Modern insulin preparations
Today it is difficult to imagine that just eighty years ago diabetes was an almost fatal disease. However, since 1939, the first insulin drug appeared on the market, and diabetic patients had a chance to live long and well. Today, according to scientists from the University of Pittsburgh, people with type 1 diabetes live up to 69 years1. What is the drug that gives diabetic patients a long and fulfilling life?
How it works?
Insulin is a hormone produced by beta cells of the pancreas. It is necessary for the cells of the body so that they can remove glucose from the blood and use it for their own “needs”.
In type 1 diabetes, the pancreas cannot produce enough insulin, and the only way to compensate for the dangerous deficiency is to administer the hormone externally as part of insulin therapy. In type 2 diabetes, insulin is produced in sufficient quantities, but the body's cells do not respond to it normally - the sensitivity of tissues to insulin decreases. To increase it, oral hypoglycemic drugs are administered, but in some cases, for example, when it is impossible to compensate for diabetes with pills alone, insulin is still prescribed.
Buy Actrapid HM solution for injection 100 IU/ml 10ml in pharmacies
Buy Actrapid HM in pharmacies Actrapid HM in the drug directory DOSAGE FORMS solution for injection 100IU/ml
MANUFACTURERS Novo Nordisk A/S (Denmark)
GROUP Short-acting insulins
COMPOSITION Soluble insulin (human genetically engineered).
INTERNATIONAL NON-PROPENTED NAME Soluble insulin (human genetically engineered)
SYNONYMS Actrapid HM Penfil, Biosulin R, Gansulin R, Gensulin R, Insuman Rapid GT, Insuran R, Rinsulin R, Rosinsulin R, Humodar R 100 Rec, Humulin Regular
PHARMACOLOGICAL ACTION Short-acting insulin preparation. The decrease in the concentration of glucose in the blood is due to an increase in its intracellular transport, increased absorption and assimilation by tissues, stimulation of lipogenesis, glycogenogenesis, protein synthesis, a decrease in the rate of glucose production by the liver (decreased glycogen breakdown), etc. After subcutaneous injection, the effect occurs within 20-30 minutes, reaches a maximum after 1-3 hours and lasts, depending on the dose, 5-8 hours. The duration of action of the drug depends on the dose, method, place of administration and has significant individual characteristics. The completeness of absorption depends on the route of administration (s.c., i.m.), injection site (abdomen, thigh, buttocks), dose, concentration of insulin in the drug, etc. It is unevenly distributed in tissues. Does not penetrate the placental barrier and into breast milk. Excreted by the kidneys.
INDICATIONS FOR USE Diabetes mellitus type 1, diabetes mellitus type 2: stage of resistance to oral hypoglycemic drugs, partial resistance to oral hypoglycemic drugs (combination therapy); diabetic ketoacidosis, ketoacidotic and hyperosmolar coma; diabetes mellitus that occurs during pregnancy (if diet therapy is ineffective); for intermittent use in patients with diabetes mellitus against the background of infections accompanied by high fever; for upcoming surgeries, injuries, childbirth, metabolic disorders, before switching to treatment with long-acting insulin preparations.
CONTRAINDICATIONS Hypersensitivity, hypoglycemia.
SIDE EFFECTS Allergic reactions (urticaria, angioedema - fever, shortness of breath, decreased blood pressure); hypoglycemia, hypoglycemic coma; hyperglycemia and diabetic acidosis (at low doses, skipping an injection, non-compliance with the diet, against the background of fever and infections); impaired consciousness (up to the development of a precomatous and comatose state); transient visual disturbances (usually at the beginning of therapy); immunological cross-reactions with human insulin; an increase in the titer of anti-insulin antibodies with a subsequent increase in glycemia; hyperemia, itching and lipodystrophy at the injection site. At the beginning of treatment, swelling and refractive error occur (they are temporary and disappear with continued treatment).
INTERACTION Pharmaceutically incompatible with solutions of other drugs. The hypoglycemic effect is enhanced by sulfonamides (including oral hypoglycemic drugs, sulfonamides), MAO inhibitors (including furazolidone, procarbazine, selegiline), carbonic anhydrase inhibitors, ACE inhibitors, non-steroidal anti-inflammatory drugs (including salicylates), anabolic steroids (including stanozolol, oxandrolone, methandrostenolone), androgens, bromocriptine, tetracyclines, clofibrate, ketoconazole, mebendazole, theophylline, cyclophosphamide, fenfluramine, Li+ preparations, pyridoxine, quinidine, quinine, chloroquinine, ethanol. The hypoglycemic effect is weakened by glucagon, somatropin, glucocorticosteroids, oral contraceptives, estrogens, thiazide and loop diuretics, slow calcium channel blockers, thyroid hormones, heparin, sulfinpyrazone, sympathomimetics, danazol, tricyclic antidepressants, clonidine, calcium antagonists, diazoxide, morphine, mar. ihuana, nicotine , phenytoin, epinephrine, H1-histamine receptor blockers. Beta-blockers, reserpine, octreotide, pentamidine can both enhance and weaken the hypoglycemic effect of insulin.
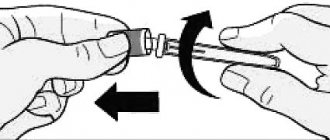
METHOD OF APPLICATION AND DOSAGE The dose and route of administration of the drug is determined individually in each specific case based on the glucose level in the blood before meals and 1-2 hours after meals, as well as depending on the degree of glucosuria and the characteristics of the course of the disease. The drug is administered subcutaneously, intravenously, intramuscularly, 15-30 minutes before meals. The most common route of administration is subcutaneous. For diabetic ketoacidosis, diabetic coma, during surgery - intravenously or intramuscularly. With monotherapy, the frequency of administration is usually 3 times a day (if necessary, up to 5-6 times a day), the injection site is changed each time to avoid the development of lipodystrophy (atrophy or hypertrophy of subcutaneous fat tissue). The average daily dose is 30-40 IU, in children - 8 IU, then in the average daily dose - 0.5-1 IU/kg or 30-40 IU 1-3 times a day, if necessary - 5-6 times a day. At a daily dose exceeding 0.6 U/kg, insulin must be administered in the form of 2 or more injections into different areas of the body. Can be combined with long-acting insulins. The insulin solution is drawn from the vial by piercing the rubber stopper with a sterile syringe needle, wiped with ethanol after removing the aluminum cap.
OVERDOSE Symptoms: hypoglycemia (weakness, “cold” sweat, pale skin, palpitations, trembling, nervousness, hunger, paresthesia in the hands, legs, lips, tongue, headache), hypoglycemic coma, convulsions. Treatment: the patient can eliminate mild hypoglycemia on his own by ingesting sugar or foods rich in easily digestible carbohydrates. Glucagon or a hypertonic dextrose solution is administered subcutaneously, intramuscularly or intravenously. When a hypoglycemic coma develops, 20-40 ml (up to 100 ml) of a 40% dextrose solution is injected intravenously until the patient emerges from the comatose state.
SPECIAL INSTRUCTIONS If foreign bodies appear, cloudiness or precipitation of the substance appears on the glass of the bottle, the drug cannot be used. The temperature of the administered insulin should be at room temperature. The dose of insulin must be adjusted in cases of infectious diseases, thyroid dysfunction, Addison's disease, hypopituitarism, chronic renal failure and diabetes mellitus in people over 65 years of age. The causes of hypoglycemia can be: insulin overdose, drug replacement, skipping meals, vomiting, diarrhea, physical stress; diseases that reduce the need for insulin (advanced kidney and liver diseases, as well as hypofunction of the adrenal cortex, pituitary gland or thyroid gland), change of injection site (for example, skin on the abdomen, shoulder, thigh), as well as interaction with other drugs. It is possible to reduce the concentration of glucose in the blood when transferring a patient from animal insulin to human insulin. Transferring a patient to human insulin should always be medically justified and carried out only under the supervision of a physician. The tendency to develop hypoglycemia can impair the ability of patients to actively participate in road traffic, as well as to maintain machines and mechanisms. Patients with diabetes can relieve self-perceived mild hypoglycemia by eating sugar or eating foods high in carbohydrates (it is recommended to always have at least 20 g of sugar with you). It is necessary to inform the attending physician about hypoglycemia in order to decide whether treatment adjustments are necessary. When treated with short-acting insulin, in isolated cases there may be a decrease or increase in the volume of adipose tissue (lipodystrophy) in the injection area. These phenomena can be largely avoided by constantly changing the injection site. During pregnancy, it is necessary to take into account a decrease (I trimester) or increase (II-III trimesters) in the need for insulin. During and immediately after childbirth, the need for insulin may decrease dramatically. During lactation, daily monitoring is necessary for several months (until insulin needs stabilize). Patients receiving more than 100 units of insulin per day require hospitalization when changing the drug.
STORAGE CONDITIONS List B. Store in a cool place at a temperature of 2-8 degrees. WITH.
Discovery of insulin
Pancreatic islets were discovered in 1869 by Paul Langerhans during a microscopic examination of the structure of the pancreas. In 1889, Oscar Malinowski in Germany, while removing a dog's pancreas, caused symptoms of diabetes mellitus. In 1921, F. Banting and C. Best isolated insulin from pancreatic islet cells, and D. Collip developed a method for its purification.
In 1922, insulin was first administered to a patient suffering from diabetes. Its therapeutic effect has shown that this type of therapy is the most effective. In subsequent years, the main efforts of scientists were aimed at organizing production in large quantities. In 1923, the Nobel Prize was awarded for the discovery and isolation of insulin. Subsequently, the amino acid structure of insulin was completely deciphered by F. Sanger.
What is insulin
Insulin is one of the most important hormones that is directly involved in metabolism:
- stimulates the exchange of glucose from the bloodstream into the body's cells;
- removes excess glucose from the liver;
- converts excess glucose into glycogen or fatty acids.
The main role of insulin is that it utilizes excess amounts of glucose into other compounds and stimulates the saturation of cells with this vital substance - the main source of energy.
The hormone also performs a number of additional functions:
- activation of amino acid biosynthesis;
- ensuring normal muscle function;
- regulation of enzyme metabolism;
- restoration of damaged tissues.
What to do if insulin is low
If the pancreas produces little insulin or does not synthesize it at all, urgent administration of the hormone artificially is required. To do this, they give injections or take tablets. The latter option is more convenient, since you do not need to give an injection, and it is also easier to take the package of tablets with you.
The dosage, frequency, and time of administration are determined by the doctor. Depending on the characteristics of administration, there are several types of insulin:
- fast acting - it starts working within 15-20 minutes after administration;
- short-acting – after 40-60 minutes;
- intermediate action – after 1-2 hours;
- long-acting - after 2-4 hours.
How to determine insulin levels
Insulin levels can be determined in a laboratory setting using a venous blood test. It is carried out for different purposes:
- detection of type 2 diabetes;
- identifying the need for artificial insulin intake;
- determining the causes of hypoglycemia (low blood glucose).
The analysis is carried out only as prescribed by a doctor. The main prerequisites are:
- sweating;
- blurred vision;
- cardiopalmus;
- frequent feeling of hunger;
- heart attacks;
- dizziness;
- to determine whether the insulinoma (pancreatic tumor) was successfully excised;
- for diagnosing relapses of insulinoma;
- to control the transplantation of Langerhans islet cells after the intervention.
Before conducting the study, certain preparation is required:
- do not eat food for at least 12 hours;
- do not take medications 24 hours in advance (check with your doctor);
- do not smoke at least 3 hours before the test.
Side effects
Hives
Danger! Quincke's edema!
In rare cases, the following complications may occur when using insulin:
- allergic reactions (urticaria, Quincke's edema, skin itching);
- a sharp decrease in blood sugar levels (develops due to the body’s rejection of the drug or in the event of an immunological conflict);
- disturbances of consciousness;
- in severe cases, hypoglycemic coma may develop;
- thirst, dry mouth, lethargy, decreased appetite;
- hyperglycemia (when using the drug against the background of infection or fever);
- facial redness;
- local reactions in the injection area (burning, itching, atrophy or proliferation of subcutaneous fatty tissue).
Sometimes adaptation to the drug is accompanied by disturbances such as swelling and visual disturbances. These symptoms usually disappear after a few weeks.
Terms of use
The most commonly used is subcutaneous injection of insulin.
Forming a fold
In emergency cases, the medicine is administered intravenously.
If the patient's condition is serious
Even an experienced diabetic can make a mistake when using the drug.
In order to avoid complications, you must:
- Before use, check the expiration date of the medicine.
- Follow storage recommendations: spare bottles should be stored in the refrigerator. The opened bottle can be stored at room temperature in a dark place.
- Make sure you remember the required dosage well: read the doctor's prescription again.
- Before injection, be sure to release the air from the syringe.
- The skin should be clean, but it is not advisable to use alcohol for treatment, as it reduces the effectiveness of the drug.
- Choose the optimal injection site. When injected under the skin of the abdomen, the drug will act faster. Insulin is absorbed more slowly when injected into the gluteal fold or shoulder.
- Use the entire surface area (prevention of the development of local complications). The distance between injections should be at least 2 cm.
- Grasp the skin in a fold to reduce the risk of getting into the muscle.
- Insert the syringe under the skin at an angle so that the medicine does not leak out.
- When injecting into the abdomen, administer short-acting insulin 20 minutes before meals. If you choose the shoulder or buttock - thirty minutes before meals.
What happens in the body after the drug is administered?
Subcutaneous injection
By connecting with the cell membrane receptor, insulin forms a complex that carries out the following processes:
- Improves intracellular transport of glucose and facilitates its absorption.
- Promotes the release of enzymes that are involved in the processing of glucose.
- Reduces the rate of formation of glycogen in the liver.
- Stimulates fat and protein metabolism.
In the case of subcutaneous administration, insulin begins to act within 20-25 minutes. The duration of action of the drug is from 5 to 8 hours. It is subsequently broken down by the enzyme insulinase and excreted in the urine. The drug does not cross the placenta and does not pass into breast milk.
What do the analysis results mean?
During the study, blood is drawn from a vein, after which the concentration of the hormone is determined using a chemical analysis. A value in the range from 2.6 to 24.9 µU/ml of blood is taken as normal.
If the norm is exceeded, the patient is sent for additional diagnostics to determine possible causes. The most common ones are:
- acromegaly;
- insulinoma;
- pancreas cancer;
- chronic pancreatitis;
- Itsenko-Cushing syndrome;
- obesity of varying degrees;
- intolerance to simple carbohydrates (glucose, galactose, fructose).