A general blood test is one of the routine tests of any clinical laboratory - this is the first test that a person takes when undergoing medical examination or when he becomes ill. In laboratory work, CBC is classified as a general clinical research method (clinical blood test).
Even people far from all laboratory wisdom, replete with a mass of difficult-to-pronounce terms, had a good grasp of the norms, meanings, names and other parameters as long as the answer form included leukocyte cells (leukocyte formula), red blood cells and hemoglobin with a color indicator. The widespread population of medical institutions with all kinds of equipment did not spare the laboratory service either; many experienced patients found themselves at a dead end: some incomprehensible abbreviation of Latin letters, a lot of all sorts of numbers, different characteristics of red blood cells and platelets...
Do-it-yourself decryption
The difficulty for patients is a general blood test performed by an automatic analyzer and scrupulously copied into a form by the responsible laboratory assistant. By the way, the “gold standard” of clinical research (microscope and doctor’s eyes) has not been canceled, therefore any analysis performed for diagnosis must be applied to glass, stained and examined in order to identify morphological changes in blood cells. In the event of a significant decrease or increase in a certain population of cells, the device may not be able to cope and “protest” (refuse to work), no matter how good it is.
Sometimes people try to find differences between a general and clinical blood test, but there is no need to look for them, because a clinical analysis implies the same study, which for convenience is called a general test (it’s shorter and clearer), but the essence does not change.
A general (detailed) blood test includes:
- Determination of the content of cellular elements of blood: erythrocytes - red blood cells containing the pigment hemoglobin, which determines the color of blood, and leukocytes, which do not contain this pigment, therefore are called white blood cells (neutrophils, eosinophils, basophils, lymphocytes, monocytes);
- Hemoglobin level;
- Hematocrit (in a hematology analyzer, although it can be approximately determined by eye after the red blood cells spontaneously settle to the bottom);
- Color index calculated according to the formula, if the study was carried out manually, without the participation of laboratory equipment;
- Erythrocyte sedimentation rate (ESR), formerly called reaction rate (ERR).
A general blood test shows the reaction of this valuable biological fluid to any processes occurring in the body. How many red blood cells and hemoglobin it contains, which perform the function of respiration (transferring oxygen to tissues and removing carbon dioxide from them), leukocytes that protect the body from infection, platelets involved in the coagulation process, how the body reacts to pathological processes, in a word, the CBC reflects the condition the organism itself at different periods of life. The concept of “complete blood count” means that, in addition to the main indicators (leukocytes, hemoglobin, red blood cells), the leukocyte formula (granulocytes and cells of the agranulocyte series) is studied in detail.
It is better to entrust the interpretation of the blood test to the doctor, but if there is a special desire, the patient can try to independently study the result issued in the clinical laboratory, and we will help him with this by combining the usual names with the abbreviation of the automatic analyzer.
How to determine a person's blood volume?
For this purpose, a certain amount of a contrast agent, usually a harmless dye, is injected into the blood. After it is distributed throughout the riverbed, a fence is made to determine its concentration.
Another way is to inject radioactive isotopes and count the number of red blood cells that contain them. The amount of blood is determined by the level of its radioactivity.
Blood transfusion is used to normalize blood volume in the body.
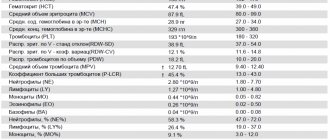
The table is easier to understand
As a rule, the results of the study are recorded on a special form, which is sent to the doctor or given to the patient. To make it easier to navigate, let’s try to present a detailed analysis in the form of a table in which we will enter the norm of blood parameters. The reader will also see in the table such cells as reticulocytes. They are not among the mandatory indicators of a general blood test and are young forms of red blood cells, that is, they are the precursors of red blood cells. Reticulocytes are examined to identify the cause of anemia. There are very few of them in the peripheral blood of an adult healthy person (the norm is shown in the table); in newborn children there can be 10 times more of these cells.
| No. | Indicators | Norm |
| 1 | Red blood cells (RBC), 10 cells to the 12th power per liter of blood (1012/L, tera/liter) men women | 4,4 — 5,0 3,8 — 4,5 |
| 2 | Hemoglobin (HBG, Hb), grams per liter of blood (g/l) men women | 130 — 160 120 — 140 |
| 3 | Hematocrit (HCT), % men women | 39 — 49 35 — 45 |
| 4 | Color Index (CPU) | 0,8 — 1,0 |
| 5 | Average erythrocyte volume (MCV), femtoliter (fl) | 80 — 100 |
| 6 | Average hemoglobin content in an erythrocyte (MCH), picograms (pg) | 26 — 34 |
| 7 | Mean erythrocyte hemoglobin concentration (MCHC), grams per deciliter (g/dL) | 3,0 — 37,0 |
| 8 | Anisocytosis of erythrocytes (RDW), % | 11,5 — 14,5 |
| 9 | Reticulocytes (RET) % ‰ | 0,2 — 1,2 2,0 — 12,0 |
| 10 | White blood cells (WBC), 10 cells to the 9th power per liter of blood (109/l, giga/liter) | 4,0 — 9,0 |
| 11 | Basophils (BASO), % | 0 — 1 |
| 12 | Basophils (BASO), 109/l (absolute values) | 0 — 0,065 |
| 13 | Eosinophils (EO), % | 0,5 — 5 |
| 14 | Eosinophils (EO), 109/l | 0,02 — 0,3 |
| 15 | Neutrophils (NEUT), % myelocytes, % young, % band neutrophils, % in absolute values, 109/l segmented neutrophils, % in absolute values, 109/l | 47 — 72 0 0 1 — 6 0,04 — 0,3 47 – 67 2,0 – 5,5 |
| 16 | Lymphocytes (LYM), % | 19 — 37 |
| 17 | Lymphocytes (LYM), 109/l | 1,2 — 3,0 |
| 18 | Monocytes (MON), % | 3 — 11 |
| 19 | Monocytes (MON), 109/l | 0,09 — 0,6 |
| 20 | Platelets (PLT), 109/l | 180,0 — 320,0 |
| 21 | Average platelet volume (MPV), fl or µm3 | 7 — 10 |
| 22 | Platelet anisocytosis (PDW), % | 15 — 17 |
| 23 | Thrombocrit (PCT), % | 0,1 — 0,4 |
| 24 | Erythrocyte sedimentation rate (ESR), mm/hour men women | 1 — 10 2 -15 |
Neutrophils
Neutrophils come from red bone marrow, they are formed from a single stem cell, which is the ancestor of all blood cells. However, stem cells do not immediately turn into neutrophils. Between these two forms there are several stages, several intermediate forms.
There are 6 types of neutrophils:
- myeloblasts;
- promyelocytes;
- myelocytes;
- metamyelocytes;
- band neutrophils;
- segmented neutrophils.
Most of all is in the blood of the latter. They are present in an amount of 40–75% of the total number of leukocytes. The number of rod-shaped neutrophils is significantly smaller, they can be 1–6%. The number of young cells does not reach 1%.
And a separate table for children
Adaptation to new living conditions of all body systems of newborns, their further development in children after one year and final formation in adolescence makes blood indicators different from those in adults. It should not be surprising that the norms of a small child and a person who has crossed the age of majority can sometimes differ noticeably, so for children there is their own table of normal values.
| No. | Index | Norm |
| 1 | Red blood cells (RBC), 1012/l first days of life up to one year 1 - 6 years 6 - 12 years 12 - 16 years | 4,4 — 6,6 3,6 — 4,9 3,5 — 4,5 3,5 — 4,7 3,6 — 5,1 |
| 2 | Hemoglobin (HBG, Hb), g/l first days of life (due to fetal Hb) up to one year 1 - 6 years 6 - 16 years | 140 — 220 100 — 140 110 — 145 115 — 150 |
| 3 | Reticulocytes (RET), ‰ up to one year 1 - 6 years 6 - 12 12 - 16 | 3 — 15 3 — 12 2 — 12 2 — 11 |
| 4 | Basophils (BASO), % for all | 0 — 1 |
| 5 | Eosinophils (EO), % up to one year 1 – 12 years over 12 | 2 — 7 1 — 6 1 — 5 |
| 6 | Neutrophils (NEUT), % up to one year 1-6 years 6 - 12 years 12 - 16 years | 15 — 45 25 — 60 35 — 65 40 — 65 |
| 7 | Lymphocytes (LYM), % up to one year 1 - 6 years 6 - 12 years 12 - 16 years | 38 — 72 26 — 60 24 — 54 25 — 50 |
| 8 | Monocytes (MON), % up to one year 1 – 16 years | 2 -12 2 — 10 |
| 9 | Platelets109 cells/l up to one year 1 - 6 years 6 - 12 years 12 - 16 years | 180 — 400 180 — 400 160 — 380 160 — 390 |
| 10 | Erythrocyte sedimentation rate (ESR), mm/hour up to 1 month up to a year 1 – 16 years | 0 — 2 2 — 12 2 — 10 |
It should be noted that the normal values may differ in different medical sources and in different laboratories. This is not due to the fact that someone does not know how many certain cells there should be or what the normal level of hemoglobin is. Simply, using different analytical systems and techniques, each laboratory has its own reference values. However, these subtleties are unlikely to be of interest to the reader...
Next, we will analyze in more detail the main indicators of a general blood test and find out their role.
Description of the analysis
The mcv value is calculated based on data obtained from a general blood test. This is one of the most widespread and frequently prescribed laboratory tests. It allows you to comprehensively assess the condition of the entire hematopoietic system.
Erythrocyte indices, which are part of a general blood test, allow one to diagnose and classify various anemias with fairly high accuracy. Thanks to this, the doctor will be able to make an accurate diagnosis and prescribe the correct treatment regimen.
Since the analysis is simple, inexpensive and publicly available, it is used as a screening technique for identifying disorders in the hematopoietic system. Another advantage of the technique is the possibility of dynamic monitoring of the effectiveness of the treatment and timely adjustment of the dosages of drugs prescribed to the patient.
The result of the study may be affected by the presence of severe leukocytosis, a large number of reticulocytes, and a significant excess of normal glucose levels. All these conditions lead to an increase in the average size of the red blood cell.
It should also be taken into account that a simultaneous increase in macrocytic (large) and microcytic (small) red blood cells can create the appearance of normality. This is due to the fact that mcv is a calculated indicator that does not always reflect the objective state of blood cells. To identify abnormalities in such cases, direct microscopy of a blood smear taken from the subject is required.
Red blood cells in a general blood test and their characteristics
Erythrocytes or red blood cells (Er, Er) are the most numerous group of cellular elements of the blood, represented by nuclear-free biconcave discs ( the norm for women and men is different and is 3.8 - 4.5 x 1012 / l and 4.4 - 5, 0 x 1012/l respectively
). Red blood cells top the general blood count. Having numerous functions (tissue respiration, regulation of water-salt balance, transfer of antibodies and immunocomplexes on their surfaces, participation in the coagulation process, etc.), these cells have the ability to penetrate the most inaccessible places (narrow and convoluted capillaries). To carry out these tasks, red blood cells must have certain qualities: size, shape and high plasticity. Any changes in these parameters that go beyond the norm are shown by a general blood test (examination of the red part).
Red blood cells contain an important component for the body, consisting of protein and iron.
This is the red blood pigment called hemoglobin. A decrease in red blood cells usually entails a drop in Hb levels, although there is another picture: there are enough red blood cells, but many of them are empty, then the CBC will have a low content of red pigment. In order to find out and evaluate all these indicators, there are special formulas that doctors used before the advent of automatic analyzers. Now equipment deals with such matters, and additional columns with an incomprehensible abbreviation and new units of measurement have appeared in the general blood test form:
- RBC – total number of red blood cells (erythrocytes).
Old people remember that they used to be counted in Goryaev’s chamber up to millions per microliter (4.0 - 5.0 million was the norm). Nowadays the quantity is measured in SI units - tera per liter (1012 cells/l). An increase in the number of Er - erythrocytosis can be associated with psycho-emotional and physical stress, which should be taken into account when going for a general blood test. A pathological increase in red cells - erythremia, is usually associated with impaired hematopoiesis. Reduced values of the indicator (erythropenia) occur with blood loss, hemolysis, anemia, and decreased production of red blood cells. - HGB is hemoglobin,
it is a protein containing iron and is measured in grams per liter (g/l), although it is hardly worth dwelling on a detailed description of the indicator, since there is probably no person who does not know about the norm of hemoglobin (120 - 140 g/l in women, 130 – 160 g/l in men) and its main purpose – transport of oxygen (oxyhemoglobin) to tissues, carbon dioxide (carbohemoglobin) from them and maintaining acid-base balance. As a rule, when this indicator decreases, people think about anemia. A drop in hemoglobin below an acceptable level requires a comprehensive examination of the patient (search for the cause). hematocrit determination
HCT – hematocrit,
the indicator is expressed as a percentage. It can be observed if a bottle of preserved blood is left alone for spontaneous sedimentation of blood cells: the red saturated part that has settled to the bottom is the formed elements of blood, the yellowish liquid of the upper layer is plasma, the ratio between the fallen red blood cells and the total volume of blood is the hematocrit. An increase in the indicator is observed with erythremia, erythrocytosis, shock, polyuria, a decrease in the level is observed with anemia and an increase in circulating blood volume (CBV) due to an increase in plasma (for example, during pregnancy).
- The color indicator,
indicating the saturation of red blood cells (erythrocytes) with hemoglobin, is calculated using the formula: CP = hemoglobin (g/l) x 3: the first three digits of the number of red blood cells. For example, HGB (Hb) = 130 g/l, red blood cells = 4.1 X 1012/l, CP = (130 x 3): 410 = 0.95, which corresponds to the norm. - Red blood cell indices (MCV, RDW, MCH, MCHC)
are calculated based on the total number of red blood cells, hemoglobin level and the ratio of blood volume to red blood cells (hematocrit):- MCV (mean erythrocyte volume)
, expressed in femtoliters. The device adds together the volumes of normocytes, microcytes (midgets), macrocytes (large cells), megalocytes (giants) and calculates the average volume value. The indicator serves to determine the water-salt status and type of anemia. - RDWс - degree of diversity of erythrocytes
, showing how cells differ from each other in volume - anisocytosis (normocytes, microcytes, macrocytes, megalocytes). - MCH - (average Hb content in Er)
- an analogue of the color indicator, indicating the saturation of cells with hemoglobin (normochromia, hypo- or hyperchromia). - MCHC (mean content and mean concentration of blood pigment in red blood cells)
. MCHC correlates with indicators such as MCV and MCH and is calculated based on hemoglobin and hematocrit levels (MCHC below normal may primarily indicate hypochromic anemia or thalassemia).
An indicator of many diseases - ESR
ESR (erythrocyte sedimentation rate) is considered a (nonspecific) indicator of a wide variety of pathological changes in the body, so this test is almost never ignored in diagnostic searches. The ESR norm depends on gender and age - in absolutely healthy women it can be 1.5 times higher than this figure in children and adult men.
As a rule, an indicator such as ESR is written down at the bottom of the form, that is, it kind of completes the general blood test. In most cases, ESR is measured in 60 minutes (1 hour) in a Panchenkov stand, which is still indispensable to this day. However, in our high-tech times there are devices that can reduce the determination time, but not all laboratories have them.
determination of ESR
MCV is higher than normal
If the results are above normal, this indicates the development of macrocytic anemia. It can be directly related to diseases such as:
- drug intoxication;
- food poisoning;
- problems with the thyroid gland;
- lack of iodine or iron in the body;
- liver dysfunction;
- oncological process of red bone marrow;
- long-term alcoholism;
- disruption of the pancreas.
An increase in mcv can be caused by:
- long-term use of birth control pills that affect hormonal levels;
- addiction to cigarettes and tobacco products;
- prolonged contact with toxic substances (work in hazardous industries);
- taking medications that increase the level of mcv in the blood.
If left untreated, macrocytic anemia can lead to frequent fainting, poor health, and low hemoglobin levels in the blood. Particularly at risk are:
- people who eat poorly, lead a sedentary lifestyle and ignore exercise;
- patients with chronic liver failure;
- people with a genetic predisposition to the disease;
- men over fifty-five years of age who abuse alcohol.
Experts identify some signs by which one can understand that a person’s red blood cell volume is too high:
- unhealthy pale lips;
- abdominal pain for no particular reason, which appears very often;
- the presence of tachycardia (heartbeat too fast), even when the person is at rest;
- skin with a yellowish tint.
If you notice similar symptoms or detect an increased level of mcv in the blood, you must immediately consult a general practitioner for appropriate treatment.
Leukocyte formula
Leukocytes (Le) are a “motley” group of cells representing “white” blood. The number of leukocytes is not as high as the content of red blood cells (erythrocytes), their normal value in an adult ranges from 4.0 - 9.0 x 109/l
.
In the CBC, these cells are presented in the form of two populations:
- Granulocyte cells (granular leukocytes),
containing granules that are filled with biologically active substances (BAS): neutrophils (rods, segments, young, myelocytes), basophils, eosinophils; - Representatives of the agranulocytic series,
which, however, can also have granules, but of a different origin and purpose: immunocompetent cells (lymphocytes) and the “orderlies” of the body - monocytes (macrophages).
The most common cause of an increase in white blood cells (leukocytosis) is an infectious-inflammatory process:
- In the acute phase, the neutrophil pool is activated and, accordingly, increases (up to the release of young forms);
- A little later, monocytes (macrophages) are included in the process;
- The stage of recovery can be determined by the increased number of eosinophils and lymphocytes.
The calculation of the leukocyte formula, as mentioned above, is not completely trusted even by the most high-tech equipment, although it cannot be suspected of errors - the devices work well and accurately, and provide a large amount of information, significantly exceeding that when working manually. However, there is one tiny nuance - the machine cannot yet fully see the morphological changes in the cytoplasm and nuclear apparatus of the leukocyte cell and replace the doctor’s eyes. In this regard, identification of pathological forms is still carried out visually, and the analyzer is allowed to count the total number of white blood cells and divide leukocytes into 5 parameters (neutrophils, basophils, eosinophils, monocytes and lymphocytes), if the laboratory has a high-precision class 3 analytical system at its disposal .
Through the eyes of man and machine
The latest generation hematological analyzers are not only capable of conducting complex analysis of granulocyte representatives, but also differentiating agranulocytic cells (lymphocytes) within a population (subpopulations of T cells, B lymphocytes). Doctors successfully use their services, but, unfortunately, such equipment is still the privilege of specialized clinics and large medical centers. In the absence of any hematological analyzer, the number of leukocytes can be counted using the old old-fashioned method (in Goryaev’s chamber). Meanwhile, the reader should not think that one or another method (manual or automatic) is necessarily better; doctors working in the laboratory monitor this, monitoring themselves and the machine, and at the slightest doubt they will ask the patient to repeat the study. So, leukocytes:
- WBC is the number of white blood cells (leukocytes).
The calculation of the leukocyte formula is not trusted to any device, even the most high-tech (III class), since it is difficult for it to distinguish young from band and neutrophils, for the machine it is all the same - neutrophil granulocytes. The calculation of the ratio of different representatives of the leukocyte unit is undertaken by the doctor, who sees with his own eyes what is happening in the nucleus and cytoplasm of the cells. - GR – granulocytes
(in the analyzer). When working manually: granulocytes = all cells of the leukocyte series - (monocytes + lymphocytes) - an increase in the indicator may indicate the acute phase of the infectious process (an increase in the granulocyte population due to the neutrophil pool). In a general blood test, granulocytes are presented in the form of 3 subpopulations: eosinophils, basophils, neutrophils, and neutrophils, in turn, are present in the form of rods and segments or can appear without completing their maturation (myelocytes, young), when the hematopoietic process is disrupted or depleted reserve capabilities of the body (severe infections):- NEUT, neutrophils
(myelocytes, young, rods, segments) - these cells, having good phagocytic abilities, are the first to rush to protect the body from infection; - BASO, basophils
(increase – allergic reaction); - EO, eosinophils
(increase – allergies, helminthic infestation, recovery period). -
MON, Mo (monocytes)
are the largest cells that are part of the MNS (mononuclear phagocytic system). They, in the form of macrophages, are present in all inflammatory foci and are in no hurry to leave them for some time after the process has subsided. - LYM, Ly (lymphocytes)
- classified as immunocompetent cells, their various populations and subpopulations (T- and B-lymphocytes) are involved in the implementation of cellular and humoral immunity. Elevated values of the indicator indicate the transition of an acute process to a chronic one or to the recovery stage.
Platelet link
The next abbreviation in a complete blood count refers to cells called platelets or platelets. Studying platelets without a hematology analyzer is quite labor-intensive; the cells require a special approach to staining, so without an analytical system this test is performed as needed and is not a default analysis.
The analyzer, distributing cells like red blood cells, calculates the total number of blood platelets and platelet indices (MPV, PDW, PCT):
- PLT
is an indicator indicating the number of blood platelets (platelets). An increase in platelet levels in the blood is called thrombocytosis, a reduced level is classified as thrombocytopenia. - MPV
– average platelet volume, uniformity of platelet population sizes, expressed in femtoliters; - PDW
– width of distribution of these cells by volume – %, quantitatively – degree of platelet anisocytosis; - PCT
(thrombocrit) is an analogue of hematocrit, expressed as a percentage and indicates the proportion of platelets in whole blood.
An increased level of platelets and a change in platelet indices in one direction or another may indicate the presence of a rather serious pathology: myeloproliferative diseases, inflammatory processes of an infectious nature localized in various organs, as well as the development of a malignant neoplasm. Meanwhile, the number of platelets can increase: physical activity, childbirth, surgical interventions.
A decrease in the content of these cells is observed in autoimmune processes, thrombocytopenic purpura, atherosclerosis, angiopathy, infections, and massive transfusions. A slight drop in platelet levels is observed before menstruation and during pregnancy, but a decrease in their number to 140.0 x 109/l and below should already be a cause for concern.
Does everyone know how to prepare for analysis?
It is known that many indicators (especially leukocytes and red blood cells) vary depending on previous circumstances:
- Psycho-emotional stress;
- Intense physical activity (myogenic leukocytosis);
- Food (digestive leukocytosis);
- Bad habits such as smoking or thoughtless drinking of strong drinks;
- Use of certain medications;
- Solar radiation (it is not advisable to go to the beach before taking tests).
Nobody wants to get unreliable results, so you need to go for analysis on an empty stomach, sober and without a morning cigarette, calm down for 30 minutes, don’t run or jump. People should be aware that in the afternoon, after exposure to the sun and during heavy physical labor, some leukocytosis will be observed in the blood.
The female sex has even more restrictions, so representatives of the fair half need to remember that:
- The ovulation phase increases the total number of leukocytes, but decreases the level of eosinophils;
- Neutrophilia is observed during pregnancy (before childbirth and during its course);
- Pain associated with menstruation and the menstruation itself can also cause certain changes in the test results - you will have to donate blood again.
Blood for a detailed blood test, provided that it is carried out in a hematological analyzer, is now in most cases taken from a vein, simultaneously with other tests (biochemistry), but in a separate tube (a vacutainer with an anticoagulant placed in it - EDTA). There are also small microcontainers (with EDTA) designed for collecting blood from a finger (ear lobe, heel), which are often used to take tests from children.
The indicators of blood from a vein are somewhat different from the results obtained from the study of capillary blood - in venous blood there is higher hemoglobin and more red blood cells.
Meanwhile, it is believed that it is better to take OAC from a vein: the cells are less injured, contact with the skin is minimized, moreover, the volume of venous blood taken, if necessary, allows you to repeat the analysis if the results are questionable, or expand the range of studies (what if it turns out that what else needs to be done and reticulocytes?).
In addition, many people (by the way, most often adults), without reacting at all to venipuncture, are panicky afraid of the scarifier that is used to pierce the finger, and sometimes the fingers are blue and cold - it is difficult to obtain blood. The analytical system that performs a detailed blood analysis “knows” how to work with venous and capillary blood, it is programmed for different options, so it can easily “figure out” what’s what. Well, if the device fails, it will be replaced by a highly qualified specialist who will check, double-check and make a decision, relying not only on the capabilities of the machine, but also on his own eyes.
Eosinophils
Eosinophils are a small number of white blood cells that are found in human blood and tissues. They are an indispensable element that provides immunity.
Like other white blood cells, they are formed from bone marrow, and their progenitor is a single stem cell. The norm is 1–4%.
In total, eosinophils live about 12 days, but do not spend all of this time in the bloodstream. After 3-4 days of ripening, they enter the bloodstream and remain there for only 6-12 hours. Then they pass into the tissues and accumulate in especially large quantities in the lungs, under the mucous membrane of the digestive tract, and in the skin.
When the number of eosinophils increases, the condition is called eosinophilia, and the reverse change is called eosinopenia. As a rule, bright changes are symptoms of diseases, but some physiological fluctuations in their number are possible within normal limits. For example, an increase and decrease in eosinophils can be observed depending on the time of day; at night they are usually most in the blood.