Comparison of the effectiveness of Galvus and Vipidia
The effectiveness of Galvus is quite similar to Vipidia - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Galvus is more pronounced, then using Vipidia even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Galvus and Vipidia. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Galvus, Ongliza, Januvia
One of the recommendations that emerged from the consultation was that clinicians should reconsider the use of DPP-4 inhibitors in the management of type 2 diabetes in older adults with hba1c levels <8.5% due to sparse data on clinically significant benefits of their use . https://www.ncbi.nlm.nih.gov/pubmed/29047372
Experimentally, DPP-4 inhibitors may enhance the ability of glucagon-like peptide-1 to stimulate cyclic adenosine monophosphate in cardiomyocytes, and potentiation of the effects of stromal cell factor-1 by DPP-4 inhibitors may exacerbate cardiac fibrosis . These potentially negative effects of DPP-4 inhibitors may not become clinically clear unless these drugs increase sodium excretion. However, the natriuretic effect of DPP-4 inhibitors is modest because they act on the distal (rather than proximal) renal tubules. Accordingly, both clinical trials and observational studies have reported an increased risk of heart failure in patients with type 2 diabetes mellitus treated with DPP inhibitors -4. This risk may be muted in trials with a high prevalence of metformin use or with a low and declining background use of insulin and thiozolidinediones. The most vulnerable patients (ie those with known heart failure) were not well represented in these studies. The only study that specifically evaluated patients with pre-existing left ventricular dysfunction observed critical structural and clinical effects associated with the drug. The increased risk of worsening heart failure appears to be a class effect of DPP-4 inhibitors, even in patients without a history of heart failure.
https://www.ncbi.nlm.nih.gov/pubmed/29525332
A study that directly compared the drugs under identical experimental conditions found that all five inhibitors demonstrated similar potency (i.e., maximum effect) at inhibiting DPP-4 in vitro, but there were differences in potency (i.e., amount required to inhibit the compound IC50 = ~1 nmol for linagliptin vs. 19, 62, 50 and 24 nmol for sitagliptin, vildagliptin, saxagliptin and alogliptin, respectively). Differences were also noted regarding the half-life of the drugs. Vildagliptin and saxagliptin are cleared from plasma relatively quickly, whereas sitagliptin, alogliptin and linagliptin have a longer shelf life. These differences are reflected in therapeutic doses (which range from 5 mg for saxagliptin and linagliptin to 100 mg for sitagliptin) as well as dosing frequency (once daily for most, twice daily for vildagliptin).
Although dipeptidyl peptidase (DPP)-4 inhibitors have been reported to have a neutral effect on thromboembolic vascular-occlusive events in large-scale trials, they act on the potential of several endogenous peptides that may cause cardiovascular effects .
DPP-4 inhibitors cause accelerated gastric emptying, thereby contributing to B12 deficiency anemia. It is proposed to use them in dosage forms that are absorbed in the oral cavity.
DPP-4 inhibitors cause pancreatitis.
Their effect on heart failure and systolic dysfunction has been noted, especially saxagliptin (Ongliza) and alogliptin (Vipidia), sitagliptin (Januvia) increases the risk of re-hospitalization for systolic dysfunction.
Galvus Vildagliptin
Clinical trials have identified peripheral edema as an adverse effect of vildagliptin https://www.ncbi.nlm.nih.gov/pubmed/27534752
The incidence of angioedema during treatment with Galvus was ≥1/10,000, <1/1000 (rare) and was similar to that in the control group. The most common cases of angioedema were observed when using the drug in combination with ACE inhibitors . In most cases, angioedema was of moderate severity and resolved spontaneously with continued therapy with vildagliptin.
Liver dysfunction has rarely been reported during therapy with Galvus . In most cases, these disorders and deviations of liver function tests from normal resolved independently without complications after discontinuation of drug therapy. When using Galvus at a dose of 50 mg 1 time/day or 2 times/day, the frequency of increases in liver enzyme activity (ALT or AST ≥3×ULN) was 0.2% or 0.3%, respectively (compared to 0.2% in the control group). The increase in liver enzyme activity was in most cases asymptomatic, did not progress, and was not accompanied by cholestasis or jaundice.
Even during the period of registration of vildagliptin, a meta-analysis of clinical data revealed that a single dose of 100 mg of the drug was associated with a slight increase in the level of liver transaminases compared to placebo and a dose of vildagliptin 50 mg when taken twice. For this reason, the recommended therapeutic dose was changed to 50 mg twice a day, and this was accompanied by recommendations for the need to monitor liver function before starting treatment, every 3 months for the first year, and periodically thereafter. Subsequently, the trend toward modest increases (more than three times the ULN) in liver enzymes was confirmed in the larger pooled safety analysis, but this was not associated with an increase in the incidence of true liver adverse events. However, evaluation of liver function tests is still recommended when using vildagliptin and the drug is not approved for use in patients with liver impairment.
Ongliza Saxagliptin
Prescriptions of saxagliptin have been associated with an increased risk or hospitalization for heart failure. https://www.ncbi.nlm.nih.gov/pubmed/31161099
This increase in risk was greatest among patients
- with increased levels of natriuretic peptide,
- previous heart failure
- chronic kidney disease, glomerular filtration rate ≤60 ml/min
https://www.ncbi.nlm.nih.gov/pubmed/25189213
Saxagliptin neither increased nor decreased cerebrovascular risk compared with placebo as assessed by the risk of death from a cerebrovascular cause, nonfatal myocardial infarction, or nonfatal stroke. Unexpectedly, more patients in the saxagliptin group (3.5%) than in the placebo group (2.8%) were hospitalized for heart failure .
https://www.ncbi.nlm.nih.gov/pubmed/26578430
Saxagliptin increases the risk of hospitalization for heart failure in the general population https://www.ncbi.nlm.nih.gov/pubmed/25758769
Several studies have reported a small, reversible, dose-dependent reduction in absolute lymphocyte counts with saxagliptin.
Januvia sitagliptin
Compared with sitagliptin therapy, saxagliptin, linagliptin, and gemigliptin therapy were associated with a lower risk of cardiovascular events . https://www.ncbi.nlm.nih.gov/pubmed/29671284
An analysis of clinical studies of the drug showed a slight increase in uric acid (approximately 0.2 mg/dL compared to placebo, average level 5-5.5 mg/dL) in patients receiving JANUVIA at a dose of 100 and 200 mg per day. No cases of gout were reported. There was a slight increase in white blood cell count (approximately 200/μL compared with placebo, mean 6600/μL), due to an increase in neutrophil counts.
Comparison of safety of Galvus and Vipidia
The safety of a drug includes many factors.
At the same time, Galvus’s is higher than Vipidia’s. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Galvus, as well as Vipidia, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Galvus has fewer risks when used than Vipidia.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of using Galvus and Vipidia.
Galvus Met®
In patients receiving insulin treatment, Galvus Met® cannot replace insulin therapy. Galvus Met® should not be used to treat type 1 diabetes or diabetic ketoacidosis.
Vildagliptin
Liver dysfunction
The use of the combination drug vildagliptin + metformin is not recommended for patients with clinical or laboratory signs of liver dysfunction, including patients with an increase in ALT or AST >3 x ULN before treatment.
Rare cases of liver dysfunction (including hepatitis) have been reported with the use of vildagliptin. These cases were usually asymptomatic, without clinical consequences, and after discontinuation of therapy, liver function tests returned to normal. Liver function should be examined before starting therapy with the combination drug vildagliptin + metformin, then monitored once every 3 months during the first year of use of the drug, and then periodically. If an increase in aminotransferase activity is detected, a re-examination should be carried out to confirm the result, and then biochemical indicators of liver function should be regularly determined until they normalize. If an excess of AST or ALT activity of 3 or more times the ULN is confirmed upon re-examination, the use of the drug should be discontinued. If jaundice or other signs of liver dysfunction develop while using the vildagliptin + metformin combination, therapy should be discontinued immediately. After normalization of liver function indicators, treatment with the drug cannot be resumed.
Metformin
Lactic acidosis
Lactic acidosis is a very rare but severe metabolic complication, most often occurring with a sharp deterioration in renal function, as well as with cardiorespiratory syndromes and sepsis. With a sharp deterioration in kidney function, metformin accumulates in the body, which increases the risk of developing lactic acidosis.
If dehydration occurs (eg, associated with severe diarrhea or vomiting, fever, or decreased fluid intake), a patient taking metformin-containing medications (eg, Galvus Met®) should immediately stop taking the above medications and seek medical attention.
In patients taking drugs containing metformin (for example, Galvus Met®), caution should be exercised when initiating therapy with drugs that can acutely worsen renal function (for example, antihypertensive drugs, diuretics, NSAIDs). Other risk factors include: alcohol abuse, liver dysfunction, inadequately controlled diabetes mellitus, ketoacidosis, prolonged fasting, conditions associated with hypoxia, and concomitant use of drugs that can cause lactic acidosis.
Diagnosis of lactic acidosis
The patient and/or caregivers should be informed of the risk of developing lactic acidosis. Lactic acidosis is characterized by acidotic dyspnea, abdominal pain, muscle cramps, asthenia and hypothermia followed by coma. If symptoms develop that suggest the development of lactic acidosis, the patient should stop taking metformin-containing drugs (for example, Galvus Met®) and immediately seek medical help. Laboratory and instrumental examination data: decreased blood pH (<7.35), increased lactate concentration in the blood serum >5 mmol/l, as well as an increased anion gap and an increase in the lactate/pyruvate ratio. If lactic acidosis is suspected, therapy with metformin-containing drugs should be stopped and the patient should be hospitalized immediately.
Monitoring kidney function
Before starting therapy, GFR should be determined, and this indicator should be monitored periodically during drug therapy. The use of metformin-containing drugs (such as Galvus Met®) is contraindicated in patients with GFR <30 ml/min; in the presence of conditions that can impair renal function, the use of the above drugs should be temporarily suspended.
Since metformin is largely eliminated by the kidneys, the risk of accumulation and development of lactic acidosis increases with the severity of renal impairment. Because older age may be associated with deterioration of renal function, in patients in this category the dose of metformin-containing drugs (such as Galvus Met®) should be carefully adjusted to select the minimum dose that provides adequate glycemic effect, with regular monitoring of renal function.
Interactions
Concomitant use of medications that affect renal function or the distribution of metformin
Caution should be exercised when used concomitantly with drugs that can affect renal function, have significant hemodynamic effects or affect the distribution of metformin in the body, such as organic cations excreted by the kidneys by tubular secretion.
The use of iodine-containing radiocontrast agents for intravascular administration
Intravenous administration of radiopaque iodine-containing agents can provoke the development of contrast-induced nephropathy, leading to the accumulation of metformin in the body and increasing the risk of developing lactic acidosis. Metformin-containing medications (such as Galvus Met®) should be temporarily discontinued before or during the procedure; Dosage should be resumed no earlier than 48 hours after the procedure, after receiving laboratory confirmation of stabilization of renal function.
Alcohol consumption
It has been established that ethanol enhances the effect of metformin on lactate metabolism. The patient should be warned not to abuse alcohol while using metformin-containing drugs (such as Galvus Met®).
Alcohol intoxication is associated with an increased risk of lactic acidosis, especially with prolonged fasting, malnutrition and impaired liver function.
Vitamin B12 content
It has been established that metformin causes an asymptomatic decrease in the concentration of vitamin B12 in the blood serum in approximately 7% of cases. Such a decrease in very rare cases leads to the development of anemia. After discontinuation of metformin and/or vitamin B12 replacement therapy, serum concentrations of vitamin B12 quickly normalize. In patients receiving metformin-containing drugs (such as Galvus Met®), general clinical blood test parameters should be monitored at least once a year. If deviations of hematological parameters from the norm are detected, the etiology of such disorders should be clarified and appropriate treatment should be carried out. Some patients (eg, patients with insufficient intake or malabsorption of vitamin B12 or calcium) are predisposed to decreased serum concentrations of vitamin B12. In such patients, determining the concentration of vitamin B12 in the blood serum at least once every 2-3 years can have diagnostic value.
Hypoxia
Cardiovascular collapse (shock), acute heart failure, acute myocardial infarction, and other conditions characterized by hypoxemia are associated with lactic acidosis and may also contribute to prerenal azotemia. If the above conditions occur, the use of metformin-containing drugs (such as Galvus Met®) should be stopped immediately.
Surgical interventions
During surgical procedures under general, spinal or epidural anesthesia (except for minor operations not associated with restriction of food and fluid intake), the use of metformin-containing drugs (such as Galvus Met®) should be discontinued.
Resumption of the drug is possible no earlier than 48 hours after the intervention or after the restoration of oral food intake after receiving laboratory confirmation of stabilization of renal function.
Patients with liver dysfunction
Since lactic acidosis, which is one of the HPs of metformin, has been reported in some cases in patients with impaired liver function, the combination drug vildagliptin + metformin should not be used in patients with liver disease or impaired biochemical parameters of liver function.
Deterioration of the condition of patients with type 2 diabetes who previously responded to therapy
If a deviation in laboratory parameters from the norm is detected or clinical symptoms of a deterioration in the general condition appear (especially when symptoms are not clearly expressed and blurred) in patients with a previous adequate response to therapy, laboratory diagnostics should be immediately carried out to identify ketoacidosis and/or lactic acidosis. If acidosis is detected, you should immediately stop using the drug and take the necessary measures to correct the patient’s condition.
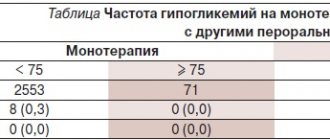
Hypoglycemia
As a rule, hypoglycemia is not observed in patients receiving therapy only with the combination drug vildagliptin + metformin, but it can occur against the background of a low-calorie diet (when intense physical activity is not compensated for by the caloric content of food), or against the background of alcohol consumption. The development of hypoglycemia is most likely in elderly, weakened or malnourished patients, as well as against the background of hypopituitarism, adrenal insufficiency or alcohol intoxication. In elderly patients and in those receiving beta-blockers, the diagnosis of hypoglycemia may be difficult.
Reduced effectiveness of hypoglycemic drugs
In case of stress (fever, injury, infection, surgery, etc.) that develops in patients receiving hypoglycemic drugs according to the standard regimen, a sharp decrease in the effectiveness of the latter for some time is possible. In this case, it may be necessary to temporarily discontinue therapy with the vildagliptin + metformin combination and transfer to insulin therapy. Resumption of treatment with Galvus Met® is possible after the end of the acute period.
Fertility
There have been no studies of the effect of the combination drug vildagliptin + metformin on fertility in humans. In animal studies, vildagliptin at doses 200 times higher than recommended did not cause fertility problems.
There were no adverse effects on fertility in males or females when metformin was administered at doses of 600 mg/kg per day, which is approximately 3 times the recommended human dose (based on body surface area).
Comparison of habituation in Galvus and Vipidia
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
Thus, the totality of the values of such parameters as “o syndrome” in Galvus is quite similar to the similar values in Vipidia. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible. At the same time, in Galvus the meaning of the “syndrome” is quite small, however, the same as in Vipidia.
Comparison of side effects of Galvus and Vipidia
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Vipidia has more adverse events than Galvus. This implies that the frequency of their occurrence is low in Vipidia and low in Galvus. Frequency of manifestation is an indicator of how many cases of an undesirable effect from treatment are possible and registered. The undesirable effect on the body, the strength of influence and the toxic effect of drugs are different: how quickly the body recovers after taking it and whether it recovers at all. When using Vipidia, the body's ability to recover faster is higher than that of Galvus.
Galvus
Hypoglycemic agent, stimulator of the islet apparatus of the pancreas, selective inhibitor of the enzyme dipeptidyl peptidase-4 (DPP-4).
Rapid and complete inhibition of DPP-4 activity (more than 90%) causes an increase in both basal and stimulated (food intake) secretion of glucagon-like peptide type 1 and glucose-dependent insulinotropic polypeptide from the intestine into the systemic circulation throughout the day.
By increasing the concentrations of glucagon-like peptide type 1 and glucose-dependent insulinotropic polypeptide, it causes an increase in the sensitivity of pancreatic beta cells to glucose, which leads to an improvement in glucose-dependent insulin secretion.
When using the drug at a dose of 50-100 mg per day in patients with type 2 diabetes mellitus, an improvement in the function of pancreatic beta cells is noted.
The degree of improvement in pancreatic islet beta cell function depends on the degree of initial damage; Thus, in persons without diabetes mellitus (with normal plasma glucose concentrations), the drug does not stimulate insulin secretion and does not reduce glucose concentrations.
By increasing the concentration of endogenous glucagon-like peptide type 1, it increases the sensitivity of alpha cells of the pancreatic islets to glucose, which leads to improved glucose-dependent regulation of glucagon secretion.
The decrease in the concentration of excess glucagon during meals, in turn, causes a decrease in insulin resistance.
An increase in the insulin/glucagon ratio against the background of hyperglycemia, caused by an increase in the concentration of glucagon-like peptide type 1 and glucose-dependent insulinotropic polypeptide, causes a decrease in the production of glucose by the liver (during the prandial period and after meals), which leads to a decrease in the concentration of glucose in the blood plasma.
With the use of the drug, a decrease in the concentration of lipids in the blood plasma is observed, but this effect is not associated with its effect on glucagon-like peptide type 1 or glucose-dependent insulinotropic polypeptide and improvement in the function of pancreatic beta cells.
An increase in the concentration of type 1 glucagon-like peptide can lead to a slower gastric emptying, but no such effect is observed with the use of the drug.
When using the drug as monotherapy or in combination with metformin, sulfonylurea derivatives, thiazolidinedione, or insulin, a significant long-term decrease in the concentration of glycosylated Hb and fasting blood glucose is observed.
Comparison of ease of use of Galvus and Vipidia
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Galvus is approximately the same as Vipidia. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-04 13:43:17