Pyelonephritis
Diabetes
Hepatitis
Rheumatism
52845 October 27
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. We remind you that independent interpretation of the results is unacceptable; the information below is for reference only.
Urea in the blood: indications for prescription, rules for preparing for the test, interpretation of the results and normal indicators.
What is urea
Urea is a product that is formed in the liver as a result of the synthesis of ammonia and carbon dioxide. The resulting compound is delivered by blood to the kidneys, where the filtering organ separates it from the general bloodstream and sends it into the urine.
Urea is a product unnecessary by the body, which must be completely eliminated, since its accumulation gives an osmotic effect, which can cause swelling of the internal organs in which it accumulates:
- liver;
- kidney;
- thyroid gland;
- spleen;
- pancreas.
Normally, the final product - urea - should be excreted from the body, but if there are any abnormalities in the functioning of the system, it is detected in the blood.
What does urea in the blood mean?
Based on the state of the blood, namely the presence of high concentrations of urea in it, one can judge:
- the functioning of the kidneys, which are required to remove waste substances;
- about the function of the liver, which synthesizes urea from ammonia;
- about the health of muscle tissue, since the breakdown of protein in the muscles also produces urea.
Indications for testing may include:
- cardiac ischemia;
- rheumatoid arthritis;
- systemic scleroderma;
- liver diseases;
- screening results that do not fit within the normal range;
- suspected kidney infections;
- preparation for drug therapy;
- studies before hospitalization;
- assessment of the dialysis procedure performed.
Most often, an increase in urea indicates chronic or acute kidney disease. Separately, a comparative analysis is carried out for the urea content in urine and blood. If the level of the substance in the urine is lower than what is found in the blood, they speak of a disease of the filtration system - renal failure.
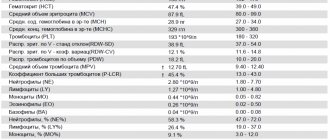
Blood test indicator table
Decoding a biochemical blood test is a comparison of the results obtained with normal values. The analysis form contains a complete list of indicators determined by the biochemical laboratory and their reference values.
The norms for biochemical blood test indicators in adults are shown in the table:
| Analysis: | Men: | Women: |
| Total protein | 64-84 g/l. | 64-84 g/l. |
| Hemoglobin | 130-160 g/l | 120-150 g/l. |
| Haptoglobin | 150-2000 mg/l | 150-2000 mg/l |
| Glucose | 3.30-5.50 mmol/l. | 3.30-5.50 mmol/l. |
| Urea | 2.5-8.3 mmol/l. | 2.5-8.3 mmol/l. |
| Creatinine | 62-115 µmol/l | 53-97 µmol/l. |
| Cholesterol | 3.5-6.5 mmol/l. | 3.5-6.5 mmol/l. |
| Bilirubin | 5-20 µmol/l. | 5-20 µmol/l. |
| AlAT (ALT) | up to 45 units/l. | up to 31 units/l. |
| ASAT (AST) | up to 45 units/l. | up to 31 units/l. |
| Lipase | 0-190 units/l. | 0-190 units/l. |
| Alpha amylase | 28-100 units/l. | 28-100 units/l. |
| Pancreatic amylase | 0-50 units/l. | 0-50 units/l. |
Each of the criteria indicated in the table reflects the condition of one or more human organs. And a combination of some of them sometimes makes it possible to make an accurate diagnosis or direct the diagnostic process in the right direction.
Sometimes it is enough to establish a final diagnosis based on deviations from the norm of one or more parameters. But much more often, a full diagnosis requires other results of additional research methods and an assessment of the clinical picture of the disease.
Total protein
Total protein is the total concentration of proteins found in the blood. Proteins take part in all biochemical reactions of the body - they transport various substances, act as catalysts for reactions, and participate in immune defense.
Normal levels of protein in the blood are 64-84 g/l. If the protein is higher than this, the body may be susceptible to infection. In addition, the cause of increased protein may be arthritis, rheumatism, or the onset of cancer. With a low protein content in the blood, the likelihood of liver disease increases many times, as well as problems with the intestines and kidneys. The most difficult diagnosis for low protein is cancer.
Albumen
This protein is produced by the liver and is considered the main protein in the blood plasma. In general, experts distinguish albumins as a separate protein group, called protein fractions.
An increase in the concentration of albumin in the blood (hyperalbuminemia) may be associated with the following pathologies:
- dehydration, or dehydration (loss of fluid from the body through vomiting, diarrhea, profuse sweating);
- extensive burns.
A reduced albumin level is observed in smoking patients and in women during pregnancy and breastfeeding. In other people, a decrease in albumin may indicate various liver pathologies (for example, cirrhosis, hepatitis, or oncology), or intestinal inflammation of an infectious nature (sepsis). In addition, in case of heart failure or cancer, burns or fever, various injuries or drug overdose, the albumin in the blood will be lower than normal.
Glucose (sugar)
The most common indicator of carbohydrate metabolism is blood sugar. Its short-term increase occurs during emotional arousal, stress reactions, pain attacks, and after eating. The norm is 3.5-5.5 mmol/l (glucose tolerance test, sugar load test).
Sugar is elevated - diabetes, endocrine disorders, pancreatitis, pancreatic tumor, cerebral hemorrhage, chronic liver and kidney damage, myocardial infarction, cystic fibrosis.
Sugar is low - damage to the liver and pancreas, hypothyroidism, stomach or adrenal cancer, arsenic poisoning or certain medications, alcohol intoxication.
Uric acid
The main breakdown product of the main component of nucleic acids - purine bases. Since it is not used further in metabolic processes, it is excreted unchanged by the kidneys. The normal level in blood plasma is 0.16-0.44 mmol/l.
An increase in uric acid levels in the blood indicates:
- renal failure;
- leukemia, lymphoma;
- prolonged fasting;
- alcohol abuse;
- overdose of salicylates and diuretics.
A decrease in the level of uric acid in the blood can be observed during treatment with piperazine drugs, allopurinol, prebenecid, ACTH, sometimes with hepatitis, anemia.
Urea
It is a consequence of the breakdown of proteins. The permissible amount of this substance in a person’s blood changes with age. Often, the level of urea goes through the roof in patients who have pathologies in their kidneys: doctors prescribe a similar blood test to diagnose and predict the disease.
A decrease in the level of urea in the blood can be triggered by reasons that are physiological (pregnancy, fasting, excessive exercise), or pathological (celiac disease, cirrhosis of the liver, heavy metal poisoning).
Creatinine
This substance, like urea, is a product of protein metabolism and is also excreted by the kidneys. Creatinine is a product of metabolic processes occurring in skeletal muscles, and to a lesser extent in the brain. Accordingly, its level will depend on the condition of the kidneys and muscles.
Increased creatinine is observed in renal failure, severe injuries with muscle damage, increased thyroid function, and after the use of certain anti-inflammatory and antibacterial agents. Moderately high creatinine is found in athletes.
Alanine aminotransferase (ALT, AlAt)
This indicator, along with AST, is used in medical practice for laboratory diagnosis of liver damage. Alanine aminotransferase is synthesized intracellularly, and normally only a small part of this enzyme enters the blood. When the liver is damaged (hepatitis, cirrhosis) as a result of cytolysis (cell destruction), this enzyme enters the blood, which is detected by laboratory methods.
The level of this transaminase may also increase during myocardial infarction and other conditions. An increase in ALT that exceeds an increase in AST is characteristic of liver damage; if the AST indicator increases more than the ALT increases, then this, as a rule, indicates problems with myocardial (heart muscle) cells.
Aspartate aminotransferase (AST, AST)
A cellular enzyme involved in amino acid metabolism. AST is found in the tissues of the heart, liver, kidneys, nervous tissue, skeletal muscles and other organs. An AST blood test may show an increase in AST in the blood if the body has a disease such as:
- myocardial infarction;
- viral, toxic, alcoholic hepatitis;
- angina pectoris;
- acute pancreatitis;
- liver cancer;
- acute rheumatic carditis;
- heavy physical activity;
- heart failure.
AST is elevated in skeletal muscle injuries, burns, heat stroke, and as a result of cardiac surgery.
Alkaline phosphatase
Many laboratories automatically include this enzyme in their biochemical analysis. From a practical point of view, only an increase in the activity of this enzyme in the blood may be of interest.
This is evidence of either intrahepatic stagnation of bile in the small bile ducts, which occurs with mechanical and parenchymal jaundice, or progressive osteoporosis or destruction of bone tissue (myeloma, aging of the body).
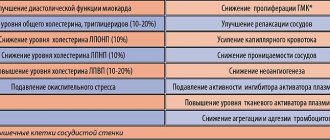
Cholesterol
A component of fat metabolism, it is involved in the construction of cell membranes, the synthesis of sex hormones and vitamin D. There is total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
Degrees of increased cholesterol in the blood:
- 5.2-6.5 mmol/l – mild degree of increase in the substance, a risk zone for atherosclerosis;
- 6.5-8.0 mmol/l – a moderate increase, which is corrected by diet;
- over 8.0 mmol/l – a high level requiring drug intervention.
An increase in cholesterol levels in the serum or blood plasma is an argument in favor of atherosclerosis, hypothyroidism (low activity of the thyroid gland), chronic hepatitis, decompensated diabetes mellitus, obstructive jaundice.
This indicator decreases when:
- malignant liver tumors;
- cirrhosis of the liver;
- rheumatoid arthritis;
- hyperfunction of the thyroid and parathyroid glands;
- starvation;
- malabsorption of substances;
- chronic obstructive pulmonary diseases.
Bilirubin
Bilirubin is a yellow-red pigment that is formed when hemoglobin breaks down in the spleen, liver and bone marrow. Its normal level in the blood of children and adults is 3.4–20.5 µmol/l.
If the table with the examination results contains an elevated level of bilirubin, then the doctor can diagnose one of the following diseases in adults:
- cholelithiasis;
- pancreatic tumors;
- inflammatory diseases of the biliary tract.
If bilirubin is below normal, then the patient may have one of the following diseases:
- acute viral hepatitis;
- bacterial liver damage (leptospirosis, brucellosis, etc.);
- toxic hepatitis;
- medicinal product;
- neoplasms in the liver and primary biliary cirrhosis;
- hemolytic anemia of various etiologies.
Bilirubin, formed as a result of the breakdown of hemoglobin (indirect), is released into the blood, where it binds to albumin and is transported to the liver. In liver cells, bilirubin combines with glucuronic acid. This bilirubin bound to glucuronic acid is called direct bilirubin.
Amylase
Breaks down carbohydrates from food and ensures their digestion. Contained in the salivary glands and pancreas. There is alpha-amylysis (diastase) and pancreatic amylase.
- alpha-amylase rate: 28-100 units/l.
- pancreatic amylase rate: 0-50 units/l.
A high amylase content in a biochemical blood test indicates: peritonitis, pancreatitis, diabetes mellitus, pancreatic cyst, stone, cholecystitis or renal failure.
Decreased alpha-amylase: thyrotoxicosis; myocardial infarction; complete necrosis of the pancreas; toxicosis of pregnant women.
Potassium
Another important intracellular electrolyte. Its normal content in the body ranges from 3.5 to 5.5 mmol per liter.
Reduced potassium content:
- excess hormones of the adrenal cortex (including taking dosage forms of cortisone);
- chronic fasting (failure to receive potassium from food);
- prolonged vomiting, diarrhea (loss with intestinal juice);
- renal dysfunction;
- cystic fibrosis.
Increased potassium content:
- dehydration;
- acute renal failure (impaired renal excretion); ,
- adrenal insufficiency.
- cell damage (hemolysis - destruction of blood cells, severe starvation, convulsions, severe injuries).
The condition when potassium is elevated is called hyperkalemia, and when it is low, hypokalemia.
Sodium
Sodium does not directly participate in metabolism. It is completely abundant in the extracellular fluid. Its main function is to maintain osmotic pressure and pH. Sodium excretion occurs in the urine and is controlled by the adrenal hormone aldosterone.
Sodium reduction:
- decreased concentration due to increased fluid volume (diabetes mellitus, chronic heart disease)
- failure, liver cirrhosis, nephrotic syndrome, edema).
- loss of an element (abuse of diuretics, kidney pathology, adrenal insufficiency).
Increased sodium content:
- increased function of the adrenal cortex;
- excess salt intake;
- loss of extracellular fluid (profuse sweat, severe vomiting and diarrhea, increased urination in diabetes insipidus);
- violation of the central regulation of water-salt metabolism (pathology of the hypothalamus, coma).
An increase in a microelement is called hypernatremia, and a decrease is called hyponatremia.
Why might urea be elevated?
To determine the level of urea in the blood, a laboratory method called a biochemical blood test is used. It involves taking material from a vein. For each age category of patients there is its own norm for urea content in the blood:
- in newborns from 1.7 to 5;
- in children of the first year of life from 1.4 to 5.4;
- from one to 15 years old can have 1.8-6.7;
- women over 18 years old - from 2 to 6.7;
- men over 18 years old - from 2.8 to 8.
Several factors influence the urea content. One of which is the level of amino acids in the body, since ammonia is formed from them during metabolism, which becomes one of the components of urea. On the other hand, with a sufficient amount of amino acids, the diseased liver will not be able to synthesize urea, which will be the reason for the detection of its negligible amount. The third important factor is the performance of the kidneys, which must, by filtering the blood, extract urea from it and send it out of the body with urine.
If we exclude all possible pathologies, then we can say that the following factors not related to the disease can increase the level of urea in the blood:
- on the eve of the collection of material, severe emotional stress was experienced;
- the patient had to buy and take a drug from the list: Tetracycline, Euthyrox, Neomycin, Lasix, any drug from the group of corticosteroids or sulfonamides, anabolic steroids, steroids, salicylates;
- the patient fasted for a long time or, on the contrary, ate a lot of protein foods;
- the patient on the eve of the delivery of the material or daily subjected the body to heavy physical activity.
When a doctor tries to determine the quality of kidney function, the presence of urea in the blood may indicate:
- blockage of the urinary ducts;
- chronic. renal failure;
- glomerulonephritis;
- pyelonephritis;
- dehydration, which could be preceded by myocardial infarction, shock or heart failure.
Separately, we should highlight the reasons why urea is formed in the human body in huge quantities:
- prostate neoplasms;
- burn disease;
- severe intestinal infections;
- hematological diseases;
- state of shock.
To accurately determine the patient’s condition, it is necessary to conduct several laboratory tests in a row to see the picture in dynamics; in addition, it is necessary to measure the amount of urea in the urine in order to be able to compare this indicator with blood data.
What do the results mean?
Normal urea values
in blood serum: from 17 to 43 mg/dl or 2.8-7.1 mmol/l.
Increased values:
- acute and chronic renal failure;
- decreased renal perfusion due to heart failure, hypovolemic shock, severe hypotension;
- obstruction of the urinary tract;
- dehydration due to decreased fluid intake, excessive fluid loss - sweating, vomiting, diarrhea, diuretics, etc.;
- gastrointestinal bleeding;
- catabolic state: trauma, severe infection, fasting, some drugs with a catabolic effect, such as corticosteroids;
- high protein diet;
- aging.
Reduced values:
- liver disease;
- low protein and high carbohydrate diet;
- parenteral nutrition is intravenous nutrition through a catheter inserted into a vein;
- low protein diet;
- overhydration;
- pregnancy;
- advanced liver disease – cirrhosis, liver failure;
- inherited defect of the enzymes of the “urea cycle” - decreased synthesis of urea.
Symptoms indicating increased urea
Based on his feelings, the patient himself can often tell that the level of urea in the blood may be elevated. This is primarily indicated by pain in the lower back in both men and women. It indicates kidney disease.
Separately distinguished:
- swelling;
- increased amount of urine produced;
- scanty urine production;
- the presence of protein in the urine.
However, indications for donating blood for urea may be:
- ischemic diseases;
- hepatitis;
- cirrhosis;
- decreased absorption of foods;
- connective tissue diseases.
The level of urea indicates several possible pathologies at once, so this analysis is often used to monitor the patient’s condition.
How to take a urea test correctly
You need to prepare for the analysis so as not to receive distorted data. First of all, you need to remember that blood is donated strictly on an empty stomach. In addition, since urea production is affected by the breakdown of muscle fibers, it is important to avoid physical activity on the eve of the test. If you can’t get to the laboratory without excessive physical activity, you need to arrive at the door of the office no later than half an hour before the appointed time in order to have time to calm down and put your nervous system in order.
If the patient is taking any medications, it is better to postpone the morning dose until the blood has already been donated. Immediately before the donation, you should not do massages, biopsies, or x-rays, especially those using contrast.
How can you reduce urea levels?
To reduce urea levels:
- avoid heavy physical activity;
- Avoid taking supplements containing creatine;
- eat less protein;
- drink more water;
- follow a diet - eat less meat and poultry, but more fish, nuts, vegetables and fruits, cereals, olive oil.
- limit your salt intake;
- Reduce your intake of bad fats – saturated and trans fats – found in processed meats, cakes, biscuits and pastries;
- Avoid obesity and lead an active lifestyle.
Herbal remedies to reduce urea levels:
- Punarnava or burhaavia spreading
from the umbrella family. This herb helps get rid of excess fluid in the kidneys, reducing swelling without any side effects. - Prickly capers
are from the caper family. Preparations from this plant are used to break up kidney stones and as a cure for urinary tract infections. This herb helps remove elements blocking the urinary tract, removes excess fluid - Gokshura or Nerinjil or devil's weed is native to India. This is a diuretic. It is also used as an herbal tonic to restore kidney cells.