Introduction
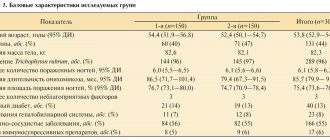
The global trend in the structure of the population is expressed in a significant increase in the proportion of older people.
Compared to 2005, in 2010 the increase in the population over 60 years of age was 6.9%. However, according to WHO, in 2010 there were 524 million people over 60 years of age in the world, which amounted to 8% of the total world population. Demographer calculations indicate that the rate of population aging in the Russian Federation may be faster than the global rate. Population aging is projected to be particularly evident in large cities [1]. Thus, the proportion of people 60 years of age and older in St. Petersburg remains one of the highest (21.1%) compared to other territories of the Russian Federation (18.9%). In addition, life expectancy in St. Petersburg for people aged 60–64 years was 15.9, for residents 75–79 years old – 7.8 years, and for residents 85 years old and older – 5.8 years [2] . Thus, diagnosis, prevention and treatment of chronic diseases associated with age should become a priority in the organization of geriatric medical care. Osteoporosis (OP) fully refers to chronic diseases of the musculoskeletal system and connective tissue associated with age (ICD, class XIII). The main complication of AP, which has a significant impact on the quality of life and its duration, are fractures that develop with minimal trauma or impact on the skeleton [3]. The incidence of osteoporotic fractures increases with age, and more than 50% of all osteoporotic fractures occur in people over 75 years of age. Large-scale epidemiological studies have shown that the prevalence of vertebral fractures among women aged 55–65 years is 7.8 cases per 1000 person-years, reaching a level of 19.6 among people over 75 years of age [4]. In addition, for older people with a history of previous fractures, the risk of recurrent fractures of any location increases significantly due to loss of both bone and muscle mass [5].
Some works devoted to the analysis of medical care for patients with AP say that older people do not receive fully adequate treatment [6]. Failure to treat when indicated leads to increased hospitalizations and overall medical costs. The current situation may be due to two main reasons. First, older patients are not included in clinical trials; therefore, the effectiveness and tolerability of available drugs remain unclear. Secondly, complex rules for taking anti-osteoporotic drugs (primarily oral bisphosphonates [BPs]) create additional difficulties, especially in the presence of cognitive impairment and functional limitations due to multiple concomitant pathologies (comorbidity).
Diagnostics of AP
Currently, the diagnosis of AP, based on the use of dual-energy X-ray densitometry (DXA - Dual-Energy X-ray Absorptiometry), has widely entered the clinical practice of many medical organizations. To establish a diagnosis, it is necessary to measure bone mineral density (BMD) in the hip (femoral neck - Neck, proximal femur - Hip) and/or spine (L1-4). Densitometry indicators also allow for monitoring treatment and assessing the risk of fractures. For people over 50 years old, the T-criterion is applicable. According to the diagnostic criteria proposed by WHO, the T-score should be < -2.5 standard deviations (SD) [7].
A WHO expert group led by J. Kanis (2008) created an algorithm for identifying patients at high risk of fractures associated with AP. Using the FRAX (Fracture Risk Assessment Tool) mathematical model, it is possible to calculate the 10-year probability of a femoral neck fracture and other fractures typical of AP in individuals aged 40 to 90 years [8]. This method is based on the interaction of clinical risk factors for fractures, namely age, the presence of a fracture of the proximal femur in parents, a history of fractures in the patient himself, taking glucocorticosteroids, smoking and alcohol, the presence of rheumatoid arthritis with or without data on hip BMD.
Strategy for the prevention and treatment of AP
Of course, the prevention of AP and fractures should become the dominant strategy in treatment, since quantitative (decreased BMD) and qualitative (impaired microarchitecture) changes in bone tissue are practically irreversible. Prevention of AP involves achieving maximum peak bone mass during the period of predominance of bone formation processes through a balanced diet, sufficient daily physical activity and the elimination of bad habits (smoking and alcohol abuse). Once peak bone mass is reached (around age 25–30), prevention is based on the principle of preserving bone mass. For this purpose, women in the early period of menopause should be given special attention. Hormone replacement therapy with estrogens, with or without progestogens for women and androgens for men (if they are deficient), can solve this problem. For the older population, minimizing bone loss is the main principle of preventing AP. It is in this population that drug therapy and drug prophylaxis are of particular importance.
An analysis of all phase III randomized clinical trials (RCTs) lasting at least 3 years, conducted to determine the antifracture effect of antiosteoporotic drugs, shows that their use can reduce the relative risk of vertebral fractures by 30–70%, and hip fractures by 30–30%. 51%.
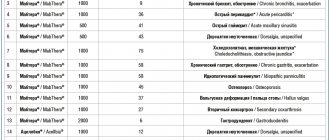
These data allow us to calculate an indicator such as the number of patients who need to be treated with a drug to prevent one fracture (number needed to treat - NNT). Thus, to prevent one vertebral fracture, it will be necessary to treat from 9 to 21 patients over 3 years, and more than 48 people will need to treat a hip fracture [9]. Various international and national guidelines favor the preferential use of antiosteoporotic drugs, which have been shown in RCTs to be effective against compression fractures of the spine, hip and other non-vertebral fractures. These drugs include alendronate, risedronate, zoledronic acid, denosumab, teriparatide, and strontium ranelate (Table 1) [10].
BD are the most widely used in clinical practice. They have shown their effectiveness in preventing bone loss caused by involutive processes during aging, estrogen deficiency in menopausal women and the use of glucocorticosteroids, which was accompanied by a reduction in the risk of fractures in postmenopausal, glucocorticosteroid osteoporosis and osteoporosis in men. BPs began to be used in clinical practice 45 years ago (etidronate - since 1977, pamidronate - since 1991). However, the first nitrogen-containing BP registered for the treatment of postmenopausal osteoporosis was alendronate (1995), followed by risedronate (2001), ibandronate (2005) and zoledronic acid (2007).
Ultimately, the decision to use a particular drug is made depending on the specific clinical situation, registered indications (Table 2), the risk of side effects, patient preferences and other reasons. Indeed, there is no one anti-osteoporotic drug that could be used by all patients with AP. However, intolerance to one of the drugs will require transferring the patient to another drug.
Prevention of fractures in older people
Age as a major determinant of treatment response has been examined in RCTs that examined the effect of alendronate, risedronate, zoledronic acid, strontium ranelate, teriparatide, denosumab, and HRT on the risks of vertebral and nonvertebral fractures.
It was not possible to assess the effect of oral supplements on the risk of nonvertebral fractures because the number of people over 80 years of age (or even 75) was small. The design of the main RCTs did not address this issue, and therefore the confidence interval turned out to be quite wide. Thus, in RCTs of HIP and VERT, the effectiveness of risedronate on the risk of vertebral fractures was approximately the same for patients both older and younger than 80 years [11, 12]. The number of nonvertebral fractures significantly decreased only in the group of patients under 80 years of age [13]. Similar data were obtained in the FIT (Fracture Intervention Trial) RCT, which reported a reduction in the relative risk of vertebral fractures in a subgroup of patients over 75 years of age during alendronate therapy [14].
An RCT that examined the effectiveness of teriparatide among 1085 women showed that the incidence of vertebral fractures was similar in subgroups of patients younger and older than 75 years [15]. However, the risks of nonvertebral fractures were reduced only for patients younger than 75 years.
A special feature of strontium ranelate was the evidence of its effect on the risks of vertebral and non-vertebral fractures in women over 80 [16]. A large prospective study, the WHI (Women's Health Initiative), found no effect of HRT on the risk of fractures in different age groups [17].
Features of the use of zoledronic acid in AP
It is known that BP belongs to the class of antiresorptive drugs. They have a high affinity for mineralized bone tissue and bind strongly to the calcium phosphate in hydroxyapatite, especially in areas of high bone turnover. Several independent studies have shown that the point of application for BP is the enzyme farnesyl pyrophosphate synthase, which is involved in lipid synthesis through the mevalonic pathway. Inhibition of this enzyme helps slow osteoclast-mediated bone resorption and causes osteoclast apoptosis. Zoledronic acid inhibits the activity of farnesyl pyrophosphate synthase tens of times more actively than other BPs [18]. Obviously, this feature of zoledronic acid allows it to be administered less frequently and in lower dosages than other BPs.
With a single intravenous administration of zoledronic acid, peak plasma concentrations are reached at the end of the infusion and then rapidly decrease. After 24 hours, less than 1% of the active substance is detected in the blood, 43–55% of zoledronic acid binds to plasma proteins, regardless of their concentration. Zoledronic acid is not metabolized in the human body, but is excreted unchanged by the kidneys. Up to 40% of the active substance is excreted on the first day after its administration. The rest enters the bone tissue and is slowly released into the circulation. The clearance of zoledronic acid depends on renal function, however, even with a glomerular filtration rate of 35–50 ml/min, the exposure does not change and, thus, no dose adjustment is required. However, treatment with zoledronic acid is not recommended if glomerular filtration rate decreases below 35 ml/min [19]. There were no changes in the pharmacokinetics of the drug depending on race and age (from 38 to 84 years). A single administration of zoledronic acid leads to a rapid decrease in biochemical parameters characterizing the process of bone resorption (by approximately 30–55%). Then, almost simultaneously, a decrease in bone formation occurs. Repeated annual administrations of the drug are not accompanied by a progressive decrease in biochemical markers of bone resorption. The lowest values of biochemical markers of bone resorption were recorded 7 days after the administration of zoledronic acid at a dose of 5 mg, and bone formation - by the 12th week.
The effectiveness of zoledronic acid was demonstrated in the randomized, double-blind, placebo-controlled international study HORIZON-PFT (Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly – Pivotal Fracture Trial), which recruited 7736 women aged 65 to 89 years. The vast majority of patients were aged 70–74 years (38% of the total population). Inclusion criteria: menopausal women with hip T-score BMD ≤ -1.5 SD and 2 mild or one moderate vertebral compression fractures, or BMD ≤ -2.5 SD with optional vertebral fractures. Patients should not have previously received any anti-osteoporotic therapy other than calcitonin, hormone replacement therapy, or selective estrogen receptor modulators. All study participants required 1000–1500 mg of calcium and 400–1200 IU of vitamin D daily. The duration of the study was 3 years, the main goal was to study the effect of the drug on the risks of vertebral fractures and hip fractures. As a result of treatment with zoledronic acid at a dose of 5 mg once a year, the absolute reduction in vertebral fractures was 7.6% over 3 full years of observation; accordingly, the relative risk decreased by 70% (in the 1st year - by 60%, in the 2nd year - by 71%) compared with the placebo group [20]. There was also a significant relative reduction in the number of hip fractures by 41% among patients receiving 3 infusions of zoledronic acid over 3 years. The absolute incidence of fractures in the placebo group was 2.5% and in the zoledronic acid group it was 1.45%.
A persistent decrease in vertebral and hip fractures over 3 years of follow-up occurred regardless of age, number of registered fractures at the start of the study, regional and racial characteristics, body mass index, and BMD level.
In patients over 75 years of age, the relative reduction in the risk of hip fracture was greater, reaching a 60% reduction compared with the placebo group (p < 0.0001). The result of treatment was also a reduction in the risk of all clinical fractures by 33%, clinical vertebral fractures by 77, non-vertebral fractures by 25%. The number of multiple vertebral fractures decreased by 89% (0.2% in the intervention group and 2.3% in the placebo group).
The reduction in the risk of all osteoporotic fractures was accompanied by an increase in BMD in various areas of the femur and spine after 6, 12, 24 and 36 months from the start of observation. A histomorphological study of bone tissue was carried out among patients receiving zoledronic acid.
Thus, despite the suppression of bone turnover, the process of bone remodeling persisted in all (except one) iliac bone biopsies [82]. There was no evidence of impaired bone quality among postmenopausal women. In addition, no cases of frozen bone, bone marrow fibrosis, or cellular toxicity have been reported. Indirect evidence was obtained of the positive effect of zoledronic acid on the strength of cancellous and cortical bone based on the results of quantitative computed tomography [21].
Another study using microspectroscopy on decalcified bone revealed an anabolic effect of zoledronic acid on the bone matrix in addition to its primary antiresorptive effect [22].
Several studies that administered zoledronic acid at varying frequencies (placebo, 1 or 2 doses) to postmenopausal women with reduced BMD (osteopenia) for 2 years demonstrated a preventive effect of the drug [23].
The RCT, designed to determine the effect of zoledronic acid on the risk of recurrent fractures, included patients who developed the most life-threatening hip fracture. 2,127 men and women over the age of 50 took part in the HORIZON-RFT (HORIZON-Recurrent Fracture Trial) study. Zoledronic acid was administered to patients for 3 months after surgery (endoprosthetics, metal osteosynthesis) [24]. If 25(OH)D was <15 ng/mL, these patients received high-dose vitamin D (50,000–125,000 IU) 14 days before study drug administration, followed by 800–1200 IU vitamin D and calcium daily. The relative risk of new clinical fractures after an average of 1.9 years decreased by 46%, and all nonvertebral fractures by 27.0%. The relative risk of recurrent hip fractures was reduced by 30%, but no statistically significant difference was achieved due to the small number of cases.
An additional analysis of the same study showed that overall all-cause mortality was significantly reduced by 28% among patients receiving zoledronic acid [25].
The effectiveness and safety of zoledronic acid in the treatment and prevention of glucocorticosteroid AP were studied in a randomized, multicenter, double-blind, placebo-controlled, active-controlled study. The study included 833 men and women aged 18–85 years who received oral prednisolone (or similar glucocorticosteroids) at a dose of at least 7.5 mg per day. Prophylactic treatment was carried out in a group of patients who began receiving GCs 3 months before randomization. The treatment group was formed from patients who received glucocorticosteroids for more than 3 months. Patients were prescribed either intravenous zoledronic acid or oral risedronate 5 mg daily. The study demonstrated that zoledronic acid had no worse effect on BMD than risedronate, and BMD in the lumbar spine increased in the treatment group by +4.06% (versus 2.71%), and in the prevention group by +2.6% (vs. 0.64%) after 12 months of follow-up. A statistically significant increase in BMD in the lumbar spine was observed among postmenopausal women and men. The number of registered vertebral fractures during the observation period was small, so there were no differences in the comparison groups [26]. Additional analysis of the same study found that the benefit of zoledronic acid was an increase in BMD at both the lumbar spine and femur in premenopausal women. The positive effect on BMD indicators developed regardless of age, gender and duration of menopause [27].
In order to study the effectiveness of zoledronic acid for men, E. Orwoll et al. (2010) conducted an RCT that included 302 men with osteoporosis aged 25–86 years (mean age 64 years). Patients divided into two comparison groups were treated for 2 years. The first group received two injections of zoledronic acid; the comparison group received alendronate 70 mg per week. Additionally, all patients were prescribed combined calcium (1000 mg) and vitamin D (800–1000 IU) daily. An increase in BMD in the lumbar vertebrae was observed in both groups (+6.1 and +6.2%, respectively), which proves the possibility of using zoledronic acid in men with AP [28].
An additional pooled analysis of data from two RCTs (HORIZON-PFT and -RFT) was conducted to evaluate the effectiveness of zoledronic acid in older adults. Zoledronic acid was prescribed to 4,761 patients over 65 years of age and 2,083 over 75 years of age. There were no differences in the efficacy and tolerability of zoledronic acid among patients of different age groups [20]. However, a more pronounced effect on the risk of vertebral fractures developed among women aged <75 years [29]. The HORIZON-PFT RCT was the first study using BF to show a significant reduction in non-vertebral fractures among people over 75 years of age [30].
An RCT performed by the authors' group showed that a single dose of zoledronic acid combined with daily teriparatide resulted in a greater increase in spinal BMD than was observed with teriparatide alone at 13 weeks of follow-up. After one year, spine BMD in the groups of patients receiving teriparatide and teriparatide in combination with zoledronic acid was approximately the same, but was higher compared to those who used only zoledronic acid. Moreover, combination therapy resulted in a rapid, significant, and consistent increase in BMD at all hip sites measured, in contrast to zoledronic acid or teriparatide monotherapy at 13 weeks. There were no differences in the incidence of adverse events in the compared groups [31].
The problem of compliance in long-term treatment of chronic non-infectious diseases is discussed quite widely in the literature. It is obvious that in the absence of proper compliance on the part of patients, it is impossible to achieve comparable treatment results demonstrated in RCTs. In one of the latest scientific articles published by JR Curtis et al. (2013), it is stated that 67% of general practitioners, when prescribing anti-osteoporotic drugs, were optimistic about the adherence to treatment of their patients. However, in reality, only 40% fully complied with recommendations for drug therapy for AP [32]. In this regard, the availability of zoledronic acid for intravenous administration certainly not only improves adherence, but also contributes to the organization of strict control over the volume of therapy and its effectiveness.
An analysis of comparative studies (zoledronic acid and alendronate, zoledronic acid and risedronate) showed that patients in 78.7% of cases preferred the administration of zoledronic acid once a year than the use of oral forms of BP in the regimen of 1 tablet per week. At the same time, 9% of patients were in favor of taking tablet forms of BP [33].
Among the specific serious adverse events reported with the use of intravenous forms of BP, the most frequently discussed are atrial fibrillation, atypical (subtrochanteric) femoral fracture, osteonecrosis of the mandible and damage to the upper gastrointestinal tract (mainly the esophagus). In older people, the most relevant side effect is atrial fibrillation, which was recorded in the HORIZON-PFT study in 1.3% of cases among patients receiving zoledronic acid, and only 0.5% in the placebo group (p < 0.001). However, no chronological relationship was identified between the drug infusion itself, its pharmacokinetic profile and atrial fibrillation. Almost all women had signs of sick sinus syndrome before treatment. In terms of indicators that included cardiovascular death, strokes and other cardiovascular adverse events, excluding all types of arrhythmias, the comparison groups did not differ. However, any arrhythmias recorded on the ECG were more common than in the placebo group (6.9 vs. 5.3%; p = 0.003). It was found that ventricular fibrillation occurred somewhat more often among patients over 85 years of age [34].
For older people with low BMD (osteopenia) receiving glucocorticosteroids, as well as with diagnosed AP, BF remains the drug of choice for both men and women. Zoledronic acid may be considered an alternative to oral forms of BP in cases of the presence or development of esophagitis, peptic ulcers, or exacerbation of other gastrointestinal diseases. It is possible to use zoledronic acid as the first anti-osteoporotic drug at the request of the patient. If there are factors that contribute to low patient adherence, zoledronic acid may be considered a priority drug.
Efficacy and safety of zoledronic acid in older women with osteoporosis
85% of elderly patients living in specialized institutions have osteoporosis, as well as an 8-9 times increased risk of developing fractures, compared with people of the same age, but living at home. Despite this, they are rarely included in osteoporosis studies.
Target.
To evaluate the effectiveness and safety of zoledronic acid in the treatment of osteoporosis in elderly frail women undergoing long-term treatment in specialized medical institutions.
design .
The two-year, randomized, placebo-controlled, double-blind study, conducted from December 2007 to March 2012, enrolled 181 women aged 65 years or older with osteoporosis, including those with cognitive impairment, immobility, and several comorbidities. All patients lived in nursing homes or specialized medical institutions. Participants were prescribed 5 mg zoledronic acid or placebo intravenously once daily and calcium and vitamin D supplements. Endpoints included hip and spine mineral density at 12 and 24 months after initiation of therapy and the number of adverse drug events. .
Results.
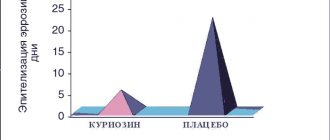
There were no differences in the baseline characteristics of the included patients in terms of age (mean 85.4 years), functional status, or cognitive status. Moreover, in the group of patients where zoledronic acid was prescribed, there were more weakened individuals, women with a history of falls, diabetes mellitus, and the use of anticonvulsants. The mean change in femoral bone mineral density was greater in the zoledronic acid group, 3.2% at 12 months and 3.9% at 24 months (P<0.01 for both comparisons), and 1.8% and 3.6% for the spine (P<0.01). 0.01). Fractures occurred in 16% of patients receiving placebo and 20% of those receiving zoledronic acid (OR, 1.30; 95% CI, 0.61-2.78); death occurred in 13% and 16%, respectively (OR, 1.24; 95% CI, 0.54–2.86). There was no difference in the incidence of single falls (28% in the study group vs 24% in the control group; OR, 1.24; 95% CI, 0.64-2.42; P = 0.52), however, multiple falls were more common in patients receiving zoledronic acid ( 49% vs 35%; OR, 1.83; 95% CI, 1.01-3.33; P = 0.047). After controlling for baseline characteristics, the difference between groups did not reach statistical significance.
Conclusion.
Administration of zoledronic acid to elderly patients with osteoporosis is associated with an increase in bone mineral density over 2 years. The clinical significance of the statistically nonsignificant increase in fracture risk and mortality should be examined in future studies.
Source:
Susan L. Greenspan, MD;
Subashan Perera, PhD; Mary Anne Ferchak, BSN; David A. Nace, MD; Neil M. Resnick, MD. Efficacy and Safety of Single-Dose Zoledronic Acid for Osteoporosis in Frail Elderly Women A Randomized Clinical Trial JAMA Intern Med. 2015;175(6):913-921. Prepared by:
Evsyutina Yu.V.