Hematocrit - what is it, what does it depend on
Hematocrit analysis provides data on the ratio of the volume of red blood cells to the total volume of blood; sometimes this indicator refers to the ratio of the volume of all formed elements to the total volume. There is no particular difference between the interpretations; 99% of the blood cell volume is made up of red cells. More often, hematocrit is recorded as a percentage of the total volume, less often as a ratio of cell volume to total blood volume.
This indicator is determined as part of a general blood test complex. It is classified as secondary and is calculated based on data on the number of red blood cells. Occasionally, direct measurement of hematocrit is performed by centrifuging the sample. This procedure allows you to separate plasma from formed elements and directly measure this indicator.
Methods for determining hematocrit
The indicator is determined as a percentage by calculating the amount of formed elements in whole blood. It is calculated using special instruments or manually.
Centrifugation using the Wintrobe method
The blood is exposed to centrifugal force for 10-30 minutes. The formed elements are heavier than plasma, so they settle to the bottom of the test tube. The hematocrit is determined by the ratio of sediment to the total volume of biomaterial.
Calculation of the indicator using the formula
The ratio of the number of red blood cells to the total blood volume can be calculated mathematically. To do this, the following indicators are required:
- total hemoglobin concentration (ctHB);
- red blood cell count (RBC);
- mean erythrocyte volume (MCV);
- mean erythrocyte hemoglobin concentration (MCHC).
The hematocrit number (HCT) is determined by one of the formulas:
- HCT (%)=(ctHB (mmol/l)*0.0485+0.0083)*100
- HCT (%)=0.1*MCV*RBC
- HCT (%)=ctHB/MCHC*100
Direct blood cell counting method
In a given volume of biomaterial, visible blood elements are counted manually or using hematological analyzers. The method is highly accurate, and the measurement process does not take much time - no more than five minutes, but the equipment required is very expensive.
Manual counting method
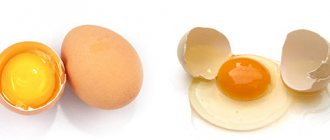
Blood collected using an anticoagulant is placed in a dry, clean tube and allowed to settle. In this case, the formed elements that have greater weight settle to the bottom of the container, and the light plasma rises to the top, forming two fractions of red and yellow colors, respectively. The hematocrit indicator can be determined by the divisions on the test tube. This method is the least accurate, its error is up to 20%, so it is currently not used in laboratories.
Indications and preparation for analysis
Indications for hematocrit analysis are symptoms indicating the development of anemia or other diseases of the blood or hematopoietic system. These include:
- Pale or jaundiced skin
- Enlarged spleen, liver
- Changes in the size of lymph nodes
- Digestive disorders
- Skin and hair problems (rashes, ulcers on mucous membranes, hair loss or brittleness)
In addition to identifying anemia, the analysis allows us to identify other diseases, for example, polycythemia (a chronic disease in which the bone marrow produces an excess amount of red blood cells) of various origins. This study is also used when it is necessary to assess the need for blood transfusion and calculate the required volume of transfusion.
No special preparation is required for the hematocrit test. It is necessary to follow the standard rules for conducting a general blood test:
- Blood is drawn early in the morning.
- You should not eat food 6-10 hours before the test.
- Avoid alcohol 2-3 days before the procedure.
Patients who smoke are advised to abstain from smoking for at least 2-3 hours before blood collection. If these recommendations are not followed, the analysis may give unreliable results. This is due to the fact that the composition of the blood is subject to strong fluctuations depending on the action of various environmental factors.
How does increased hematocrit manifest?
An increase in the specific gravity of red blood cells may not manifest itself in any way, or there may be individual, completely nonspecific symptoms:
- headache;
- dizziness;
- feeling of pressure in the head;
- dyspnea;
- fast fatiguability;
- skin itching;
- redness of the skin.
With such symptoms, a person may not see a doctor for a long time, but the problem may grow and lead to serious consequences.
See: Thick blood, Why I'm always cold, Complete blood count.
Blood test for hematocrit
The manipulation is performed in the morning, blood is taken from a vein or from a finger. At the Medart clinic, the most modern equipment is used for analysis, so the sampling is most often done from a vein.
To obtain the material, special vacuum containers (vacutainers) are used. This is a modern syringe replacement that provides a number of benefits for the patient:
- Virtually painless procedure.
- Minimum time to obtain the required amount of blood.
- Accurate calculation of the amount of reagent and blood.
- Minimum time for conducting the study and issuing results to the patient.
Modern technologies allow the procedure to be carried out as quickly as possible, without consequences for health.
Indications
The appointment of an OAC, which includes a hematocrit study, is included in the standard patient examination plan and is mandatory:
- when undergoing a medical examination and/or medical examination;
- if any disease is detected or suspected by a clinic doctor;
- in preparation for planned surgery;
- during hospitalization (on the day of admission and on the eve of discharge).
Calculation of the hematocrit number is required for certain indications;
- blood clotting disorder;
- dehydration (dehydration);
- assessment of the degree of anemia (anemia), polycythemia (increase in blood cells);
- bleeding.
Norms
The normal hematocrit level depends on the age and gender of the person. For a mature woman it is 37-50%, for a man 34-45%. For newborns, this figure may be higher and ranges from 35 to 65%. As people grow older, the hematocrit decreases, reaching minimal levels in the elderly. This is the result of decreased bone marrow activity and decreased production of blood cellular elements.
A decrease in normal hematocrit in women is associated with regular blood loss during menstruation. High values in children are a manifestation of active processes in the development of red bone marrow and other hematopoietic organs.
It is important to consider that after massive blood losses and blood transfusions, determining the hematocrit level will give results with a large error. To reliably assess this indicator in such cases, it is necessary to wait a certain time.
It may take up to 3 months for complete physiological restoration of red blood cell levels to normal levels. This period is the life cycle of red blood cells, during which the cellular composition of the blood is renewed.
The value of normal hematocrit in humans
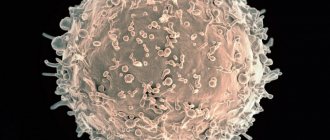
The body of a healthy adult contains approximately 4.5-5 liters of blood. It contains formed elements and cells - red blood cells, platelets, leukocytes, as well as a liquid part called plasma.
Some blood components, for example, red blood cells, do not have all the necessary components of a human cell, losing them during the maturation process. Therefore, red blood cells and platelets are called blood cells, not cells.
In different categories of patients, the normal values of various parameters of the blood tested will differ. So, for most men, the hematocrit will be higher: 40-41%, and in some cases it can reach up to 51%, which is due to its slower renewal.
In healthy women, the hematocrit usually ranges from 36 to 42%. This is due to physiological features - due to regular menstrual bleeding, blood is renewed more often to replenish its volume. During pregnancy, from the 20th week, the indicator begins to decrease, which is also not considered a deviation.
In children, hematocrit differs at different age periods:
- 44-62% for newborns;
- 32-43% for babies up to three months;
- 36-43% for children under one year of age;
- 35-47% (up to 52% for boys) - in the first ten years.
In subsequent years, the hematocrit norm depends on gender and practically corresponds to the values of an adult.
Hematocrit increased
An increase in the level of red blood cells detected in a hematocrit analysis may indicate various pathological conditions. The most common:
- Primary erythrocytosis. It occurs as a result of overactive production of red blood cells, including immature forms. May indicate the development of tumors in the bone marrow.
- Secondary erythrocytosis. Develops as a consequence of pathologies of the respiratory and cardiovascular systems (heart defects, respiratory failure).
- Reduced plasma volume. May indicate the development of peritonitis, leukemia, kidney disease. Often occurs with extensive burns, when blood plasma sweats through the damaged dermis.
- Dehydration. Observed in uncompensated diabetes mellitus, it can result from diarrhea, vomiting, excessive sweating and lack of fluid in the diet.
Erythrocytosis can develop in heavy smokers, especially if smoking has led to secondary damage to the respiratory system and heart. In this case, the body turns on mechanisms to compensate for insufficient oxygenation due to a significant increase in the number of red cells.
An increase in hematocrit is not always a consequence of disease. An increase in the number of red blood cells is considered normal for residents of mountainous areas and professional climbers. When exposed to high altitude conditions for a sufficiently long time, the body compensates for the lack of oxygen and atmospheric pressure by increasing the production of red blood cells.
Erythrocytosis is often asymptomatic and is discovered by chance during a blood test for other reasons. Only with a significant increase in hematocrit are the following observed:
- Pain in joints, muscles.
- Dyspnea.
- High blood pressure.
- Ringing in the ears and dizziness.
- Increased sweating, sleep disturbances.
These symptoms are not specific, so if such ailments occur, you should consult a doctor for further diagnosis.
To restore the physiological level of hematocrit, it is necessary to find out the reason that led to an increase in the amount of blood cells and eliminate it. For example, if erythrocytosis was caused by dehydration (lack of water in the body - dehydration), it is enough to restore the normal amount of fluid to normalize this indicator.
There is no need to self-medicate; only a specialist can accurately determine the cause of the increase in hematocrit and prescribe the correct diagnosis and treatment. Therefore, if there are any changes in the blood test, you should consult a specialist and strictly follow the recommendations received.
Decreased hematocrit
A decreased hematocrit occurs when the number of red blood cells or their size decreases - erythrocytopenia. The cause may also be the accumulation of water in the body when the blood becomes thinner - hyperhydration, as well as hyperproteinemia or the accumulation of proteins in the plasma, which contributes to fluid retention.
Causes
A decrease in hematocrit is facilitated by prolonged immobility, fasting or a strict diet, taking anticoagulants and antiplatelet agents, and intravenous infusions in large volumes; heavy drinking, chronic alcoholism, excessive salt intake, menstruation in women.
Also, a downward change in the indicator may indicate the following pathologies:
- iron-, B12- or folate-deficiency anemia;
- severe bleeding;
- impaired hemoglobin production in sickle cell anemia;
- fibrous degeneration of the liver - cirrhosis;
- disruption of the urinary system;
- hemolysis of erythrocytes - destruction of red blood cells due to hereditary mutation, autoimmune processes or toxic effects on blood cells;
- malaria, typhoid fever;
- oncological diseases of the bone marrow or its metastatic lesions from other organs;
- an increase in the amount of protein in plasma due to vomiting, diarrhea, blood cancer and other conditions.
During pregnancy, a decrease in hematocrit can be observed in the case of toxicosis, a very young age of the mother, multiple pregnancies, a short period of time between pregnancies, and also after the 20th week of gestation due to a physiological increase in fluid in the body.
Symptoms
A decrease in hematocrit in the blood is accompanied by hypoxia of various organs, since it is the red blood cells that normally carry oxygen throughout the body. This condition is manifested by the following symptoms:
- fast fatiguability;
- general weakness;
- drowsiness;
- increased heart rate and breathing;
- feeling of lack of air;
- headache, dizziness;
- decreased memory and concentration;
- hair loss;
- marbling or pallor of the skin.
Reasons for increasing hematocrit
Dehydration (dehydration). Loss of fluid due to repeated vomiting and/or diarrhea, sunstroke, burn disease, pathology of the digestive tract, intestinal obstruction, hyperhidrosis (excessive sweating), peritonitis leads to blood thickening due to an unchanged number of red blood cells.
Hypoxia. People suffering from diabetes, smokers, people located high in the mountains or in unventilated areas experience a lack of oxygen, which leads to the release of red blood cells into the bloodstream.
Cardiovascular pathology. Heart defects, coronary disease, and cardiovascular failure are accompanied by a lack of oxygen in the blood.
Bronchopulmonary pathology. Chronic hypoxia leads to: bronchial asthma, emphysema, obstructive bronchitis and other pulmonary diseases.
Neoplasms in the kidneys. Any kidney tumor provokes increased production of erythropoietin, which increases the formation of red blood cells.
Erythrocytosis. The pathology is characterized by increased production of red cells (true erythrocytosis) or redistribution of formed blood elements in some diseases (redistribution).
Erythremia. Refers to true erythrocytosis, synonymous with Vaquez-Osler disease. It is one of the variants of chronic leukemia.
Leukemia. Accompanied by an increase in white blood cells and a decrease in its liquid part.