, which once again emphasizes the need for an integrated approach to diagnosing the etiology of recurrent diseases of the respiratory tract [3].
In recent years, the problem of combined GVI has become relevant. The presence of several herpesviruses in active form at once in the acute phase of the disease changes the clinical picture and complicates laboratory diagnosis of the condition.
In the work of N.G. Yaroslavtseva [4] demonstrated that the concentration of HHV-6 DNA in peripheral blood leukocytes and plasma of adult patients is almost 3 times lower in mixed HVI than in HHV-6 monoinfection (5.9 × 104 and 2 × 104, respectively). Earlier studies demonstrated the ability of HHV-6 to activate EBV replication from a latent state during co-infection [5, 6]. In turn, the presence of the EBV genome made B cells more susceptible to HHV-6 infection [7]. The combination of HHV-6 and EBV infection made it difficult to diagnose active forms of HVI in pregnant women [8] and in children after liver and kidney transplantation [9].
One of the most studied antiviral agents worldwide is inosine pranobex [10, 11]. The drug can affect the levels of viral RNA and is active against herpes simplex virus (HSV), human papillomavirus, human immunodeficiency virus, influenza viruses and acute respiratory infections, CMV infection and EBV [12].
Inosine pranobex (a synthetic compound of para-aminobenzoate NN-dimethylamino-2-propanol with inosine in a 3:1 molar ratio) has been widely used since 1971 as an antiviral agent, affects the immune system, enhancing the proliferation of T-lymphocytes and the activity of natural killer cells, increasing cytokine levels [12–15].
Currently, the antiviral effects of inosine pranobex are explained by three mechanisms:
Inosine pranobex binds to specific receptors on the cell membrane of lymphocytes or penetrates the cell and has a direct effect on the transmission of signals that increase nuclear-cytoplasmic transport and RNA synthesis in lymphocytes. This leads to the stimulation, maturation and functioning of virus-infected lymphocytes [16].
Inosine pranobex inhibits viral RNA synthesis. This mechanism causes the predominance of mRNA over RNA in the cells of the host organism, which reduces the ability of the virus to control protein synthesis [17].
Inosine pranobex enhances the effect of endogenous γ-IFN, which is one of the components of the stimulating effect of the drug on the cellular immune response. The drug is able to increase the levels of IL-2 and γ-IFN, reduce the level of IL-10, stimulate the maturation and differentiation of T lymphocytes, and also enhance activated lymphoproliferative reactions [15].
In 2022, M. Votava and J. Beran proposed the use of inosine pranobex as a nonspecific immunostimulant in the treatment of infection caused by the SARS-CoV-2 virus [18]. However, descriptions of studies examining the antiviral activity of inosine pranobex against SARS-Cov-2 in vitro
or clinical studies have not yet been found in the available literature.
In 2016, J. Beran et al. published the results of a randomized, placebo-controlled, double-blind, phase IV study demonstrating the efficacy and safety of inosine pranobex in acute respiratory viral infection (ARVI). The study included 463 adult patients with confirmed ARVI, of which 231 received inosine pranobex, 232 received placebo. In the study group, the patients' condition improved faster than in the placebo group; among patients under 50 years of age without obesity, the time for relief of influenza-like symptoms was significantly reduced. Inosine pranobex was found to be well tolerated [19].
Thus, in any epidemic season, there is a problem of choosing antiviral therapy tactics for children with respiratory infections, including recurrent ones. Active forms of HVI, including combined ones, play a role in the etiology of these conditions; therefore, it is necessary to use drugs with a proven wide spectrum of antiviral action.
Purpose of the study
: evaluation of the effectiveness of various treatment regimens using inosine pranobex (Normomed®) in children with monthly infections of the respiratory tract against the background of reactivation of HVI, including combined forms.
Use of the drug Inosine
Inosine - orally before meals or intravenously slowly, in a stream or drip. Initially, 200 mg (10 ml of 2% solution) is administered once a day, then, if well tolerated, up to 400 mg (20 ml of 2% solution) 1–2 times a day. The rate of administration is 40–60 drops per minute. The course of treatment is 10–15 days. In case of acute cardiac arrhythmia, jet injection in a single dose of 200–400 mg (10–20 ml of 2% solution). When administered intravenously, 2% inosine solution is diluted in 5% glucose solution or isotonic sodium chloride solution (up to 250 ml). The daily dose when taken orally is 0.6–2.4 g. In the first days of treatment, the daily dose is 0.6–0.8 g (0.2 g 3–4 times a day). If well tolerated, this dose is increased over 2–3 days from 1.2 g (0.4 g 3 times a day) to 2.4 g. The duration of the course is from 4 weeks to 1.5–3 months. For urocoproporphyria, the daily dose is 0.8 g (0.2 g 4 times a day). Take daily for 1–3 months. Inosine pranobex - adults are usually prescribed at a dose of 50 mg per 1 kg of body weight in 3-4 doses; children - 50–100 mg/kg in 3–4 doses. The average duration of treatment is 5–8 days, in severe cases up to 15 days. For herpes zoster ( Herpes zoster ), 1 g is prescribed 3-4 times a day for 10 days. For genital herpes - 1 g 3 times a day for 5-6 days (acute phase) in combination with local treatment, then 1 tablet 2 times a day for up to 6 months, depending on the severity of the disease and the frequency of relapses. For genital warts, 1 g is prescribed 3 times a day in combination with local treatment for 14–28 days. When combined with cryotherapy or CO2 laser therapy - 1 g 3 times a day for 5 days; carry out 3 courses of treatment with an interval of 1 month. For aphthous stomatitis, 1 g is prescribed 4 times a day for 6 days (acute phase), then 1 g 3 times a day, 2 times a week for 6 weeks. For chronic, recurrent urinary and respiratory tract infections in elderly patients, 1 g is prescribed 4 times a day for 2–3 months. For chronic, recurrent infectious diseases in children with a weakened immune system - 50-100 mg per 1 kg of body weight per day in 3-4 doses for 1-2 weeks (from 1 year - 0.5 g per 10 kg of body weight ). For viral hepatitis, 1 g is prescribed 3-4 times a day for 2-3 weeks, maintenance therapy is 0.5 g 2 times a day for up to 6 months.
Newspaper “News of Medicine and Pharmacy” 19(342) 2010
Relevance of the problem
In recent years, there has been an increased interest among practitioners in immunomodulatory agents, which has given impetus to the active publication of the results of the use of synthetic inosine analogues (SAIs) for various infectious diseases [1–3], lesions of the skin and mucous membranes associated with the human papillomavirus (HPV) [4–7] (Linask and Grigorieva, 2005), and conditions caused by immunodeficiency in children [8], in scientific, medical and popular science publications.
This is due to the fact that AIS, widely known in Western Europe, were registered in the CIS countries only at the very end of the last century. Currently, the Russian pharmaceutical market is saturated with a variety of immunomodulators, their number increasing every year [9]. At the same time, aggressive marketing technology is used in the media, which makes it difficult for practitioners to choose the optimal drug agent for the treatment and prevention of viral and opportunistic infections, especially in patients with impaired immune systems. The main aspects of the use of Groprinosin, one of the SAIs, were widely covered earlier by L.M. Belyaeva [8] in the complex treatment of frequently ill children, and by us - for herpetic and papillomavirus infections [10, 11], which predetermined the topic of this review:
1. Current trends in the spread and course of infectious diseases.
2. What are the requirements for an “ideal” immunomodulator and what determines the interest of scientists and clinicians in immunomodulators like inosine pranobex (Groprinosine).
3. The nature of direct analogues of inosine (PAI) and SAI.
4. Molecular mechanisms of potentiation of the immune system using SAI.
5. Results regarding the use of SAI for infections caused by the human immunodeficiency virus (HIV) and other viral, inflammatory and autoimmune diseases in difficult or problematic patients.
Current trends in the spread of infectious diseases
Global climate change, environmental pollution, the introduction of modified foods and the daily stress inherent in our era have radically changed the way people live and the adaptive capabilities of the human body. Increased international connections, mass tourism and globalization contribute to the active transfer and widespread spread of pathogenic microorganisms from one geographical region to another, exposing residents of new areas to mortal risk [12, 13].
According to WHO, half of the world's population is at risk of contracting various infectious diseases, which is accompanied by the death of about 17 million people annually [14]. A clear example of the emergence of infectious agents new to humans or modified strains of infectious disease agents that threaten new pandemics are HIV infection and the outbreak of bird and swine flu in recent years.
Antibiotics have significantly reduced morbidity and mortality from infectious diseases and thereby saved the lives and health of millions of people. A number of factors, such as a steady increase in the consumption of antibacterial drugs, indiscriminate and uncontrolled use of antibiotics, have led to the formation of antibiotic-resistant strains of infectious agents. Thus, according to the Centers for Disease Control, the annual budget of clinics increases by 661 million US dollars due to antibacterial resistance, not counting sick leave fees and other indirect financial losses [15]. Currently, the choice of antibacterial and antiviral drugs for the treatment of common infectious diseases is becoming limited and sometimes impossible.
As a result of the aggressive influence of all of the above factors, mutations in the human genome are increasingly occurring, disturbances in homeostasis and the immune system occur, which leads to a decrease in the body’s resistance and an increased risk of developing diseases caused by opportunistic pathogens and severe clinical manifestations of viral infections and fungal infections. Violation of the body's immune defense is accompanied by the clinical manifestation of opportunistic infections caused by bacteria, herpes simplex viruses (HSV), herpes zoster, human papilloma (HPV), cytomegalovirus (CMV), candida fungi, cryptococci, toxoplasma and other protozoal parasites. Modern clinical pathology is characterized, on the one hand, by the growth of chronic infectious diseases caused by opportunistic microbes, and on the other hand, by a decrease in the immunological reactivity of the population, observed in almost all developed countries [16].
Motives for searching for immunomodulators
Treatment of opportunistic infection is an extremely difficult task, due to the lack of adequate immune protection in such patients. Moreover, there are still no therapeutic agents aimed at the complete eradication of pathogens such as HSV, HPV, CMV, or obligate microorganisms existing in the human body in the form of symbiosis, which often manifest themselves as opportunistic infections [12]. It should be noted that in most cases, the body of an immunocompetent host independently eliminates HPV or transfers it to the latent stage of HSV or CMV infection [10, 11, 17]. The possibilities of targeted interaction between hierarchically organized components of the immune system, which in healthy individuals controls the situation during the introduction of microorganisms, depends on the nature of the infectious agent and the competence of the immune system [12].
Based on the outstanding results of vaccine prevention of infectious diseases, it was hypothesized that if the body’s natural immune defense is considered as the most highly organized anti-infective therapeutic system, then from this point of view it is a promising target for therapeutic manipulations. This state of affairs predetermined the need for the emergence of immunomodulatory agents aimed at stimulation, i.e. potentiation or, conversely, inhibition of one or another part of the immune system. So, according to R.M. Khaitov and B.V. Pinegin [16], “the main target of immunomodulatory drugs is secondary immunodeficiencies, which manifest themselves in the form of often recurrent, difficult-to-treat infectious and inflammatory diseases of various localizations. Any chronic infectious-inflammatory process is based on certain changes in the immune system, which are one of the reasons for the existence of this process.”
The first attempt to use a systemic immunomodulatory agent was a series of clinical experiments by Dr. William Coley, performed in the 80s of the 19th century to study the antitumor properties of bacteria. At first, Koley successfully introduced a suspension of live streptococci directly into tumor masses. Subsequently, he expanded his experiments and used gram-positive and gram-negative bacteria after their heat treatment, called “Cauley toxins” [18].
Currently, there are numerous immunomodulatory drugs of both natural and artificial origin (Table 1).
There is an intensive search for immunomodulatory agents; the use of new high-tech technologies in this area expands the possibilities for the development of new powerful, in particular recombinant, endogenous cytokines that have optimal therapeutic and prophylactic potential with minimal side effects [12, 19, 20].
Principles of immunotherapy and characteristics of an “ideal” immunomodulator
According to Academician A.A. Vorobyov [21], the prescription of treatment, the effect aimed at the immune system, should be based on the general principles of immunotherapy and the main requirements for immunomodulatory drugs are the presence of immunomodulatory properties in this drug, clinically proven high antiviral effectiveness, preferable natural origin, safety, harmlessness, absence addiction, absence of side and carcinogenic effects. Immunomodulators should not cause excessive sensitization and induction of immunopathological reactions, and should not potentiate it in other medications. Necessary qualities for the candidate's acceptability also include predictability of the metabolic pattern and route of elimination from the body, and high compatibility with other drugs used for infectious and inflammatory diseases. The preferred quality is the ease of delivery of the drug to the target area and the possibility of its use by non-parenteral routes [21].
Immunomodulators stimulate the host's defense mechanisms against pathogens of infectious diseases. Ideally, the optimal immunomodulators are substances that take part in the regulation of immune processes in the body (cytokines), or their synthetic or recombinant analogues. However, the use of cytokines is limited due to the inherent toxicity of cytokines, the unpredictability of their pharmacological behavior and the presence of a pleiotropic effect (multiple effect) in them. It should be noted that the effectiveness of exogenous cytokines is limited in individuals with reduced immunity due to the lack of appropriate effector cells or the presence of pathognomonic disease factors that prevent the activation of lymphocytes. The short half-life of exogenous cytokines and the need to use such cytokines in high doses to achieve a therapeutic effect stimulate researchers to search for the most acceptable and adequate immunopotentiator that takes part in the regulation of immune processes in the body, but does not have the side effects of cytokines. Such immunomodulators include SAIs, the precursors of which are natural purines. In anatomical-therapeutic-chemical, i.e. International system (ATS) of classification of drugs associated with WHO, both inosine and inosine pranobex are registered with codes as drugs for the treatment of diseases of the skin (D), urogenital organs (G), sensory organs (S), as immunomodulators (L) and antimicrobial antiviral drugs (J) for systemic use [22].
Inosine, a purine derivative, is a natural immunomodulatory and metabolic agent
It is known that purines have powerful immunomodulatory properties and are one of the fundamental substances necessary for the normal functioning of cells. Purines are constantly present in the body, they are supplied daily with food and take part in many physiological vital processes in the cell nucleus.
The best known representative of this class of substances is the nucleoside adenosine, which affects all aspects of the immune system [23, 24]. Thus, adenosine and its analogs prevent the development of various inflammatory diseases, rheumatoid arthritis, inflammation of the pleura, nephritis, colitis, uveitis and toxic shock. The effects of adenosine are believed to be due in part to the inhibition of harmful processes initiated by the immune system, including the release of proinflammatory cytokines and oxygen radicals. There is an active search for therapeutic agents based on the action of adenosine receptors for the treatment and prevention of infectious, autoimmune, ischemic and degenerative diseases.
Inosine is a metabolite of adenosine, formed due to the cleavage of the latter under the influence of diaminase (Fig. 1).
Inosine has properties similar to its predecessor, including anti-inflammatory effects in endotoxic and septic shock, colitis and severe forms of pneumonia, which have been demonstrated in various experimental models. It inhibits the secretion of proinflammatory cytokines, including tumor necrosis factor (TNF-α) and interleukin (IL-1β), produced by activated monocytes and epithelial cells. Inosine also inhibits the production of superoxide radicals by stimulated neutrophils. The bioavailability of inosine is high (more than 90%), and complete elimination of inosine and its metabolite uric acid from the body occurs within 48 hours, therefore, there is no accumulation of inosine in the body.
Direct analogues of inosine (DIA) under the trade name Riboxin or Inosine F are used as anabolic agents due to their metabolic, antihypoxic and antiarrhythmic properties. Riboxin [9-Ribofuranosylpurine-6 (1H)-OH] contains hypoxanthine as a purine base; accordingly, in the liver the drug is broken down into ribose and hypoxanthine. Further, hypoxanthine, as a precursor of ATP, stimulates the synthesis of nucleotides, activates the metabolism of pyruvic acid to ensure the normal process of tissue respiration, and enhances the activity of some enzymes of the Krebs cycle. PAIs, penetrating into cells, increase energy levels, have a positive effect on metabolic processes in the myocardium, increasing its energy balance, improve coronary circulation and, thus, increase the strength of heart contractions. PAIs are directly involved in glucose metabolism and contribute to the activation of metabolism under hypoxic conditions and in the absence of ATP. Accordingly, PAI is widely used for diseases of the cardiovascular system, coronary heart disease, liver cirrhosis, severe post-infectious conditions, poisoning, radiation exposure and other serious diseases.
Inosine pranobex is a synthetic analogue of inosine (SAI)
Inosine pranobex consists of two components: the first (active) component is inosine, a metabolite of purine (1,9-dihydro-9-β-D-ribofuranosylo-6H-purine-6-OH); the second (auxiliary) component increases the availability of inosine for lymphocytes (salt of 4-acetamidobenzoic acid with N,N-dimethylamino-2-propanol) in a molar ratio of 1: 3, which is patented in the USA under the name Methisoprinol.
Currently, there are more than 10 trade names of SAI in the pharmaceutical markets (Groprinosin, Inosiplex, Inosine pranobex, Immunovir, Methisoprinol, Isoprinosine, Viruxan, Prinosine, Virimun, Modimunal, etc.) from various pharmaceutical companies in 3 dosage forms (tablets, syrup , solution), which have proven themselves as a powerful immunomodulator and antiviral drug. By 1990, SAIs were registered in more than 70 countries, and by 1996, according to Newport Pharmaceuticals, the results of more than 1,750 clinical studies had been published. Since the use of the drug in clinical practice, the tablet equivalent of SAI consumption was 109, and therefore, when recalculated for the course dose of “6 tablets × × 10 days”, the consumption index was equal to 18 × 106. SAIs are safe products of the purine series, non-toxic even when prescribed high doses [25, 26].
There is evidence that SAIs suppress the replication of DNA and RNA viruses by binding to the cell ribosome and changing its stereochemical structure and contribute to the restoration of cellular immunity in the treatment of malignant tumors, especially in patients receiving chemotherapy or radiation.
Groprinosin is considered a universal immunomodulator with a predominance of thymomimetic effects (Fig. 2).
Groprinosin activates the proliferation of T-lymphocytes, T-helpers, natural killer cells (NK) and balances the balance of the cellular and humoral components in the immune system:
- on the one hand, by stimulating biochemical processes in macrophages, it enhances the chemotactic and phagocytic activity of monocytes, macrophages and polymorphonuclear cells;
- on the other hand, while simultaneously increasing the production of cytokines (interferons and interleukins), it enhances the synthesis of antibodies.
Results of clinical trials of SAI for various diseases and HIV infection
Over more than 38 years of use of SAIs, there have been no reported cases of serious side effects from their clinical use. It is noteworthy that there is evidence from numerous clinical trials on the effectiveness of SAI as an immunomodulatory and antiviral agent in problematic or difficult patients.
SAIs have been used in many countries to treat various infectious and autoimmune diseases, especially in difficult patients, including hepatitis [27, 28], arthritis [29], HIV infection [30–36], influenza and ARVI [2, 3, 26], with chronic fatigue syndrome [37] and diseases of the skin, hair and mucous membrane, such as focal and total alopecia (hair loss) [38–41] and HPV-positive proliferative warty leukoplakia of the oral mucosa [42].
From a practical point of view, the use of SAI in HIV-infected individuals is of interest. Thus, at the initial stage of the HIV pandemic, SAIs were widely used in combination with various antiviral drugs. SAIs, as immunomodulatory agents, were thought to delay the progression of HIV infection and thus prevent the development of AIDS [30, 43, 44]. The evidence for this hypothesis was the results of numerous clinical trials of SAI [31–35]. A Scandinavian research group conducted a randomized, double-blind, placebo-controlled study to evaluate the effectiveness and safety of SAI in the treatment of patients with HIV without clinical manifestations of AIDS. This multicenter study analyzed the results of 866 patients from 21 medical centers in Denmark and Sweden [31, 35]. Depending on the level of CD4+ cell concentration, patients were divided into 3 groups, which were double randomized to receive SAI 1 g 3 times a day (n = 429) or placebo (n = 437) for 24 weeks. The drug was well tolerated, and a long period of use of SAI did not cause any side effects. At the end of treatment, the development of signs of AIDS progression was noted in 17 cases among individuals who received placebo, and only in 2 cases among infected individuals who received SAI. The effectiveness of SAI in this indicator was significantly superior to the same result in the placebo control (p < 0.001) with a probability coefficient of a successful outcome of 8.6 (95% CI 2.2–52.6). Based on these data, BK Pedersen et al. believe that SAIs significantly delay the progression of AIDS in HIV-infected individuals. J. Rhodes [45], having analyzed data on the use of immunomodulators, believes that the antiviral effect of inosine pranobex is associated with its ability to enhance the production of IFN-α. He believes that the ability of SAI to delay the progression of AIDS, identified during clinical use, is associated with the interference of SAI with the synthesis of folates (folic acid salts), inherent in the replication of the causative agent of Pneumocystis pneumonia (P. carinii) [45, 46].
In the mid-90s of the last century, due to the development and introduction of new highly effective drugs against HIV, interest in the use of immunomodulatory drugs waned, however, in 1999, Newport Pharmaceuticals International and the National Institute of Allergy and Infectious Diseases sponsored 7 scientific projects for clinical trials of SAI. The main areas of the trial were severe forms of AIDS; AIDS-related symptom complex; diseases of the lymph nodes and immunosuppressed patients in the absence of generalized lymphadenopathy. This set of trials also included determining the optimal dose of inosine pranobex in immunosuppressed volunteers, assessing its effectiveness and safety in patients with weakened immune systems and lymph node disease, as well as a phase I and II clinical trial of the combined use of ribovirin and SAI in asymptomatic HIV-infected patients . Clinical trials on the use of SAI in HIV-infected patients are ongoing, which indicates the significance of SAI in HIV infection, and the combined use of antiviral and immunomodulatory agents is considered a rational approach [19, 20, 36].
There are also clinical and experimental results assessing the effectiveness of SAI in acute respiratory viral infections [2, 3], influenza [47] and allergic diseases [1]. Thus, in patients with chronic obstructive pulmonary disease, Groprinosin was used to treat ARVI during the development of clinical symptoms (in 14 people, 1 g 3 times a day for 5–7 days). According to the author, the inclusion of Groprinosin in the complex treatment of ARVI significantly reduces the duration of the clinical manifestation of ARVI with minimal symptoms of intoxication and prevents the complicated course of ARVI. The use of Groprinosin for the prevention of ARVI in 12 patients (50 mg/kg daily or 3 times a week for two months) contributed to a significant reduction in the incidence of ARVI in frequently ill individuals. If these patients became ill, their acute respiratory viral infections did not last long, with minimal and mild symptoms [3]. Similar positive clinical data were obtained in another study, when Groprinosin was used in 27 patients for the treatment of sore throat due to ARVI [2].
MM. Abelevich et al. [1], using SAI in 31 children with complicated allergic diseases of the skin and respiratory tract, showed a decrease in infectious complications and recurrence of the underlying disease compared to similar indicators in the control group of 29 patients.
FROM. Karimov [27] demonstrated the effectiveness of SAI in acute viral hepatitis B, prescribing SAI to 14 patients daily at 50 mg/kg for 5–10 days against the background of traditional therapy and to 21 patients - traditional treatment. There was a reduction in time in terms of both regression of clinical symptoms and normalization of biochemical parameters, indicating an improvement in liver function, which led to a decrease in the time patients spent in the clinic.
In 33 patients, J. Janeczko [48] established a diagnosis of mononucleosis based on clinical symptoms and the degree of impairment of blood tests using nonspecific and/or specific serological tests. At the same time, the total number of lymphocytes varied from 884 to 992 per 1 mm3. The number of B lymphocytes varied from 146 to 198, CD4 - from 482 to 645 and CD8 - from 245 to 364 per 1 mm3. 18 patients were prescribed thymosin 0.02 g daily subcutaneously for 30 days, and 15 patients were prescribed SAI 3 g in a similar regimen. For control purposes, 12 patients with less severe lymphopenia were additionally observed and did not receive treatment. The effectiveness of treatment was assessed by determining the total number of lymphocytes, B-lymphocytes, CD4 and CD8 cells before and after the course of the above treatment, followed by control studies every 6 months for 5 years of observation. In 33 patients who received immunotherapy, the overall effectiveness of mononucleosis therapy was 64%, which was higher than that (40%) in 12 patients with spontaneous normalization of blood counts.
The results of the successful use of SAI for total and focal alopecia, in our opinion, are of particular interest, given the complexity of the etiopathogenesis of this pathology and the low effectiveness of existing methods of its treatment. Thus, S. Georgala et al. [40] conducted a randomized, double-blind, placebo-controlled study in 34 patients with alopecia areata who had previously failed systemic and local treatments. Inclusion criteria were disease duration of more than 1 year and the absence of previous immunotherapy. 16 patients were prescribed 50 mg/kg SAI (Inosine pronabex) daily in 5 divided doses for 12 weeks, the remaining 16 patients were prescribed placebo in a similar regimen. The effectiveness of therapy was carefully assessed every 4 weeks during treatment and at its end. Treatment with SAI was accompanied in 33.3% of cases by complete hair restoration, in 53.3% of cases - partial, i.e. a reduction of more than 50% of the affected surface, and in 13.3% of cases - no effect. These results in terms of effectiveness significantly exceeded those of the placebo-controlled group (p < 0.01), where complete hair restoration was not recorded, partial restoration was noted in 28.5% of cases, and no effect in 71.5% of cases.
The mechanism of hair restoration, according to GM Galbraith et al. [38, 39], is due to increased T-cell function under the influence of SAI. These authors also obtained clinically significant results with hair restoration in 7 patients with alopecia totalis in a series of 9 patients. Moreover, the positive effect of SAI on the function of the T-cell component of the immune system was noted in all observations. Similar clinical and laboratory results were obtained by M. Lowy et al. [41], who used SAI in patients with both total alopecia and focal hair loss. At the same time, along with the stimulation of immunocompetent cells, the disappearance of specific autoantibodies identified before the start of treatment with SAI was detected, with a positive correlation between positive clinical data on the effectiveness of therapy and laboratory parameters.
Dividing 50 patients with HPV-positive proliferative warty leukoplakia (PBL) of the oral mucosa into groups, F. Femiano et al. [42] in the first group (n = 25) combined treatment was used (SAI and surgical removal of PBL), and in the second group (n = 25) only surgical treatment was used. 18 months after combined treatment, relapse of PBL was registered in 4 (16.0%) cases, and after surgical elimination - in 18 (72.0%) cases, indicating the high effectiveness of SAI for HPV-associated diseases of the oral cavity.
Results of assessing the effectiveness of the use of SAI in pathologies of the cervix and external genitalia associated with HPV infection
In recent years, specialists from various fields of practical gynecology have begun to widely use AIS. Thus, active research in this direction is carried out under the guidance of professors V.N. Prilepskaya (at the Scientific Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov), V.P. Kozachenko (at the Russian Cancer Center named after N.N. Blokhin), E.E. Grigorieva (at Altai State Medical University), A.V. Zabelev (at Rostov State Medical University) and many others. This is evidenced by a series of works published in periodicals and scientific monographs [4–7, 49].
Practitioners use SAI for a variety of gynecological diseases, including genital herpes, cytomegalovirus, papillomavirus infections, and other combined pathologies, such as chlamydia and ureaplasmosis [50]. However, the main point of application of AIS are various gynecological diseases caused by viral and opportunistic pathogens. In our opinion, the results of the use of SAI in pathologies of the cervix, vagina and vulva associated with HPV infection are of particular interest to practitioners. Thus, the group of Professor V.N. Prilepskaya, for severe cervical dysplasia, classified as LSIL according to the Bethesda system, used SAI in a combined mode in 34 patients, 3 g per day for 5 days for 7–10 days before destruction and in mono mode in 29 women, 3 g per day day for 10 days. It should be noted that in all patients, LSIL foci were detected against the background of chronic cervicitis of combined etiology. The control group consisted of 34 women with a similar pathology of the cervix, who underwent only destruction of the pathological focus of the cervix. At the same time, the effectiveness of the combined regimen of SAI was 87.5%, and the effectiveness of mono-destruction of LSIL lesions was 65.6% with a relapse rate of 9.4 and 28.1%, respectively. The efficiency of elimination of HPV infection particles after combination therapy was 65.6%, and after mono-destruction of LSIL foci - 46.9%. A clinically pronounced effect of improving the well-being of patients with the cessation of pathological discharge (leucorrhoea) was found after monotherapy with SAI in 72.4% of cases, and the elimination of HPV infection virions was found in 65.5% of observations [6, 7].
In an open prospective study by A.G. Kedrova et al. [5] used SAI in a combined mode to 45 patients with dysplasia of varying degrees and cervical cancer (CC) in situ. In order to determine the tactics of treatment and management of patients depending on the severity of dysplasia, the patients were divided into 3 groups: 20 patients with grade I–II dysplasia; 15 women with grade III dysplasia and cervical cancer in situ; 10 patients with recurrent dysplasia and cervical cancer in situ. The main criterion for including patients in this study was HPV virus carriage, i.e. the presence of high-risk HPV genotypes (genotypes 16 and 18 or one of them). SAI was prescribed at a dose of 3 g per day for 10 days with a control examination for virus carriage 10 days after the end of the course of treatment, and the volume of surgical treatment was determined depending on the severity of cervical pathology. After the first course of treatment with SAI, in 77.8% of cases, the disappearance of HPV infection virions was noted in samples of materials taken from the affected areas of the cervix. Repeated SAI courses increased the effectiveness of this approach, and therefore the authors completed additional courses in 13 cases.
In the work of KC Mohanty and CS Scott [51], the effectiveness of SAI was studied for multiple genital condylomas (more than three condylomas) in both women and men. In 145 patients, divided into 3 groups, the traditional method of removing condylomas (podophyllin), SAI, or a combination of traditional therapy with SAI was used. Although the effectiveness of the use of SAI itself did not differ from traditional therapy, the addition of traditional SAI therapy significantly increased the effectiveness of treatment from 41 to 94%. Moreover, the use of SAI was successful in long-term persistent genital warts. According to the results of a multicenter, double-blind, placebo-controlled study conducted by J. Davidson-Parker et al. [52], additional use of SAI 3 g daily for 4 weeks improved the results of traditional treatment with podophyllin in 55 patients with long-term (at least 12 months) genital warts. The therapeutic effect of SAI was especially more pronounced in severe clinical manifestations of HPV with recurrent multiple and large condylomas. S. Georgala et al. [53] in a randomized placebo-controlled study, using SAI at a dose of 50 mg/kg for 12 weeks, also showed high efficacy and safety of this drug.
Clinical, experimental and laboratory studies have proven that SAI stimulate the activity of immunocomponent cells (monocytes, macrophages and NK cells) in terms of both chemotaxis and phagocytosis, as well as antigen processing and presentation, and enhance the production of cytokines (interferons and interleukins). SAIs also stimulate the proliferation of lymphocytes (accelerate the differentiation of pre-T-lymphocytes, stimulate mitogen-induced proliferation of T- and B-lymphocytes), increase the total number and increase the functional activity of T-lymphocytes, stimulate the formation of lymphokines, enhance the production of interleukin-2 and interferon, normalize CD4/CD8 ratio, increase the ability of cells to respond to lymphokines and chemotactic factors. Thanks to these properties, SAI can be used for the treatment and prevention of acute and chronic viral infections.
Thus, literature data indicate the need to use immunomodulatory agents to correct diseases caused by opportunistic pathogens, which is associated with the growing number of patients with secondary immunodeficiency. This requires a search for the most acceptable and adequate immunopotentiator that does not have the side and pleiotropic effects inherent in exogenous cytokines. As a suitable immunomodulator, a medicinal analog of inosine, Groprinosin (inosine pranobex), is presented, a metabolite of natural purines, which initiates the production of interferons, interleukins and other cytokines, activates immunocompetent cells, and also balances the balance of the cellular and humoral components of the immune system and thus builds the body's antiviral defense, which is especially important in difficult patients.
Research results
Evaluation of clinical effectiveness
An assessment of the clinical effectiveness of therapy, based on the dynamics of granularity of the posterior pharyngeal wall, hypertrophy of the tonsils, lymphadenopathy and hepatomegaly, is presented in Table 3.
When comparing the severity of granularity of the posterior pharyngeal wall, it is clear that the most pronounced restoration of the mucous membrane of the posterior pharyngeal wall during the therapy was in patients receiving a course of antiviral therapy with inosine pranobex in combination with meglumine credone acetate. In all study groups, changes in the size of the palatine tonsils before and after therapy, as well as in the comparison group, were statistically insignificant. When comparing the degree of lymphadenopathy expressed in points (Mann-Whitney test), it was found that the differences in the groups were statistically insignificant, with the exception of the group with inosine pranobex therapy in combination with recombinant IFN, where statistically significant differences were noted (p = 0.036). The severity of lymphadenopathy was higher before therapy than after therapy (1.5 and 1.0 points, respectively). Thus, the most rapid decrease in the severity of polylymphadenopathy occurred in patients receiving therapy with inosine pranobex in combination with recombinant IFN.
When comparing liver sizes, it was revealed that in the group of patients receiving therapy with a combination of inosine pranobex + recombinant IFN, the indicator before and after therapy had statistically significant differences (p = 0.003 by Student's t-test).
Thus, the clinical effect, assessed using established criteria (see Table 2), was achieved in the majority of patients who received antiviral therapy. The largest proportion of patients with a complete clinical effect, i.e., no respiratory infections for 3 months. from the beginning of observation, was in the group of therapy with inosine pranobex in combination with recombinant IFN - 86%, in the group of monotherapy with inosine pranobex, a complete clinical effect was achieved in 75% of patients, in the group of therapy with inosine pranobex in combination with meglumine acridone acetate - in 63%, and in in the comparison group that did not receive etiotropic therapy - only in 8% of cases. The differences between patients receiving therapy and patients in the comparison group were statistically significant.
Assessment of virological effectiveness
The structure of GVI before and after treatment is presented in Figure 1. In total, before the start of therapy, reactivation caused by HHV-6A/B was recorded in 85.8% of children, caused by EBV - in 35.6%, caused by CMV - in 7.5% caused by HSV-1 - in 16%. Before therapy, monoinfections were diagnosed in more than half of the cases; combined HVIs were diagnosed in 41% of patients; of these, mixed HHV-6A/B + EBV was most often detected - in 23% of cases. After treatment, 63% of patients had a latent infection with HHV-6A/B, the proportion of mixed infections was 8%.
Virological effectiveness was assessed by the proportion of patients with active forms of BBVI in the groups before and after treatment. The proportion of patients with active HHV-6A/B infection after antiviral therapy (65 patients) was 35.4% (23 patients), and in the comparison group (26 patients) this figure was 69.2% (18 patients). When comparing the frequency of HHV-6 reactivation depending on the presence of etiotropic treatment with the drug inosine pranobex (as monotherapy and in combination with other antiviral agents), statistically significant differences were identified (p<0.01). Thus, the use of etiotropic therapy reduces the chances of GVI reactivation by 4.11 times (95% CI 0.092–0.646). There was an average relationship between the compared characteristics (V=0.307).
Material and methods
We examined 91 children aged from 3 to 17 years (mean age 6.9±0.42 years), who were observed on an outpatient basis with complaints of monthly infections of the respiratory tract during the previous 3 months. and laboratory confirmed active forms of GVI, including combined forms.
The patients were divided into 4 groups depending on the treatment method. In group 1, 12 children received treatment with inosine pranobex according to the following regimen: inosine pranobex for 10 days, then a 10-day break, then inosine pranobex for 10 days. In group 2, 29 children received inosine pranobex for 10 days, then recombinant IFN-α2b in the form of rectal suppositories for 10 days, then inosine pranobex for 10 days. And in the 3rd group, 24 children were prescribed therapy with inosine pranobex for 10 days, then meglumine acridone acetate according to the scheme on days 1, 2, 4, 6, 8, 11, 14, 17, 20, 23. The comparison group consisted of 26 children who received local therapy for inflammatory changes in the oropharynx with herbal medicines. The dose of inosine pranobex according to the manufacturer's instructions was 50–75 mg/kg/day, divided into 3–4 doses. The groups were comparable in age and gender characteristics (Table 1).
All patients underwent a comprehensive clinical and laboratory examination before the start of therapy, as well as after completion of treatment. Diagnosis of GVI was carried out on the basis of indirect and direct data.
Using the PCR method with hybridization-fluorescence detection of real-time analysis results, DNA of type 5 HHV, type 6 HHV, and type 4 HHV was detected and quantified in peripheral blood samples and oropharyngeal smears. The PCR study was carried out using reagent kits developed at the Central Research Institute of Epidemiology of Rospotrebnadzor.
Blood and oropharyngeal swabs were tested for the presence of viral antigens. The rapid culture method (vero, u937) was used to detect early HHV-6 antigens in blood serum, blood cells, and oropharyngeal smears. Using the indirect immunofluorescence reaction (experimental test systems created at the N.F. Gamaleya National Research Center for Epidemiology and Epidemiology of the Russian Ministry of Health), late antigens of HHV-6 were detected in blood serum, blood cells, and oropharyngeal smears.
The enzyme immunoassay method was used to determine virus-specific IgM and IgG to the proteins HSV-1, EBV, and CMV using kits (Russia). Detection of specific IgG to HHV-6 antigens was carried out by enzyme immunoassay using a set of reagents “VectoHHV-6-IgG” (RU No. FSR 2011/09853 2166, JSC “Vector-Best”, Russia) on an automatic enzyme immunoassay analyzer Freedom EVOlyzer 200 (TECAN Schweiz AG, Switzerland). The concentration of virus-specific IgG was assessed by the positivity rate: positive result ≥1.0; borderline - from ≥0.8 to <1.0; negative - <0.80.
Acute primary infection was diagnosed in the presence of viremia, increased IgM levels, and the absence of IgG. Reactivated infection was defined as viremia and an increase in IgG levels by 2.5 times or more. An increase in IgG and/or the presence of viral DNA in an oropharyngeal smear without viremia was regarded as a manifestation of a latent form of infection.
To objectively assess data before and after prescribing a course of study drugs, a ranking scheme for clinical signs was used, presented in Table 2.
The virological and complex clinical effectiveness of treatment was also assessed depending on the manifestations of acute respiratory disease (ARI): complete effectiveness - absence of ARI for 3 months. from the start of therapy; incomplete effectiveness - reduction in the number of acute respiratory infections and/or reduction in severity; lack of effectiveness - persistent monthly acute respiratory infections.
Statistical data processing
was carried out using Microsoft Office Excel 2016, IBM SPSS Statistics v.26. For quantitative indicators with a normal distribution, arithmetic means (M±SD) were calculated; Student's t-test was used to compare samples; in case of non-normal distribution, medians (Me) and interquartile range (Q1–Q3) were calculated, and the Mann-Whitney U test was used to compare populations. Nominal data is described with absolute values and percentages. Comparisons of nominal data were made using Pearson's χ2 test and Fisher's exact test. Differences were considered significant at p<0.05.