Latran, 2 mg/ml, solution for intravenous and intramuscular administration, 2 ml, 5 pcs.
INSTRUCTIONS for using LATRANUM
APPROVED:
Pharmacological State Committee of the Ministry of Health of the Russian Federation on March 23, 2000 in return
instructions approved on April 11, July 6, 1995, March 28, 1996, 29
July 1998
Latran (ondansetron) - 9-methyl-3-(2-methyl-1H-imidazol-1-ylmethyl)-1,2,3,9-tetrahydrocarbazole-4
(H)-one hydrochloride dihydrate - white or off-white
crystalline powder. In medical practice it is used in the form of an injection solution and tablets.
Pharmacological properties
Latran is an antiemetic from the group of serotonin antagonists. Pharmacodynamics.
Selectively blocks 5-HT3 receptors of the central and peripheral nervous system, incl. in the neural centers that regulate the implementation of gag reflexes. The drug has anxiolytic activity and does not cause sedation, impaired coordination of movements or decreased activity and performance. Eliminates somatic and psychopathological symptoms of mild to moderate alcohol withdrawal syndrome.
Indications for use
Nausea and vomiting caused by X-ray or chemotherapy
antitumor drugs or exposure to ionizing radiation.
Prevention and treatment of vomiting in the postoperative period. Symptomatic
treatment of alcohol withdrawal syndrome (especially mild and moderate
degree of severity).
Directions for use and doses
Latran solution 0.2% for injection is administered intravenously, Latran tablets are taken orally. For adults, Latran solution 0.2% is first administered once intravenously at a dose of 0.008–0.016 g over 15 minutes immediately before chemotherapy. After 2 hours, start taking Latran tablets orally in a single dose of 0.008 g every 8 hours, but not more than 5 days. For children over 4 years of age, Latran solution 0.2% is administered once intravenously for 15 minutes immediately before chemotherapy at a dose determined at the rate of 0.005 g of the drug per 1 m2 of the child’s body surface, after which Latran tablets are taken orally at 0.004 g every 8 h, but not more than 5 days. When exposed to ionizing radiation, the drug is taken orally in a single dose of 0.008 g (2 tablets) 1 hour before or immediately after radiation exposure. For the symptomatic treatment of alcohol withdrawal syndrome, a dose of 0.008 g is administered intravenously in the form of a 0.2% solution in 400 ml of hemodez, chlosol or saline. If necessary, re-administration of the drug Latran is possible.
Contraindications
Hypersensitivity, pregnancy, breastfeeding period.
Side effect
From the side of the central nervous system:
headache; rarely - transient visual disturbances and dizziness (with rapid intravenous administration), involuntary movements.
From the cardiovascular system:
chest pain, arrhythmias, bradycardia, arterial hypotension.
From the digestive system:
constipation, diarrhea, transient increase in serum transaminases.
Allergic reactions:
rarely - bronchospasm, angioedema, urticaria; in some cases - anaphylactic reactions.
Other:
urinary retention, feeling of warmth and rush of blood to the head and epigastric region.
special instructions
When used in patients with moderate and severe liver dysfunction, it is not recommended to exceed a dose of 8 mg/day.
Interaction with other drugs
Due to the fact that ondansetron is metabolized in the liver by enzymes of the cytochrome P450 system, it is possible that when used simultaneously with drugs that are inducers or inhibitors of this enzyme system, Cl and T1/2 of ondansetron change.
Release form
Solution 0.2% for injection in ampoules of 2 ml or 4 ml, 5 ampoules per box; tablets of 0.004 g, film-coated, 10 pcs. in blister packs, 1 pack in a box, or in jars of 60 or 100 pcs., or in jars of 0.5 kg.
Storage conditions
Ampoules with solution - in a place protected from light. Tablets - in a dry place, protected from light. List B.
Best before date
3 years.
Dispensed by prescription.
Manufacturer - State Enterprise SPC "Pharmzashchita", 141400, Khimki, Moscow region, Vashutinskoe highway, 11
Nosological classification (ICD-10)
- F10.3 Withdrawal state
- K21 Gastroesophageal reflux
- K21.0 Gastroesophageal reflux with esophagitis
- K25 Stomach ulcer
- K26 Duodenal ulcer
- K29.1 Other acute gastritis
- K29.5 Chronic gastritis, unspecified
- K91.3 Postoperative intestinal obstruction
- K94* Diagnosis of gastrointestinal diseases
- R11 Nausea and vomiting
- T51 Toxic effects of alcohol
- T90.5 Consequences of intracranial injury
- Z100* CLASS XXII Surgical practice
- Z51.0 Radiotherapy course
- Z51.1 Chemotherapy for neoplasm
- Z54 Convalescent period
- Z58.4 Exposure to radiation pollution
Indications for use of the drug Latren
Peripheral circulatory disorders, intermittent claudication, diabetic neuropathy, obliterating endarteritis, Raynaud's syndrome and disease. Violation of tissue trophism, post-thrombotic syndrome, varicose veins, trophic ulcers of the lower leg, gangrene, frostbite. Cerebrovascular accident, ischemic stroke. Cerebral atherosclerosis: dizziness, headache, memory impairment, sleep disturbance. Encephalopathy. Poor circulation in the retina and choroid of the eye. Degenerative changes against the background of vascular pathology of the inner ear with gradual deterioration of hearing.
Pharmacokinetics
With intramuscular administration, Cmax in plasma is achieved within 10 minutes; after oral administration - after about 1.5 hours. The distribution of ondansetron is the same with oral, intramuscular and intravenous administration. Absolute bioavailability is about 60%. Plasma protein binding is 70–76%. Metabolized in the liver. Less than 5% of the drug is excreted unchanged in the urine. Both after oral administration and with parenteral administration, T1/2 is about 3 hours, in elderly patients it can reach 5 hours, and with severe liver failure - 15–32 hours. With kidney damage (Cl creatinine <15 ml/min) T1 /2 increases by 4–5 hours, but this increase is not clinically significant.
special instructions
Hypersensitivity reactions when using Latran® may occur in patients previously observed for similar reactions when using other selective 5-HT3 receptor antagonists.
Patients with signs of intestinal obstruction after using the drug require regular monitoring, because ondansetron may cause constipation.
The infusion solution must be prepared immediately before use. If necessary, the prepared infusion solution can be stored until use for a maximum of 24 hours at a temperature of 2–8 °C.
No protection from light is required during the infusion: the diluted injection solution remains stable for at least 24 hours in natural light or normal lighting.
Directions for use and doses
IV, IM, inside.
Cytostatic therapy: the choice of dosage regimen is determined by the emetogenicity of antitumor therapy. For adults, the daily dose is usually 8–32 mg, the following regimens are recommended:
With moderate emetogenic chemotherapy or radiotherapy
- 8 mg IV in a slow stream or IM immediately before starting therapy;
- 8 mg orally (2 tablets) 1–2 hours before the start of therapy, then another 8 mg (2 tablets) 12 hours after the start of therapy.
With highly emetogenic chemotherapy
- 8 mg IV infusion slowly immediately before the start of chemotherapy, and then 2 more IV injections of 8 mg each with an interval of 2-4 hours;
- continuous 24-hour infusion at a dose of 24 mg at a rate of 1 mg/h;
- 16–32 mg, diluted in 50–100 ml of the appropriate infusion solution, as a 15-minute infusion immediately before the start of chemotherapy.
The effectiveness of Latran® can be increased by a single intravenous administration of a glucocorticoid (for example, 20 mg of dexamethasone) before starting chemotherapy.
To prevent delayed vomiting that occurs after the first 24 hours from the start of chemotherapy, it is recommended to continue taking the drug orally in tablet form, 8 mg 2 times a day for 5 days.
For children over 2 years of age, the drug is prescribed at a dose of 5 mg/m2 IV immediately before the start of chemotherapy, followed by oral administration at a dose of 4 mg after 12 hours; after completion of chemotherapy, it is recommended to continue treatment at a dose of 4 mg orally 2 times a day for 5 days.
Prevention of postoperative nausea and vomiting: adults are given a single dose of 8 mg IM or IV in a slow stream at the beginning of anesthesia, or 16 mg is prescribed orally 1 hour before the start of anesthesia. To relieve nausea and vomiting, it is recommended to administer 8 mg of the drug intramuscularly or slowly intravenously. Latran® can be administered intramuscularly into the same area of the body in a dose not exceeding 8 mg.
For children, to prevent postoperative nausea and vomiting, Latran® is used exclusively parenterally in a single dose of 0.1 mg/kg (maximum 4 mg) as a slow intravenous injection before or after anesthesia. For the treatment of developed postoperative nausea and vomiting in children, slow intravenous administration of a single dose of 0.1 mg/kg (maximum up to 4 mg) is recommended. In Russia there is not enough experience in using the drug to prevent and treat postoperative nausea and vomiting in children under 2 years of age.
When exposed to ionizing radiation, Latran® is taken orally in a single dose of 8 mg (2 tablets) 1 hour before or immediately after radiation exposure.
For the symptomatic treatment of alcohol withdrawal syndrome, the drug is administered intravenously in a dose of 8 mg (in the form of a solution of 2 mg/ml, 4 ml) in 400 ml of hemodez, chlorsol or saline solution. If necessary, the drug can be re-administered.
Elderly patients do not need to change the dosage.
Patients with kidney damage do not need to change the usual daily dose or frequency of administration of the drug.
If there is liver damage, the dose should be reduced to 8 mg per day.
The following solutions can be used to dilute the injection solution: 0.9% sodium chloride solution; 5% glucose solution; Ringer's solution; 0.3% potassium chloride solution and 0.9% sodium chloride solution; 0.3% potassium chloride solution and 5% glucose solution.
Composition and release form
| Solution for intravenous and intramuscular administration | 1 ml |
| ondansetron hydrochloride dihydrate (based on base) | 2 mg |
| excipients: sodium chloride; hydrochloric acid; water for injections |
in ampoules of 2 or 4 ml; in a cardboard pack 1; 2 or 5 pcs.
| Film-coated tablets | 1 table |
| ondansetron hydrochloride dihydrate (based on base) | 4 mg |
| excipients: MCC; colloidal silicon dioxide (Aerosil); potato starch; magnesium stearate shell composition: hydroxypropylcellulose; Tween 80 (polysorbate); tropeolin O; castor oil |
in a blister pack 10 pcs.; in a cardboard pack 1 package, or in dark glass jars of 0.4 (4000) and 0.8 kg (8000 pcs.).
Interaction
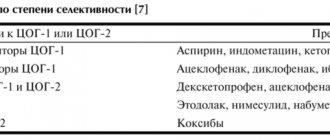
Since ondansetron is metabolized by the liver enzyme system (cytochrome P450), caution is required when used together:
- with P450 enzymatic inducers (CYP2D6 and CYP3A) (barbiturates, carbamazepine, carisoprodol, glutethimide, griseofulvin, nitrous oxide, papaverine, phenylbutazone, phenytoin and probably other hydantoins, rifampicin, tolbutamide);
- with inhibitors of P450 enzymes (CYP2D6 and CYP3A) (allopurinol, macrolide antibiotics, antidepressants - MAO inhibitors, chloramphenicol, cimetidine, estrogen-containing oral contraceptives, diltiazem, disulfiram, erythromycin, valproic acid, sodium valproate, fluconazole, fluoroquinolones, isoniazid, ket okonazole, lovastatin , metronidazole, omeprazole, propranolol, quinidine, quinine, verapamil).
Side effects
From the nervous system: headache, dizziness, spontaneous movement disorders and convulsions.
From the cardiovascular system: chest pain, in some cases with ST segment depression, bradycardia, arrhythmias, arterial hypotension.
From the gastrointestinal tract: hiccups, dry mouth, diarrhea, constipation, sometimes asymptomatic transient increases in the level of aminotransferases in the blood serum.
Allergic reactions: urticaria, bronchospasm, laryngospasm, angioedema, anaphylaxis.
Other: local reactions (pain, burning and redness at the injection site), flushing of the face, feeling of heat, temporary impairment of visual acuity, hypokalemia.
Pharmacological properties of the drug Latren
The active component of the drug is pentoxifylline, a peripheral vasodilator from the purine group. Improves microcirculation and rheological properties of blood, inhibits phosphodiesterase, increases the content of cyclic 3,5-AMP in vascular smooth muscle cells and platelets. It increases the ATP content in red blood cells while simultaneously saturating the energy potential, which in turn leads to vasodilation, a decrease in peripheral resistance, an increase in systolic and cardiac output without a significant change in heart rate. The drug relaxes the smooth muscles of the coronary arteries, increases the delivery of oxygen to the myocardium, which determines the antianginal effect of the drug. By expanding the blood vessels of the lungs, Latren improves blood oxygenation, increases the tone of the respiratory muscles (intercostal muscles and diaphragm), leads to increased collateral circulation, and an increase in the volume of inflowing blood. The drug leads to an increase in the ATP content in brain cells and has a beneficial effect on the bioelectrical activity of the central nervous system. Reduces blood viscosity, causes platelet disaggregation, increases the elasticity of red blood cells by affecting the properties of their membrane. Improves blood microcirculation in areas of impaired blood supply. In case of occlusive lesions of the peripheral arteries (intermittent claudication), pentoxifylline leads to an increase in walking distance, elimination of night cramps of the calf muscles and pain at rest. The drug is almost completely metabolized with the formation of 5 metabolites, of which (M-I) - hydroxypenioxyphylline is the main one. Others (M-GU) and (M-U) are formed due to the oxidation of (M-I) and have the same pharmacological activity as the original substance. More than 90% is excreted by the kidneys, regardless of the route of administration, in the form of unconjugated water-soluble polar metabolites. The half-life of the active substance and its metabolites is 0.5–1.5 hours. If liver and kidney function are impaired, the half-life increases.