November 14, 2018
All tests in 1 day
One type of laboratory diagnosis is a general blood test. It allows you to identify a large number of pathologies, such as malignant tumors, infectious, inflammatory diseases, etc. It can also be used to evaluate the effectiveness of patient treatment. After all, a general blood test can tell a lot about the state of the body.
Only specialized doctors can correctly decipher a general blood test. Therefore, without the appropriate medical knowledge, you should not even try to do it yourself. But it will not be superfluous to know by what indicators the blood is analyzed, as well as the norms of the test result. You will find this information in our article.
Red blood cells
Erythrocytes, or red blood cells, ensure the delivery of oxygen to all cells of the body. In English-language literature, red blood cells are called “red blood cells,” which is where the international abbreviation RBC .
To transport oxygen, these cells contain hemoglobin, which can combine with it through chemical reactions. The analyzer displays the following indicators regarding these processes:
- RBC is the number of red blood cells per liter of blood. An increase in this indicator in humans can be observed with various neoplasms, hormonal disorders, but much more often it is the result of blood thickening due to dehydration, burns, taking diuretics and some other reasons. A decrease in RBC is observed with blood loss, anemia, disorders of their formation or increased destruction. A slight decrease in the number of red blood cells during pregnancy is normal.
- HGB - total hemoglobin content. The indicator grows following an increase in RBC and decreases for the same reasons. A decrease in HGB is also observed during hemodilution—blood dilution, for example, against the background of intensive intravenous administration of a large volume of solutions. Hemoglobin levels in women are usually lower than in men due to physiological blood loss during menstruation.
- HCT - hematocrit. This is a value that reflects the ratio of all blood cells to its liquid part - plasma. Since 99% of these cells are red blood cells, the indicator is used to estimate their volume.
Red blood cell indices
In addition, the so-called erythrocyte indices are assessed:
- MCV - average erythrocyte volume. Before the introduction of new analyzers, an accurate assessment was not carried out, and the result was designated as microcytosis, normocytosis or macrocytosis - depending on the size of the cells. An increased level of MCV may indicate a deficiency of vitamin B12, folic acid, hemolytic anemia, a decreased level may indicate iron deficiency and sideroblastic anemia.
- MCH is the concentration of hemoglobin in one red blood cell. In older analyzers, for this purpose, the color indicator was assessed, which is 0.03 of the MCH.
- MCHC is the average hemoglobin concentration in the erythrocyte mass, which reflects the degree of saturation of RBC with hemoglobin. It is the most stable indicator and can serve as an indicator of a correctly performed analysis.
All of the above indicators are closely related to each other and are assessed as a whole. For example, bleeding is accompanied by the loss of a large number of red blood cells. Accordingly, the total hemoglobin content also decreases, but MCH may remain normal. With a disease such as iron deficiency anemia, a slight deficiency of red blood cells occurs with a decrease in hemoglobin and various changes in erythrocyte indices. It makes no sense to list all possible changes in the body related to the content of red blood cells, and the doctor deciphers the result based on knowledge of those processes in the body in various diseases.
A separate indicator associated with red blood cells is their sedimentation rate - ESR (in modern analyzers - ESR) . This is a completely non-specific indicator, an increase in which indicates some problems in the body that the doctor needs to look for. In some cases, for example during pregnancy, an increase in ESR is physiological and is considered normal.
Errors in hemoglobin measurement
Inflated concentration results may be due to the following factors:
- Hyperlipidemia.
- Hyperbilirubinemia.
- Cryoglobulinemia.
- High leukocytosis.
- Excess of unstable hemoglobins.
Clinical and diagnostic value:
- Increased concentrations are caused by dehydration, as well as primary or secondary erythremia.
- Reduced concentration occurs with anemia or overhydration.
Some patients whose hemoglobin in the blood is higher than 75 g/l can increase the hemoglobin level by 20-30 g/l by taking iron supplements for 10 days, but the iron deficiency itself does not compensate. If a patient (body weight 70 kg) also receives a blood transfusion (500 ml), the hemoglobin level may increase by 12 g/l.
Leukocytes
Leukocytes are a large group of diverse cells whose task is to provide protection to the body. In international medicine, they are often referred to as WBC - white blood cells. This abbreviation denotes the total content of leukocytes in the analyzer form. The reason for the increase in WBC is various damaging factors: infections, injuries, ischemia and tissue necrosis, and others. Simply put, an increase in the number of white blood cells means that the immune system is actively involved in the fight against damage. At the same time, low values of the indicator may indicate a lack of immunity under the influence of radiation, medications, certain viral infections, as well as diseases that are accompanied by impaired formation or increased destruction of leukocytes.
Leukocyte indices
In addition, in assessing the content of leukocytes, leukocyte indices , or in old forms - leukocyte formula . The general clinical analysis with the latter is called detailed. There are several types of leukocytes, which differ from each other in morphology and functional characteristics. The leukocyte formula reflects their percentage of the total number, and modern analyzers also display the absolute content of each type of these cells. They can be identified on the form by the following abbreviations:
- LYM - lymphocytes;
- MXD - agranulocytes (monocytes, basophils and eosinophils);
- NEUT—neutrophils;
- MON - monocytes;
- EO - eosinophils;
- BA - basophils.
If there is a “%” sign after the abbreviation, then we are talking about percentage, and the “#” sign means their absolute content. Changes in the leukocyte formula can serve as an indicator of a wide variety of problems in the body. Let's take a closer look at them.
The main task of neutrophils is phagocytosis - the absorption of foreign objects and their destruction. They always rush to areas of inflammation and tissue breakdown, where they perform this work, so their increased content indicates active inflammation.
In addition to neutrophils, the function of phagocytosis is performed by macrophages, into which, in the process of their development, monocytes . A high level of the latter also serves as a marker of inflammation, usually of an infectious nature.
Eosinophils take part in reactions associated with the allergic component. An increase in their number is observed in allergies, parasitic infestations, some infections and cancer.
Basophils take part in inflammation and allergies by releasing heparin, histamine and serotonin. They rarely increase in isolation, although such a phenomenon in some forms of leukemia has a serious prognostic significance.
Lymphocytes are actively involved in a wide variety of conditions, including immunodeficiencies, allergies, inflammation, and autoimmune disorders. Their high content may be a sign of childhood infections, viral hepatitis, mononucleosis, tuberculosis and a number of other diseases.
Assessment of leukocyte indices and leukocyte formula requires an understanding of the pathological and physiological processes in the body, and should not be carried out solely on the basis of tabular data. You absolutely cannot diagnose yourself based solely on the results of the analysis.
Average hemoglobin concentration in erythrocyte MCHC
| Age | Women/Men (g/dL) |
| Blood from the umbilical cord | 30 — 36 |
| 2 weeks | 28 — 35 |
| 1 month | 28 — 36 |
| 2 months | 28 — 35 |
| 4 months | 29 -37 |
| 6 - 12 months | 32 — 37 |
| 1 - 2 years | 32 — 38 |
| 3 – 74 years | 32 — 37 |
The study is carried out using venous or capillary blood with EDTA salts. The indicator characterizes the amount of hemoglobin in an average red blood cell and is calculated in % using the following formula:
MCHC = Hb g/l * 10 / Ht%
This is one of the most stable and genetically determined parameters that are not influenced by age, gender or race. The concentration of hemoglobin depends on the structure of the cell and does not change throughout life, so the normal limits are quite narrow and practically not subject to fluctuations in various pathologies.
There is a clear upper limit for MCHC. This parameter may be determined incorrectly if the red blood cell count is inaccurate. With its help it is convenient to control the accuracy of the device.
Clinical and diagnostic value:
- An increased value occurs with hypertensive disorders in the water-electrolyte system or hyperchromic anemia.
- A decrease in the value of the indicator is typical for hypotonic disturbances of water-electrolyte balance or hypochromic anemia.
Important! Since the maximum solubility of hemoglobin in water is 37 g/dL, an MCHC value exceeding 37 indicates the need for re-testing. An increased value can also cause hemolysis.
Disturbances in water-electrolyte balance should be accurately determined using not absolute MCHC values, but their dynamics.
Platelets
The main task of platelets is to participate in stopping bleeding. They form the primary plug in the area of vessel damage and participate in the formation of a blood clot. In forms, automatic analyzers are designated by the abbreviation PLT , which comes from the English word platelets (literally, “saucers”) for their peculiar shape.
A decrease in the number of platelets can be accompanied by bleeding and is a consequence of diseases and conditions such as malaria, thrombocytopenic purpura, malignant neoplasms, disseminated intravascular coagulation syndrome and some others.
A high platelet count can cause excessive blood clotting and often has no apparent cause. In this case, the condition is designated as essential thrombocythemia. In addition, thrombocytosis can be caused by iron deficiency anemia, hemolysis, some infectious and autoimmune diseases, and bone marrow damage.
This is where the work with platelets in a classic blood test ends; however, automatic analyzers even in this case offer additional diagnostic capabilities in the form of the following indicators:
- MPV —mean platelet volume. An indicator reflecting the size of cells, which directly depends on their age. An increased MPV may indicate hematological diseases, damage to the spleen, thyrotoxicosis, and progression of atherosclerosis. A decrease in the rate is observed in some genetic diseases, myocardial infarction, childhood infections, cancer chemotherapy and a number of other conditions.
- PCT is the ratio of the total volume of platelets to blood plasma (thrombocrit). It is not a specific indicator, it varies widely physiologically, but it allows one to assess the risk of bleeding and thrombosis.
- PDW —platelet distribution by volume. The indicator has no independent meaning and is assessed in conjunction with other indices.
Average hemoglobin content in erythrocytes (MHC)
| Age | Women (pg) | Men (pg) |
| Blood from the umbilical cord | 31 — 37 | 31 — 37 |
| 2 weeks | 30 — 37 | 30 — 37 |
| 1 month | 29 — 36 | 29 — 36 |
| 2 months | 27 — 34 | 27 — 34 |
| 4 months | 25 — 32 | 25 — 32 |
| 6 months | 24 — 30 | 24 — 30 |
| 9 months | 25 — 30 | 25 — 30 |
| 1 year | 24 — 30 | 24 — 30 |
| 1 - 2 years | 22 — 30 | 22 — 30 |
| 38 years | 25 — 31 | 25 — 31 |
| 9 – 14 years | 26 — 32 | 26 — 32 |
| 15 - 17 years old | 26 — 34 | 27 — 32 |
| 18 – 44 years | 27 — 34 | 27 — 34 |
| 45 - 64 years | 27 — 34 | 27 — 35 |
| 65 - 74 years | 27 — 35 | 27 — 34 |
For research, venous or capillary blood with EDTA salts is used.
MHC is used to determine the average hemoglobin content in an individual red blood cell. To calculate the parameter use the following formula:
MHC pg = Hb g/l / RBC T/l
The numerator is the total hemoglobin value.
The denominator is the total number of red blood cells.
The parameter is defined in picograms. To determine the average amount of hemoglobin in red blood cells, a parameter such as the color index - CP - is also used. It is defined in conventional units.
CP = Hb g% * 3 / first 2 digits of red blood cell count
Or it is calculated using this formula:
CPU = MCH pg / 33.4
The CPU can completely replace the MCH. If an automatic hematology analyzer is used for research, which calculates the MCH value, then there is no need to additionally determine the CP.
Hyperchromia or an increase in MCH of more than 34 pg is not caused by an increase in the concentration of hemoglobin in erythrocytes, but is caused by an increase in their volume. A false overestimation of this indicator is possible due to errors caused by an increased level of hemoglobin and a reduced number of red blood cells. A decrease in MCH to 27 pg or less is called hypochromia.
Clinical and diagnostic value:
- An increase is possible with anemia due to liver cirrhosis, hyperchromic or megaloblastic anemia.
- The decrease is caused by anemia in malignant neoplasms, hypochromic anemia.
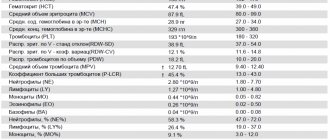
Table of normal blood test values
In conclusion, we provide a table of the main normal indicators of a general blood test in adults and children. We remind you that its results can only be assessed in conjunction with examination data, other laboratory data, including biochemical blood tests and instrumental diagnostic methods. In addition, reference, that is, acceptable, values depend on the type and model of diagnostic equipment. In this case, in the form of the automatic analyzer, next to the result obtained, normal values for a specific model are reflected.
| Index | Adults | Children | ||||||
| Men | Women | up to a year | 1-2 years | 2-4 years | 4-6 years | 6-10 years | 10-16 years | |
| RBC, *10^12/l | 4,3-5,7 | 3,8-5,1 | 4,1-5,3 | 3,8-4,8 | 3,7-4,9 | 3,8-4,9 | 3,8-5,2 | |
| HGB, g/l | 132-173 | 117-155 | 113-141 | 110-140 | 115-145 | 115-160 | ||
| HCT, % | 39-49 | 35-45 | 33-41 | 32-40 | 32-42 | 33-41 | 35-45 | |
| MCV, fl | 80-99 | 81-100 | 71-112 | 73-85 | 75-87 | 75-90 | ||
| MCH, pg | 27-31 | 31-37 | 24-33 | 26-32 | ||||
| ESR, mm/h | 2-15 | 2-20 | ||||||
| WBC, *10^9/l | 4-10 | 6-17 | 5,5-15,5 | 5,5 -15,5 | 4,5-13,5 | 4,5-13 | ||
| LYM#, 10^9/k | 1-4,8 | 2-11 | 3-9,5 | 3-9,5 | 1,5-7 | 1,5-6,5 | 1,2-5,2 | |
| NEUT#, *10^9/l | 1,8-7,7 | 1,5-8 | 1,8-8 | |||||
| MON#, *10^9/l | 0,05-0,8 | 0,05-1,1 | 0,05-0,6 | 0,05-0,5 | 0,05-0,4 | |||
| BA#, *10^9/l | 0-0,08 | |||||||
| EO#, *10^9/l | 0,02-0,5 | 0,05-0,4 | 0,02-0,3 | 0,02-0,5 | ||||
| PLT, *10^9/l | 180-320 | 160-390 | 150-400 | 180-450 | 150-450 | |||
| MPV, fL | 9,4 -12,4 | |||||||
| PCT,% | 0,108-0,282 | |||||||
Hematocrit
| Age | Women | Men |
| Blood from the umbilical cord | 42 — 60 % | 42 — 60 % |
| 2 weeks | 41 — 65 % | 41 — 65 % |
| 1 month | 33 — 55% | 33 — 55% |
| 2 months | 28 — 42% | 28 — 42% |
| 4 months | 32 — 44 % | 32 — 44 % |
| 6 months | 31 — 41 % | 31 — 41 % |
| 9 months | 32 — 40 % | 32 — 40 % |
| 1 year | 33 — 41 % | 33 — 41 % |
| 1 - 2 years | 32 — 40 % | 32 — 40 % |
| 35 years | 32 — 42 % | 32 — 42 % |
| 6 - 8 years | 33 — 41 % | 33 — 41 % |
| 9 – 11 years | 34 — 43 % | 34 — 43 % |
| 12 – 14 years old | 34 — 44 % | 35 — 45 % |
| 15 - 17 years old | 34 — 44 % | 37 — 48 % |
| 18 – 44 years | 35 — 45 % | 39 — 49 % |
| 45 - 64 years | 35 — 47 % | 39 — 50 % |
| 65 - 74 years | 35 — 47 % | 37 — 51 % |
For research, venous blood with EDTA salts is used, as well as capillary blood collected in a hematocrit capillary. In modern analyzers, hematocrit (Hct) is a secondary calculated parameter.
A false increase in hematocrit is possible when:
- Development of cryoglobulinemia.
- The presence of large platelets in the sample.
- Increased leukocyte count (more than 50 g/l).
- Hyperglycemia (more than 33.3 mmol/l).
False underestimation in hardware-based analysis causes:
- Agglutination of red blood cells.
- Microerythrocytosis (less than 36 fl).
Clinical and diagnostic value:
An increase in hematocrit is observed when at high altitude, the presence of tumors in the kidneys or their polycystic disease, chronic lung diseases, erythrocytosis, or conditions leading to a decrease in the volume of plasma circulating in the body - diabetes, non-stop vomiting, increased sweating).
The hematocrit value decreases with anemia or due to an increase in the volume of circulating plasma during pregnancy or overhydration.
Reasons for deviation from the norm
Factors that may lead to a decrease in the number of red blood cells:
- the formation of anemia in the body;
- insufficient intake of protein and vitamins from food;
- pathologies of the hematopoietic system;
- increased death of cellular elements due to exposure to toxic substances.
Reasons that cause an increase in the level of red blood cells in the blood:
- decreased fluid levels in the body;
- the occurrence of insufficiency in the respiratory and cardiovascular systems;
- pathological disorders in the hematopoietic system.
The main step when detecting changes in the number of red blood cells is to establish the pathology that led to this. To do this, it is recommended to undergo a comprehensive examination.
Indications for analysis
The diagnostic method for determining the number of red blood cells in the blood is a general blood test, which is taken by puncturing the capillaries of a finger or taking venous blood. Its implementation is recommended for every person who comes to a medical institution. In addition to determining the concentration of erythrocytes, in many cases the study of their additional characteristics is indicated: erythrocyte sedimentation rate (ESR), their average volume, hemoglobin content in erythrocytes.
The main indications for this analysis are:
- suspicion of anemia and determination of its type;
- monitoring the effectiveness of therapy for anemia;
- upcoming surgery;
- diagnosis of diseases of the hematopoietic system of the body according to indications or due to family history in children;
- assessment of the patient's condition after chemotherapy or radiation therapy;
- determining whether the patient belongs to any blood group;
- being in territorial zones that pose a danger due to infectious pathology of the circulatory system.
Changes in childhood
A pathological increase in the number of red blood cells in children is associated with various factors:
- with a low level of oxygen in maternal blood - the anomaly manifests itself in newborns;
- regular exposure of the baby to tobacco smoke (passive smoking);
- living in high mountain areas;
- regular sports activities.
A list of probable sources of deviation in children is presented:
- congenital heart defects;
- bone marrow dysfunction;
- hypertension in the pulmonary circulation;
- blood pathologies;
- obstructive pulmonary lesions with a chronic course;
- acute bronchitis, rhinitis or allergies;
- obesity of the last two degrees;
- dehydration caused by vomiting or diarrhea;
- disruption of the adrenal cortex.
Serious diagnoses associated with changes in the number of red blood cells include cancer of the kidneys and liver. Erythrocytosis is not an independent disease; it indicates latent pathologies or the presence of external influence factors.