General information
A condition called thrombocytopenia is characterized by a decrease in the number of platelets in the blood to less than 150 x 109/L. As a result, the patient experiences increased bleeding and difficulty stopping the bleeding . Thrombocytopenia (ICD-10 code - D69.6 Thrombocytopenia, unspecified) may accompany hematological diseases. However, an independent disease is also diagnosed - idiopathic thrombocytopenic purpura (ICD-10 code - D69.3), as well as an autoimmune form of the disease.
Speaking about thrombocytopenia - what kind of disease it is, it should be noted that it develops as a result of a disruption in the production of platelets or too active destruction of them. The autoimmune form of the disease is most often diagnosed. This condition can also develop against the background of a number of diseases: herpes , hepatitis , HIV, infectious mononucleosis , influenza . It can also be provoked by some exogenous factors. What thrombocytopenia is, the causes and treatment of this disease are described in detail in this article.
Types of thrombocytopenia
Depending on the causes of development, thrombocytopenia is divided into several types.
Hereditary
A group of diseases caused by a genetic mutation:
- May–Hegglin anomaly;
- congenital amegakaryocytic thrombocytopenia;
- Wiskott–Aldrich syndrome;
- TAR – syndrome;
- Bernard–Soulier syndrome.
Productive
A group of diseases of the hematopoietic organs with a characteristic change in the process of platelet production by red bone marrow:
- acute leukemia;
- aplastic anemia;
- myelofibrosis;
- myelodysplastic syndrome;
- megaloblastic anemia.
Also, a productive form of the disease can develop as a result of metastasis of a cancerous tumor (the diagnosis is made and treated by an oncologist), the use of cytostatic drugs, hypersensitivity to medications, exposure to radiation, and alcohol abuse.
Destruction
Leads to increased destruction of platelets in the spleen, sometimes in the liver or lymph nodes:
- idiopathic thrombocytopenic purpura;
- post-transfusion thrombocytopenia;
- thrombocytopenia of newborns;
- Evans–Fisher syndrome;
- drug and viral thrombocytopenia.
Consumption
Platelets are activated in the vascular bed, which triggers the blood coagulation mechanism, which has a pronounced symptomatic character. The greater the consumption of platelets, the more the body tends to produce them.
If the cause of activation is not eliminated, the compensatory capabilities of the red brain will be exhausted:
- hemolytic-uremic syndrome;
- thrombotic thrombocytopenic purpura;
- disseminated intravascular coagulation syndrome;
Breedings
It develops as a consequence of massive bleeding, during which the patient was transfused with a large volume of fluid, plasma substitute, plasma or red blood cells. However, the moment of need to compensate for platelet loss was missed.
Their concentration in the blood decreases so much that the emergency release of platelets from the depot does not help maintain adequate functioning of the coagulation system.
Redistributions
A consequence of impaired platelet deposition due to splenomegaly. 90% of platelets settle in the spleen, which literally “confuses the body.” Regulatory systems take into account their total amount, and not the amount that circulates in the blood.
Doctor's advice
Many people wonder whether thrombocytopenia is curable. It depends on the reason. If it is an infection, then when it is cured, all symptoms go away. In case of liver pathologies, complete relief from thrombocytopenia is also possible. If it’s leukemia, then when the condition stabilizes, the platelet count increases, but there will be concern about a relapse. In the case of congenital genetic abnormalities, the disease cannot go away because the body does not work correctly. But there is always supportive therapy that allows you to maintain a decent standard of living.
Victoria Druzhikina Neurologist, Therapist
A large percentage of deposition by the spleen leads to a compensatory increase in their production, this happens when:
- liver cirrhosis (hepatologist treats and consults);
- systemic lupus erythematosus;
- alcoholism;
- lymphoma or leukemia;
- infectious invasion: malaria, hepatitis, tuberculosis, etc.
In children
In a child, the pathology is expressed in a typical symptomatic complex, complicated by hemorrhagic syndrome. It develops against the background of a decrease in the number of platelets, due to their rapid destruction or insufficient production.
An increased rate of platelet destruction is a consequence of:
- immunopathological processes leading to heteroimmune, transimmune and isoimmune thrombocytopenia;
- vasopathy, Kasabach-Merritt syndrome, systemic inflammatory response syndrome, respiratory system disorder syndrome, aspiration syndrome, pneumonia, pulmonary hypertension, infectious invasions, disseminated intravascular coagulation syndrome;
- thrombocytopathies of Wiskott-Aldrich, Shwachman-Diamond, May-Hegglin,
- overdose of certain drugs, hyperbilirubinemia, acidosis, generalized form of viral infections, long-term parenteral nutrition;
- isolated or generalized post-traumatic thrombosis, hereditary deficiency of antithrombin III and protein C, antiphospholipid syndrome in the mother;
- blood transfusion, hemosorption, plasmapheresis.
A common cause of decreased platelet production in children is megakaryocytic hypoplasia caused by TAR syndrome, leukemia, aplastic anemia, neuroblastoma, and trisomy.
Newborns are at risk when the rate of thrombocytopoiesis in the mother decreases, preeclamptic conditions during pregnancy, extremely low birth weight, antenatal hemolytic disease, deficiency of thrombocytopoietin production, etc.
Children's thrombocytopenia can develop against the background of severe suffocation, infection, sepsis, polycythemia, and thyrotoxicosis. A pediatrician treats diseases in children.
For infants, the pathology is dangerous due to an asymptomatic increase in the rate of platelet destruction.
Only 5-7% of total cases of childhood thrombocytopenia are associated with a quantitative decrease in platelet synthesis.
Pathogenesis
Platelets are blood cells that are produced in the bone marrow. They live in the body for a little more than a week, after which they disintegrate in the spleen and liver. The main functions of these cells in the body are to prevent the development of bleeding. The cells stick together and a blood clot forms, blocking the wounded vessel. In addition, they determine the synthesis of growth factors that affect tissue repair processes. Platelet levels may fluctuate depending on certain factors. However, such fluctuations are physiological and temporary. Normally, the level of these cells is 150 thousand per microliter (150 x 109/l). If the platelet count decreases, we are talking about thrombocytopenia.
Currently, the pathogenesis of this disease has not been sufficiently studied.
The mechanism of development of the disease may be associated with the following factors:
- impaired platelet production by the bone marrow;
- disruption of their distribution in the vascular bed;
- platelet deficiency and increased destruction.
Idiopathic thrombocytopenic purpura develops due to an autoimmune reaction that is directed against one’s own platelets. This immune reaction is a complex cyclic process in which B lymphocytes, T lymphocytes, macrophages , NK cells, and cytokines participate. Antibodies to platelets are not always detected in the blood.
In children, the development of ITP often occurs after acute respiratory viral infections. When the platelet count falls below 10 x 109/L, the bleeding period prolongs.
How does thrombocytopenia manifest?
Treatment
Since the genesis of immune thrombocytopenia is not clear, a complete cure for this disease is not yet possible. However, therapy can significantly improve the quality of life of a patient with immune thrombocytopenia and cause stable remission. According to the generally accepted protocol, it includes:
Glucocorticosteroids (GCS)
In 70-80% of cases, the use of drugs of this type is effective. However, in 60-70% of cases, remission is unstable and eventually gives way to relapse.
In this case, glucocorticosteroids can provoke side effects:
- Decreased glucose tolerance;
- Suppression of adrenal function;
- Diseases of the gastrointestinal tract;
- Increased risk of developing fungal, viral, bacterial infections;
- Problems in the field of emotional regulation: increased excitability, anxiety, depressive states;
- Osteoporosis;
- Weight gain.
For this reason, GCS are contraindicated in diabetes mellitus, infectious diseases, mental diseases, etc.
To prevent the occurrence of side effects from taking glucocorticosteroids or reduce their severity, in parallel, the doctor prescribes concomitant therapy.
High-dose normal human immunoglobulin G (IVIG)
The effectiveness of this product is 80%. It is prescribed to those who, for any reason, are contraindicated to take GCS. IVIG is administered intravenously using a drip. Usually 2-5 sessions are required.
Splenectomy
If GCS and IVIG are not effective or if, for any reason, they cannot be used, a more radical remedy is used - splenectomy. Those. surgical removal of the spleen. This gives a quick positive effect in 80-88% of cases. At the same time, in 60-70% the remission turns out to be long-term.
Thromboetin receptor agonists
This is a whole group of drugs that can become an alternative to radical methods. Some are administered subcutaneously, others are taken orally. Their effectiveness varies depending on the product from 80 to 40%. Taking this group of medications helps normalize platelet levels, but after stopping treatment, thrombocytopenia returns in most patients. Only some experience long-term, stable remission.
The selection of a specific treatment regimen is carried out by a doctor. Only a qualified specialist can take into account all the factors and prescribe the appropriate therapy for your case. Self-medication is strictly not recommended.
Classification
The disease is divided according to several characteristics. Taking into account the origin, it is determined:
- Primary thrombocytopenia - development is associated with a violation of hematopoietic processes, the production of antibodies in the body that destroy platelets.
- Secondary thrombocytopenia develops against the background of other diseases. The secondary form of the disease can also be the result of serious poisoning, radiation, or alcoholism.
The types of thrombocytopenia are determined by:
- Immune thrombocytopenia - this condition develops if the immune system begins to perceive platelets as foreign agents. As a result, immune thrombocytopenia leads to the destruction of platelets by the body's immune system.
- Essential thrombocytopenia - this form of the disease most often affects older people, after 50 years. The essential form often develops after surgical operations, as well as against the background of chronic diseases of internal organs and iron deficiency.
- Idiopathic thrombocytopenic purpura is most often diagnosed in children. The disease is associated with blood clotting disorders.
- Thrombocytopenia in newborns can accompany congenital pathological conditions, and also develop as a secondary disease during asphyxia during childbirth, infection of the child, etc.
Taking into account the severity of the disease, it is determined:
- Easy . The platelet level is the lower limit of normal (30-50 x 109/l), symptoms of pathology do not appear. Sometimes nosebleeds occur. As a rule, this condition is determined by chance, during preventive tests. In this case, no treatment is required; the doctor monitors the patient’s condition.
- Average. The platelet level is reduced (20-50 x 109/l). There are hemorrhages under the skin, even with minor blows noticeable hematomas occur, and frequent nosebleeds are a concern. Small rashes may appear on the body. Treatment of the condition is carried out if there is a threat of internal bleeding.
- Heavy. The platelet level is very low, sometimes critical (less than 20 x 109/l). Extensive internal bleeding and multiple skin rashes develop. Treatment is mandatory and the patient should be hospitalized.
Based on the nature of the disorders, the following forms of thrombocytopenia are distinguished:
- isoimmune;
- transimmune;
- heteroimmune;
- autoimmune.
The nature of the flow determines:
- acute (up to six months);
- chronic:
- with rare relapses;
- continuously relapsing.
Causes
Why this disease occurs is unknown. Doctors talk about hereditary predisposition and the negative effects of the following factors:
- bacterial and viral infections;
- vaccinations;
- excessive exposure to solar radiation (insolation);
- general hypothermia of the body;
- some medications (Indomethacin, Furosemide).
On the surface of platelets there are molecular complexes called antigens. If a foreign antigen enters the body, the immune system immediately begins to produce specific antibodies. By interacting with antigens, they destroy the cells on whose surface they are located.
In essential thrombocytopenia, the spleen produces antibodies to its platelet antigens. They are fixed on platelet membranes and, as it were, mark them. As they pass through the spleen, blood cells are captured and destroyed.
Due to a decrease in the number of platelets, the liver begins to produce them more. The rate of maturation of megakaryocytes and the formation of platelets from them in the red bone marrow increases significantly. But gradually the compensatory capabilities of the bone marrow become thinner, and the disease makes itself felt.
If autoimmune thrombocytopenia is diagnosed during pregnancy, this means that antibodies to one’s own platelets cross the placental barrier and destroy normal fetal platelets. As a result, the child may be born sick.
Thrombocytopenia consumption
Platelets are activated in the vascular bed, and the blood clotting mechanism is activated. Due to the increased consumption of platelets, the red bone marrow begins to actively produce them, and if the cause of the pathology is not eliminated in time, their level in the blood will decrease to a critical level.
The activation of formed elements is caused by:
- Thrombotic thrombocytopenic purpura. Caused by an insufficient amount of prostacyclin in the blood. This anticoagulant factor is produced by the endothelium and prevents platelets from sticking to each other. When its release is disrupted, local platelet activation occurs and microthrombi form. Vessels are damaged and intravascular hemolysis develops.
- Disseminated intravascular coagulation syndrome. Appears as a result of severe damage to internal organs or tissues (infections, burns, injuries, surgeries, etc.), due to which the blood coagulation system is depleted. Numerous blood clots form in the vascular bed. They clog small vessels, preventing normal blood supply to the kidneys, brain and other organs. In response, the anticoagulant system is activated, aimed at restoring blood flow by breaking up blood clots. Over time, the blood completely loses its ability to clot. Severe internal bleeding may occur, which can be fatal.
- Hemolytic-uremic syndrome. Associated with intestinal infections, hereditary predisposition, systemic diseases and the use of certain medications. Bacterial toxins are released into the blood. They damage the vascular endothelium and activate platelets by attaching them to damaged areas. As a result, microthrombi are formed and microcirculation of internal organs is disrupted.
Thrombocytopenia redistribution
Normally, about 30% of all platelets are deposited in the spleen. In some diseases, the organ greatly increases in size, which is why up to 90% of the formed elements of blood are deposited in it. The disease can be caused by cirrhosis of the liver, systemic lupus erythematosus, infections, tumors, and alcoholism.
Thrombocytopenia dilution
Develops in patients who are transfused with large volumes of plasma, fluids, red blood cells, plasma substitutes, without replacing platelets. As a result, the concentration of the latter decreases to such a level that even their release from the depot is not able to maintain the normal functioning of the coagulation system.
Causes of thrombocytopenia
The reasons for the decrease in platelet levels in children and adults are due to the fact that they are being destroyed too actively, or an insufficient number of them is formed in the body.
The following conditions can lead to platelet destruction:
- idiopathic thrombocytopenic purpura;
- other autoimmune diseases - lupus erythematosus , rheumatoid arthritis ;
- previous surgical operations ( heart bypass surgery );
- side effects of certain medications;
- preeclampsia in pregnant women.
The causes of thrombocytopenia in adults, leading to decreased platelet production, may be the following:
- viral diseases - hepatitis C , chickenpox , HIV , mononucleosis , etc.;
- oncological diseases – leukemia , lymphoma ;
- bone marrow irradiation;
- chemotherapy;
- alcoholism;
- deficiency of folic acid , vitamin B12 .
Diagnostics
The presence of thrombocytopenia in children and adults is indicated by a decrease in the number of platelets in the blood. To make an accurate diagnosis and prescribe quality treatment, additional studies are carried out, which can be completed in any modern hematology clinic
:
- general blood analysis;
- Duke bleeding time assessment;
- puncture of red bone marrow (allows you to study the state of the hematopoietic system);
- determination of blood clotting time;
- genetic research (carried out if hereditary thrombocytopenia is suspected);
- determination of antibodies in the blood (clarification of the ratio of antibodies and platelets);
- Ultrasound (makes it possible to study the density and structure of internal organs, determine the size of the liver and spleen);
- MRI (to obtain layer-by-layer images of blood vessels and internal organs).
Symptoms
Thrombocytopenia in adults is manifested by a number of symptoms that depend on the severity of the disease. Signs may be as follows:
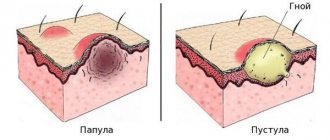
- the appearance of spontaneous hemorrhages in the mucous membranes and under the skin;
- nausea, dizziness ;
- prolonged bleeding after tooth extraction;
- increasing the period of bleeding cessation;
- spontaneous appearance of hematomas in different parts of the body;
- severe drowsiness , loss of strength;
- increased nosebleeds;
- very heavy periods.
Speaking about what thrombocytopenia is in adults, it should be noted that the results of a blood test for thrombocytopenia show from 0 to 50 per 10 in 9 platelets / l.
Tests and diagnostics
The main test to determine thrombocytopenia is a clinical blood test that determines platelet levels.
If, based on the test results, the patient is diagnosed with congenital thrombocytopenia , a bone marrow examination is performed. megakaryocytes is determined . If they are absent, this indicates a disruption in the process of platelet formation, if they were present - we are talking about the deposition of platelets in the spleen or their peripheral destruction.
To determine the causes of the development of pathology, the doctor may prescribe the following studies:
- antibody tests;
- genetic tests;
- Ultrasound;
- electrocardiogram;
- endoscopic examination;
- radiography.
Publications in the media
Thrombocytopenia is a low platelet count in the peripheral blood, the most common cause of bleeding. When the platelet count decreases to less than 100´109/l, the bleeding time lengthens. In most cases, petechiae or purpura appear when the platelet count drops to 20–50´109/l. Serious spontaneous bleeding (eg, gastrointestinal) or hemorrhagic stroke occurs when thrombocytopenia is less than 10´109/L.
Etiology and pathogenesis
• Thrombocytopenia can occur as a manifestation of drug allergies (allergic thrombocytopenia), caused by the production of antiplatelet antibodies (autoimmune thrombocytopenia), caused by infections, intoxications, thyrotoxicosis (symptomatic).
• In newborns, thrombocytopenia can be caused by the penetration of autoantibodies of a sick mother through the placenta (transimmune thrombocytopenia).
• Pathology of thrombocytopoiesis •• Maturation of megakaryocytes is selectively suppressed by thiazide diuretics and other drugs, especially those used in chemotherapy, ethanol •• A special cause of thrombocytopenia is ineffective thrombopoiesis associated with the megaloblastic type of hematopoiesis (occurs with deficiency of vitamin B12 and folic acid, as well as with myelodysplastic and preleukemic syndromes). Morphologically and functionally abnormal (megaloblastic or dysplastic) megakaryocytes are identified in the bone marrow, giving rise to a pool of defective platelets that are destroyed in the bone marrow •• Amegakaryocytic thrombocytopenia is a rare cause of thrombocytopenia caused by a congenital deficiency of megakaryocyte colony-forming units.
• Anomalies in the formation of the platelet pool occur when platelets are eliminated from the bloodstream, the most common cause is deposition in the spleen •• Under normal conditions, the spleen contains a third of the platelet pool •• The development of splenomegaly is accompanied by the deposition of a larger number of cells with their exclusion from the hemostasis system. With a very large size of the spleen, it is possible to deposit 90% of the total platelet pool •• The remaining 10% in the peripheral bloodstream has a normal circulation duration.
• Increased platelet destruction in the periphery is the most common form of thrombocytopenia; Such conditions are characterized by a shortened platelet lifespan and an increased number of bone marrow megakaryocytes. These disorders are referred to as immune or nonimmune thrombocytopenic purpura • • Immune thrombocytopenic purpura • • • Idiopathic thrombocytopenic purpura (ITP) is the prototype of thrombocytopenia due to immune mechanisms (no obvious external causes of platelet destruction). See Idiopathic thrombocytopenic purpura ••• Other autoimmune thrombocytopenias caused by the synthesis of antiplatelet antibodies: post-transfusion thrombocytopenia (associated with exposure to isoantibodies), drug-induced thrombocytopenia (for example, caused by quinidine), thrombocytopenia caused by sepsis (the incidence can reach 70%), thrombocytopenia in combination with SLE and other autoimmune diseases. Treatment is aimed at correcting the underlying pathology. It is necessary to stop taking all potentially dangerous drugs. GK therapy is not always effective. Transfused platelets undergo the same accelerated destruction • • Nonimmune thrombocytopenic purpura ••• Infections (eg, viral or malaria) ••• Massive transfusion of preserved blood with a low platelet count ••• DIC ••• Prosthetic heart valves ••• Thrombotic thrombocytopenic purpura .
Genetic aspects
• Thrombocytopenia (*188000, Â). Clinical manifestations: macrothrombocytopenia, hemorrhagic syndrome, rib aplasia, hydronephrosis, recurrent hematuria. Laboratory tests: autoantibodies to platelets, shortened platelet life, increased clotting time, normal tourniquet test, defects in the plasma component of hemostasis.
• May–Hegglin anomaly (Hegglin syndrome, 155100, Â). Macrothrombocytopenia, basophilic inclusions in neutrophils and eosinophils (Döhle bodies).
• Epstein syndrome (153650, Â). Macrothrombocytopenia in combination with Allport syndrome.
• Fechtner family syndrome (153640, Â). Macrothrombocytopenia, inclusions in leukocytes, nephritis, deafness.
• Congenital thrombocytopenia (600588, deletion 11q23.3–qter, Â). Clinical manifestations: congenital dysmegakaryocyte thrombocytopenia, mild hemorrhagic syndrome. Laboratory studies: 11q23.3-qter deletion, increased number of megakaryocytes, giant granules in peripheral blood platelets.
• Cyclic thrombocytopenia (188020, Â). Hemorrhagic syndrome, cyclic neutropenia.
• Thrombocytopenia Paris–Trousseau (188025, deletion 11q23, defect of the TCPT gene, Â). Clinical manifestations: hemorrhagic syndrome, thrombocytopenia, hypertelorism, ear abnormalities, mental retardation, coarctation of the aorta, developmental delay in the embryonic period, hepatomegaly, syndactyly. Laboratory studies: giant granules in platelets, megakaryocytosis, micromegakaryocytes.
• TAR syndrome (from: t hrombocytopenia – a bsent r adius - thrombocytopenia and absence of the radius, *270400, r). Congenital absence of the radius in combination with thrombocytopenia (pronounced in children, later smoothed out); thrombocytopenic purpura; in the red bone marrow there are defective megakaryocytes; Anomalies of kidney development and congenital heart disease are sometimes noted.
The clinical picture is determined by the underlying disease that caused thrombocytopenia.
Diagnostics • Thrombocytopenia is an indication for examining the bone marrow for the presence of megakaryocytes; their absence indicates a violation of thrombocytopoiesis, and their presence indicates either peripheral destruction of platelets, or (in the presence of splenomegaly) platelet deposition in the spleen • Pathology of thrombocytopoiesis. The diagnosis is confirmed by identifying megakaryocytic dysplasia in a bone marrow smear • Abnormalities in the formation of the platelet pool. The diagnosis of hypersplenism is made when there is moderate thrombocytopenia, a normal number of megakaryocytes is detected in the bone marrow smear, and a significant enlargement of the spleen • Diagnosis of idiopathic thrombocytopenic purpura requires the exclusion of diseases associated with thrombocytopenia (for example, SLE) and thrombocytopenia caused by taking medications (for example, quinidine). Available but nonspecific methods for detecting antiplatelet antibodies are known.
TREATMENT
• Pathology of thrombocytopoiesis. Treatment is based on eliminating the offending agent, if possible, or treating the underlying disease; The half-life of platelets is usually normal, allowing platelet transfusions in the presence of thrombocytopenia and signs of bleeding. Thrombocytopenia caused by deficiency of vitamin B12 or folic acid disappears when their normal levels are restored.
• Amegakaryocytic thrombocytopenia responds well to treatment; antithymocyte immunoglobulin and cyclosporine are usually prescribed.
• Anomalies in the formation of the platelet pool. There is usually no treatment, although splenectomy may resolve the problem. During transfusions, some platelets are deposited, making transfusions less effective than in states of reduced bone marrow activity.
• Treatment of idiopathic thrombocytopenic purpura - see Idiopathic thrombocytopenic purpura.
Complications and associated conditions • Decreased platelet production is associated with aplastic anemia, myelophthisis (replacement of bone marrow by tumor cells or fibrous tissue) and some rare congenital syndromes • Evans syndrome (Fisher-Evans syndrome) - a combination of autoimmune hemolytic anemia and autoimmune thrombocytopenia.
ICD-10 • D69 Purpura and other hemorrhagic conditions
Treatment with folk remedies
If the treatment of thrombocytopenia is carried out according to the regimen prescribed by the doctor, then after consultation with a specialist, you can try to improve the general condition of the body using folk remedies. However, it is important to understand that treatment of thrombocytopenia with folk remedies should under no circumstances replace therapy prescribed by a doctor.
You can use the following traditional methods:
- Verbena infusion. Pour 5 g of verbena into a glass of boiling water. Leave for half an hour. Drink a glass every day for a month.
- Sesame oil. Every day you should consume 10 g of oil, adding it to a salad or consuming it separately from food.
- Stinging nettle. Pour 10 g of dry raw material into a glass of boiling water and boil for 10 minutes. Drink 20 ml 3 times a day.
- Burnet decoction. An effective remedy for stopping bleeding. 2 tbsp. l. pour the product into a glass of water and boil for 15 minutes. After 3 hours, strain, drink 20 minutes before meals, 3 tbsp. l.
- Herbal collection. Mix 30 g of yarrow flowers and shepherd's purse. 1 tbsp. l. Pour 0.5 liters of boiling water over this mixture and leave for several hours. Drink half a glass three times a day before meals.
- Rose hip decoction. Pour 50 g of rose hips into 0.5 liters of water and cook for 5 minutes. Pour into a thermos and leave overnight. Drink instead of tea, adding honey.
- Viburnum bark. 2 tbsp. l. dry raw materials, pour 300 ml of water, cook for half an hour. Strain and add water to get the original volume. Drink 4 times a day, 2 tbsp. l.
- Dried fruits. It is necessary to chop 200 g of dried apricots, figs, raisins, and prunes. Add 200 g of honey and the juice of 2 lemons to the mixture. Place the mixture in small jars and store them in the refrigerator. In the morning, take 1 tbsp. l. facilities.
- Beetroot juice. Mix fresh beet juice with equal amounts of cucumber and carrot juice. Take a glass of this remedy in the morning, then have breakfast an hour later.
In children
When discussing the treatment and causes of thrombocytopenia in children, it should be noted that this condition can be congenital, accompanying pathologies in newborns. Thrombocytopenia may also be a secondary disease. The reasons for this are related to infection of the child, premature birth or asphyxia during childbirth.
The causes of thrombocytopenia in children depend on the form of the disease.
- Idiopathic thrombocytopenic purpura develops with a frequency of 3-5 cases per 100 thousand children. Most often diagnosed in school-age children. Most often it manifests itself in children who have recently suffered a viral disease - mumps , measles , chickenpox , rubella , etc.
- Secondary thrombocytopenia can develop against the background of certain diseases ( hepatitis , cytomegalovirus infection ), taking a number of medications ( Heparin , Abciximab , etc.).
In order to recognize the disease in a child in time, parents should pay attention to the characteristic manifestations of the disease. In this condition, bleeding develops - pinpoint hemorrhages appear on the skin, frequent nosebleeds, gum bleeding, and gastrointestinal bleeding are disturbing. It is important to understand that internal bleeding can threaten the baby's life.
If the diagnosis has been confirmed through research, it is important to properly treat thrombocytopenia in children. His regimen is prescribed by a doctor.
Treatment is prescribed if the platelet count is less than 20-30 thousand per microliter. But most often, the doctor is guided by the presence of pronounced clinical manifestations before prescribing a treatment regimen. The specialist may prescribe corticosteroids ( Prednisolone , Dexamethasone ). In severe cases, cytostatics ( Vincristine , Vinblastine ) and immunosuppressants ( Azathioprine , Cyclosporine ) are prescribed. In rare cases, the spleen is removed.
But most often, the platelet count in children becomes normal over time on its own, without treatment. According to statistics, in 60% of children the condition returns to normal after a month and a half, in 80% of children - after 6 months.
But in any case, over a certain period it is necessary to visit a doctor and conduct control blood tests.
In addition, parents must adhere to some important rules to protect their baby:
- It is important that the child does not engage in activities that could cause injury. He should not engage in traumatic sports.
- You should choose your toothbrush carefully - it should be soft.
- In some cases, it is advisable to take laxatives to avoid intestinal trauma.
- Do not use medications that increase bleeding ( Aspirin ).
- Provide hospitalization of the child in case of bleeding, in the presence of severe hemorrhages in the mucous membranes and skin.
Parents should be aware that the most serious complication of thrombocytopenia is cerebral hemorrhage. It develops if the platelet count is 10-20 thousand per microliter. Symptoms that should be alarming are a sharp bursting headache , convulsions , vomiting, and facial asymmetry. If such signs occur, you should immediately call an ambulance. However, such complications rarely develop.
Thrombocytopenia during pregnancy
Pregnant women may experience a decrease in platelet counts and hemocoagulation changes. Thrombocytopenia during pregnancy can be a consequence of both physiological and pathological processes. Normally, in most expectant mothers, the platelet count decreases by 10% compared to normal levels. The most significant decrease in platelets during pregnancy is observed in the last trimester.
If severe thrombocytopenia develops, this is manifested by a loss of strength and the formation of hematomas on the skin and mucous membranes.
Specific conditions associated with pregnancy are:
- Gestational thrombocytopenia - the platelet count may decrease to 43x109/L. Develops at the end of the second to the beginning of the third trimester. It is a physiological condition that does not complicate pregnancy.
- Thrombocytopenia in a hypertensive state – these conditions include preeclampsia and HELLP syndrome. These conditions require treatment, as they threaten the normal course of pregnancy.
To prevent complications, a pregnant woman should regularly take blood tests, eat right and follow all doctor’s recommendations.
How dangerous is the disease and who is at risk?
The causes of the disease depend on the pathological processes occurring in the body:
- Platelet deficiency in the bone marrow. It is observed in aplastic and megablastic anemia, metastasis of malignant tumors into the body of the red brain, acute and chronic leukemia, and viral invasion. It can be a consequence of taking medications and a course of radiation therapy.
- Massive bleeding or increased platelet destruction.
- Impaired distribution of platelets or their excessive deposition.
- Excessive rate of destruction of blood plaques and attenuation of compensatory mechanisms.
- Anomalies in the development of the skeletal system.
The mechanics of the development of the disease are identical for all cases - the concentration of platelets decreases, which provokes disturbances in the nutrition of the capillary walls, and this leads to their excessive fragility.
The result is spontaneous or traumatic bleeding due to rupture of small vessels. Since the platelet count is low, a platelet plug does not appear inside the damaged vessel, and this causes a massive release of blood outside the vessel into the surrounding tissue.
The greatest danger for the patient is the fact that a decrease in platelets to 100x10 in 9 g/l is asymptomatic (at a normal level of 180-320x10 in 9 g/l). A person feels quite comfortable, but at the same time life-threatening conditions, for example, anemia, are already developing in his body.
The prognosis for the outcome of the disease is determined by several factors:
- severity of clinical symptoms and duration of the disease;
- presence of complications;
- timeliness and correctness of treatment;
- the severity of the underlying disease.
All patients undergoing treatment for thrombocytopenia should undergo a complete blood count every 6 months for preventive purposes.
Thrombocytopenia is insidious with sudden relapses. Against the background of complete well-being, a sharp drop in platelets is possible. This is mainly characteristic of thrombocytopenia in blood diseases. Such patients, in addition to laboratory monitoring, require self-monitoring. Even slight bleeding of the gums should alert you. In this case, you do not need to undergo a scheduled examination; you must immediately make an appointment.
Diet
Diet for essential thrombocythemia
- Efficacy: therapeutic effect after 3 weeks
- Timing: constantly
- Cost of products: 1400-1500 rubles per week
People who have a low platelet count in their blood should follow some recommendations when shaping their diet.
- You need to eat meals in small portions, doing this at least 5 times a day.
- The diet should contain protein foods that are easily digestible (liver, poultry, fish).
- It is important to get proteins from plant foods, consuming legumes, nuts, and mushrooms.
- It is recommended to include more fresh vegetables and fruits in the menu. It is better to choose seasonal fruits and steam, boil, or bake vegetables.
- Low-fat dairy products should also be included in your diet every day.
- It is recommended to cook porridge in water from whole grains - buckwheat, rice, wheat.
- It is better to choose bread with bran.
- You should drink weak tea, dried fruit compote, berry fruit drinks, cocoa, and fresh juices.
- You can make an omelet from quail eggs.