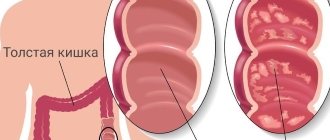
Colitis is an inflammatory disease that affects the large intestine. As the disease progresses, the intestinal mucosa atrophies, disrupting the functioning of one of the most important organs of the digestive system. Colitis can occur in all parts of the intestine at once (then it is called pancolitis) or in a specific section (then it is called segmental).
The symptoms are specific and extremely unpleasant, so patients usually consult a doctor on time. Often acute colitis becomes chronic; one of the most serious forms is ulcerative colitis. Erosion and ulcers form in the intestinal mucosa; symptoms occur during exacerbations.
At CELT you can get advice from a gastroenterologist.
- Initial consultation – 4,200
- Repeated consultation – 3,000
Make an appointment
Why does colitis develop?
Colitis is a polyethological disease. This means that doctors identify many different reasons for the development of this disease. The main reason is infection of the intestines by pathogens - bacteria, protozoa, helminths.
In addition to the direct cause, there are risk factors that can increase the likelihood of developing colitis:
- Taking medications that inhibit the natural intestinal microflora. As a result, normal flora dies and pathogenic microorganisms take its place. This result can be caused by: antibiotic therapy, long-term use of laxatives, and the use of suppositories.
- Chronic poisoning - chemical or food. Toxins penetrate the intestines through the bloodstream and inhibit the natural microflora.
- Stress, physical and mental overload.
- Exposure to heavy metal salts, work in hazardous industries.
- Diseases associated with circulatory disorders.
- Poor eating behavior: eating insufficiently processed food, frequent snacking on the go, dry food, addiction to spicy, salty and fatty foods.
- Alcohol abuse.
“Hand in hand” with dysbiosis
There are two forms of colitis - acute and chronic . In both the first and second cases, the infectious component plays a special role in the occurrence and development of the disease - most often bacterial dysentery . It can be triggered by other representatives of pathogenic microflora (for example, coli bacteria, staphylococci, streptococci, bacteria of the Proteus group, etc.). In other words, colitis goes “hand in hand” with dysbacteriosis. Inflammation can also be caused by previous intestinal infections and poor diet, as well as inadequate therapy with various medications. As practice shows, the causes of inflammation are indeed multiple. Let's summarize the main factors :
- infection in the gastrointestinal tract;
- infection with salmonella, staphylococci and other pathogenic microflora due to consumption of poor-quality food;
- the presence of worms (but not in all cases);
- inadequate, monotonous diet (mainly carbohydrates);
- allergies to certain types of food;
- chronic constipation;
- alcohol abuse;
- neglect of personal hygiene rules (for example, touching food with dirty hands);
- long-term use of certain antibiotics that can provoke dysbacteriosis;
- intoxication (poisoning with lead, arsenic and its preparations, mushrooms);
- nervous and emotional tension, stress.
Colitis ulcerosa - all Stages
Classification
There are several types of colitis:
- Ulcerative. Experts still find it difficult to name specific mechanisms for the development of this disease. It is known that the risk is increased by hereditary predisposition, as well as infectious diseases of the gastrointestinal tract.
- Infectious. Develops after infection with pathogenic and opportunistic microorganisms.
- Ischemic - occurs against the background of damage to blood vessels - the branches of the abdominal aorta, and the blood supply to the intestine is disrupted.
- Toxic. Occurs against the background of poisoning with various chemicals, including uncontrolled use of medications.
- Radiation is a consequence of radiation sickness. Anyone who works in an area of high radiation exposure, as well as patients receiving radiation therapy, are at risk.
- Spastic - the exact causes have not been established.
- Microscopic – lymphocytic, collagen. Inflammatory changes are diagnosed only by histological examination.
Symptoms and treatment of colitis depend on the type of colitis diagnosed.
Symptoms of colitis
Symptoms manifest in different ways. There are main signs of colitis - diarrhea and abdominal pain, but there are symptoms that may not appear for a long time.
Signs of colitis include:
- Abdominal pain of varying intensity and localization, constant or occurring at regular intervals.
- Bloating and flatulence, discomfort in the intestinal area.
- Periodically occurring chills, fever.
- Diarrhea, which may alternate with constipation.
- Frequent urge to defecate, including false ones.
- An admixture of blood and mucus in the stool. It is important to know that this symptom is characteristic of many intestinal diseases and in any case requires consultation with a doctor.
- Symptoms of dehydration with severe diarrhea: dizziness, weakness, rare urination, dry mouth, dry skin, feeling of “sand in the eyes.”
In adults, local intestinal signs of colitis are accompanied by general malaise. Weight loss may occur. Symptoms disappear with treatment. Progress before starting therapy. In the chronic form, sometimes you feel better than in the acute form. Symptoms are less obvious. Worries include loss of appetite, decreased performance, belching and nausea.
Clinical picture
In world practice, the severity of an attack (exacerbation) of UC is assessed using the disease activity index. There are several indices of UC activity (Rakhmilevich, Mayo, Oxford index, Swedish index, Truelov and Witts severity rating system, Montreal classification). There is no consensus among experts regarding the preferability of using any particular index, since all of them are not sufficiently validated. Currently, there is a tendency to additionally use the level of C-reactive protein (CRP) to assess activity, which is reflected in the European consensus (ECCO-consensus) on the diagnosis and treatment of UC. This document discusses all indices, with experts making the following conclusion: currently, to assess the severity of UC, it is necessary to take into account all parameters of the disease - clinical, laboratory, instrumental and histological [4]. The Expert Council of the Russian Group for the Study of Inflammatory Bowel Diseases (IBD) proposes a set of criteria that includes easily determined parameters for exacerbation of UC, including the level of CRP. This complex is broader than what is usually used when assessing activity indices, and therefore is more informative. The set of assessed disease parameters, to a greater extent than any indices (section 2.2.2.), corresponds to the expert assessment of the ECCO-consensus and takes into account both clinical and laboratory manifestations of the disease. This scoring system is an expanded modification of the UC severity criteria proposed by Truelov and Witts [6]. In accordance with the severity of clinical and laboratory symptoms, mild, moderate and severe UC are distinguished (see table).
The clinical picture of UC includes several groups of symptoms [1]:
• intestinal (blood in the stool, diarrhea, tenesmus);
• systemic extraintestinal autoimmune manifestations (arthropathy, skin lesions, aphthous stomatitis, eye lesions, primary sclerosing cholangitis, etc.);
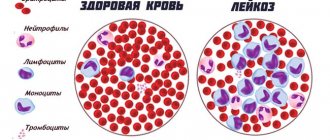
• endotoxemia syndrome (general intoxication, febrile fever, tachycardia, anemia, increased ESR, leukocytosis with a shift in the leukocyte formula to immature forms, toxic granularity of neutrophils, increased levels of acute-phase proteins - CRP, seromucoid, fibrinogen);
• metabolic disorders (weight loss, dehydration, hypoproteinemia, hypoalbuminemia, hypokalemia and other electrolyte disturbances).
Survey
Colonoscopy
- Cost: 25,000 rub.
More details
Diagnosis begins at a consultation with a gastroenterologist with examination and questioning. The nature of pain and discomfort and their duration play a big role. When diagnosing colitis, a whole range of instrumental studies is used:
- Colonoscopy. The most common endoscopic examination of the intestine.
- Sigmoidoscopy (examination of the rectum and anal area).
- Laboratory examination of stool (scatology, bacterial examination, inflammatory markers - calprotectin and others).
- X-ray examination using a contrast agent (irrigoscopy). Allows you to detect the exact localization of inflammation.
- Biopsy of the mucosa for histological examination. Allows you to clarify the diagnosis and exclude the possibility of a malignant neoplasm, which often manifests itself with the same symptoms as colitis.
Diagnostics is aimed at collecting the maximum amount of data about the disease. The doctor tries to find out the cause (it must be eliminated during treatment) and to clarify the localization of the inflammatory process. The more accurate the examination, the easier it is to choose effective treatment tactics.
Diagnostics
The complex of mandatory diagnostics includes macro- and microscopy of stool, coprogram, detection of helminth eggs, as well as bacteriological culture of stool. A general blood test is prescribed to determine the presence of signs of inflammation.
Contrast irrigoscopy is also performed to visualize the anatomical and functional features of the large intestine. Colonoscopy makes it possible to thoroughly examine the condition of the mucous membrane of the entire colon. During this study, it is also possible to obtain biopsies of the intestinal mucosa necessary for histological examination.
To exclude hemorrhoids, anal fissures, paraproctitis and other proctological pathologies, the proctologist performs a digital examination of the anus.
How to treat intestinal colitis in adults
Chronic colitis is treated on an outpatient basis or in a hospital, depending on the severity of the condition. The doctor selects treatment tactics. If the cause of acute colitis is an infectious agent, then treatment is carried out in the infectious diseases department.
For any type of colitis, depending on the clinical picture, the following prescriptions are made:
- Diet 4 or 3.
- Taking adsorbent drugs.
- Drugs that normalize intestinal motility.
- Laxatives or antidiarrheals.
- Drugs that stimulate the regeneration of the intestinal mucosa.
- Anti-inflammatory drugs.
- Preparations that promote the growth of normal microflora (prebiotics and probiotics).
- Detoxification.
- Taking vitamins, minerals, treatment with mineral waters, physical therapy.
During treatment, it is necessary to try to eliminate the cause of colitis, for which the following are prescribed:
- antiparasitic drugs;
- antimicrobials;
- vascular drugs to improve blood circulation.
Colitis is a disease that is sufficiently amenable to conservative treatment. CELT clinic specialists will help you cope with the problem. Examination using the latest equipment guarantees an accurate diagnosis. Many years of experience of doctors works for your health.
Features and benefits of treatment for ulcerative colitis at the Rassvet Clinic
Doctors at the Rassvet Clinic use treatment protocols for ulcerative colitis developed by the world's leading associations (ACG, ECCO) and based on reliable scientific research. Our specialists do not use unproven methods for treating ulcerative colitis, such as a strict diet, and help create a treatment plan during pregnancy and breastfeeding. To protect against the side effects of immunosuppressants, the doctor will propose a vaccination plan and draw up a schedule of blood tests that will allow timely recognition of unwanted reactions to medications.
Author:
Golovenko Alexey Olegovich gastroenterologist
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Sigmoidoscopy | 2 500 |
| Colonoscopy (video colonoscopy) | 7 000 |
| Irrigoscopy | 7 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions