Hemorrhoids – literally translated from Greek as “bleeding” – are the most common proctological disease associated with hypertrophy and varicose veins of the rectum with the formation of hemorrhoids and the risk of bleeding.
Hemorrhoids occur with equal probability in men and women; they affect about 120-145 people out of 1000, that is, about 25% of the adult population. In the structure of proctological morbidity, it occupies 43%.
Hemorrhoids can be acute or chronic, external, internal or combined (depending on the location of the hemorrhoids), primary or secondary (as a complication of other diseases and conditions), complicated or not.
Causes of hemorrhoids
The appearance of hemorrhoids is associated with congenital insufficiency of the development of veins or venous stasis, varicose veins of the rectum that develop during life.
Risk factors for developing hemorrhoids:
- sedentary lifestyle;
- age from 35 to 55 years;
- sedentary or standing work;
- heavy physical labor, pregnancy and childbirth, causing an increase in intra-abdominal pressure;
- constipation and diarrhea;
- congenital venous insufficiency (weakness of the vascular wall and venous valves of the rectal veins);
- chronic heart failure;
- stagnation in the systemic circulation;
- chronic pelvic inflammation;
- portal hypertension;
- pelvic neoplasms (bacterial salpingoophoritis, prostatitis or cystitis);
- alcoholism;
- errors in nutrition (spicy foods, lack of fluid, lack of fiber, overeating);
- intoxication of various origins (including anabolic steroids, contraceptives, chemotherapy, long-term use of psychotropic drugs).
In the rectal area there are cavernous veins connected by anastomoses to the arteries of the rectum.
These plexuses ensure the retention of feces by the rectum and defecation itself, and participate in the rectal immune barrier. Disruption of venous outflow and increased arterial inflow lead to stagnation of blood in the pelvis, overstretching of the vein wall with the formation of nodes. The trophism of the longitudinal muscle of the submucosal rectum decreases and, as a result, a fibromuscular framework of the hemorrhoidal node is formed, displacing it from the anal canal externally or into the intestinal lumen. At first, they fall out and correct themselves when straining, then they require manual reduction, and in severe cases, surgical treatment.
The scarlet color of arterial blood during hemorrhoidal bleeding is explained by the presence of anastomoses between varicose cavernous veins and rectal arteries.
Causes of hemorrhoids in women
Hemorrhoids often occur in pregnant women
With minor differences, the causes of the disease are similar to those in men:
- Inactive lifestyle. Office work leaves its mark on the health of almost all organ systems, and even more so the pelvic organs. The accumulation of blood in the intestinal vessels due to the impossibility of its outflow provokes swelling of the veins and the formation of nodules.
- Excessive athletic activity and heavy lifting. In the age of feminism, women have the opportunity, on an equal basis with men, to work physically, compete in sports competitions (for example, weightlifting and wrestling), and also simply train in the gym (and often ineptly and dangerously).
- Unbalanced diet. The abundance of flour, spicy and peppery foods provokes disruptions in the intestines, which can lead to constipation or diarrhea. Both extremes contribute to the appearance of hemorrhoids.
- Hereditary predisposition.
- Bearing a child and giving birth. Anatomically, the uterus is located close to the large intestine, which contributes to compression of the latter. This leads to two consequences - accumulation and slow outflow of blood from the intestines and a banal mechanical obstacle to the passage of feces. Therefore, you have to push a lot during bowel movements, provoking the occurrence of hemorrhoids. The process of childbirth occupies a special place. The colossal tension that is created during the expulsion of the fetus often leads to the pathology mentioned above.
- Menses. Increased blood flow, uterine contractions and decreased motor activity contribute to the overflow of venous collections. This is especially true for a girl’s first cycle in her life.
- Intensive use of laxatives for weight loss.
- Increased body weight (accumulation of adipose tissue in the upper body due to hormonal obesity).
- Age-related changes associated with loss of elasticity of vascular and intestinal muscles, and increased body weight.
- Passion for anal sex.
- Psycho-emotional stress.
Symptoms of hemorrhoids
- Constipation.
- Pain in the anus.
- Burning and itching around the anus.
- Maceration of the skin of the perianal area.
- Sphincter weakness.
- Mucous discharge from the rectum.
- Hemorrhoids are painful brown lumps that periodically appear in the anus at the entrance to the rectum or externally during defecation or other straining.
- Discharge of scarlet blood from the anus.
Acute hemorrhoids are characterized by:
- severe pain;
- bleeding from the anus that is difficult to stop.
Chronic hemorrhoids are accompanied by:
- infrequent and less intense pain;
- spotting, scanty, but constant bloody discharge.
Additional signs of hemorrhoids (not always included in the clinical picture):
- weakness, dizziness;
- dyspnea;
- depression;
- sensation of a foreign body and incomplete emptying.
Clinical signs of hemorrhoids
At the first symptoms you should consult a doctor
Symptoms directly correlate with the stage of development of the disease, and also depend on the individual characteristics of the body, for example, the ability to clot blood.
In any case, the disease does not occur suddenly, but develops over several days, initially manifesting itself as burning and pain during bowel movements, itching, mucus secretion, sensation of a foreign object in the intestine and swelling of the rectal area.
Stages (degrees) of hemorrhoids
I degree:
- acute hemorrhoids: painful, tight-elastic small nodules in the anal area;
- chronic hemorrhoids: occasional bleeding without prolapse of hemorrhoids.
II degree:
- acute hemorrhoids: increased pain; compaction and enlargement of hemorrhoids, capable of prolapse and self-reduction into the intestinal lumen; redness of the skin around the anus; anal sphincter spasm;
- chronic hemorrhoids: prolapse and self-reduction of hemorrhoids, sometimes with bleeding from the rectum. The prolapse of nodes into the intestinal lumen or externally is provoked by straining.
III degree:
- acute hemorrhoids: inflammation and hyperemia spread to surrounding tissues; pain intensifies; around the anus - unreducible purple-bluish, dense, thrombosed painful nodes with foci of necrosis; risk of significant bleeding;
- chronic hemorrhoids: hemorrhoids periodically prolapse into the intestinal lumen or externally, and are reduced manually.
IV degree – chronic hemorrhoids: hemorrhoids fall out and cannot be reduced on their own.
At stages 3 and 4, the weak, thin longitudinal muscle cannot contract normally, so independent reduction of the node is impossible. If you do not manually adjust it in a timely manner, complications such as paraproctitis, fever, bleeding, and anal fissures develop.
Symptoms of the acute form of the disease
Symptoms of acute hemorrhoids in young women are most often associated with pregnancy or childbirth. The appearance of an enlarged hemorrhoid constipation characteristic of this period .
Acute dilatation of hemorrhoidal veins manifests itself with sharp pain , which becomes unbearable during bowel movements. In addition, the pain syndrome can intensify while walking, as well as with increased intra-abdominal pressure during straining, coughing, laughing, and hiccups.
Another characteristic sign of the acute form of the disease is bleeding from the dilated veins of the rectum. This symptom manifests itself as fresh blood on the surface of the stool.
Often hemorrhoids in women are combined with anal fissure. In such cases, blood stains on toilet paper and underwear appear even more often after defecation.
Complications of hemorrhoids
- Paraproctitis (inflammation of the tissues around the rectum).
- Anal fissures.
- Hemorrhoidal bleeding.
- Thrombosis of the pelvic veins.
- Incarceration of the hemorrhoidal node.
Bleeding with hemorrhoids can be regarded as one of the most important symptoms, and as a life-threatening condition, depending on the amount of blood loss.
Minor bleeding during bowel movements appears as scarlet drops, usually not mixed with feces. They lead to the development of anemia only in 2% of cases, but they cause anxiety to the patient and require planned treatment by a proctologist. Profuse hemorrhoidal bleeding is life-threatening when the vascular wall of the hemorrhoidal node ruptures. Heavy bleeding from the anus with scarlet blood is accompanied by weakness, dizziness, sticky cold sweat, increased breathing, tachycardia and a weak pulse. These are grounds for an emergency call to emergency medical services.
While waiting for the team to arrive, the patient should be placed with his legs elevated and a cold pack placed on the anus. The patient requires emergency hospitalization.
Treatment during pregnancy and after childbirth
Treatment of hemorrhoids in pregnant women and in the early postpartum period does not involve surgical intervention. The fact is that the reasons for the dilation of the veins of the rectum during this period are physiological in nature: • changes in hormonal levels; • increased intra-abdominal pressure; • increase in circulating blood volume; • straining during childbirth.
After childbirth, hormonal levels gradually normalize, which leads to the disappearance of the tendency to constipation. The volume of circulating blood decreases, intra-abdominal pressure decreases, the body's defenses are restored and all conditions for recovery are created.
Therefore, in most cases, a painful node that occurs during pregnancy or after childbirth disappears on its own under the influence of standard methods of conservative treatment.
Attention! When conservatively treating hemorrhoids in pregnant women, as well as in women during lactation, care should be taken. Some active ingredients of topically applied drugs still enter the bloodstream and can harm the child. Therefore, treatment must be done under the supervision of a physician.
Diagnosis of hemorrhoids
Diagnosis begins with collecting anamnesis, clarifying complaints and examination by a proctologist.
The patient is positioned in a gynecological chair with his legs adducted, knee-elbow position, and less often - on his side. A physical examination by a proctologist includes:
- digital examination of the rectum;
- anoscopy (to examine the walls of the anal canal and distal rectum);
- sphincterometry (for chronic hemorrhoids - weakness, and for acute hemorrhoids - sphincter spasm);
- colonoscopy (for differential diagnosis);
- sigmoidoscopy (diagnosis of concomitant diseases of the colon);
- X-ray of the large intestine with barium (enema).
Endoscopic examinations are performed under anesthesia, in some cases under general anesthesia.
Classification of phlebotonic drugs
Modern tablets allow you to treat external hemorrhoids and relieve pronounced symptoms of the disease at any stage. According to clinical trials and patient reviews, the most effective means in the fight against anal varicose veins are:
- Phlebodia is a new generation drug based on plant components of bioflavonoids. The active ingredient diosmin has a venotonic, angioprotective effect on venous vessels, increases lymphatic drainage, strengthens the walls of veins and reduces their permeability. Tablets are indicated for acute and chronic forms of the disease. Contraindications: allergy to the components of the tablet, age under 18 years, 1st trimester of pregnancy and lactation period.
- Detralex is a tablet based on diosmin and hesperidone, which has a complex effect in several directions at once: increasing venous tone, eliminating blood stagnation, normalizing microcirculation of lymph and blood, as well as giving elasticity to blood vessels. Indications: exacerbation of external hemorrhoids, varicose veins of the lower extremities, general prevention of venous insufficiency.
- Venarus – hesperidin and diosmin in tablets. It has the same effects as previous medications. With regular use, it helps to normalize blood flow in the pelvic organs, maintains the elasticity and reliability of the venous wall, and eliminates blood stagnation. Tablets are effective in complex treatment of the problem.
- Vazonit is a medicine based on the active substance pentoxifylline. Helps normalize microcirculation of the venous vessels of the rectum and anus, improves oxygen supply to tissues. The tablets reduce the risk of blood clots in external hemorrhoids, which minimizes the risk of complications. Dispensed with a doctor's prescription.
Prevention of hemorrhoids
Preventive measures should be carried out both by people with risk factors for the development of hemorrhoids, and by those who have already begun treatment for this disease:
- physical activity: walking, fitness programs without straining, swimming, exercise therapy;
- compliance with the work and rest schedule, for example, organizing food points on the highway for drivers, “physical education” for office employees, sometimes even a temporary change of job;
- compliance with the principles of ergonomics of the work process and labor protection rules;
- a diet that includes a sufficient amount of liquid and plant fiber;
- prevention and treatment of constipation;
- careful hygiene of the anus and perineum.
In this way, it is possible to prevent exacerbation and aggravation of the severity of the disease.
Minimally invasive methods
Mechanism of action of low-traumatic interventions
Minimally invasive (low-traumatic) treatment methods involve the removal of hemorrhoids without the use of a traditional surgical scalpel. Such procedures are well tolerated by patients, so they are often called the treatment of hemorrhoids without surgery. ___1. Sclerotherapy of hemorrhoids is the introduction of a chemical substance into the lumen of the vessel feeding the node, which burns the inner lining of the vessel. As a result, the pathological element decreases in size. ___2. During coagulation of hemorrhoids, “gluing” of the internal walls of the vein feeding the node occurs under the thermal influence of wave radiation. ___3. Ligation of nodes with latex rings is a mechanical ligation of the feeding arteries.
Thus, the mechanism of action of minimally invasive methods is the same: the pathological element is “disconnected” from the vascular network, becomes necrosis and is excreted from the body with feces.
Advantages and disadvantages of low-impact methods
The advantages of low-traumatic methods of treating hemorrhoids are expressed in the name itself. An injury that is insignificant to the body does not impose increased demands on the patient’s health, so such treatment can be carried out even in old age in patients aggravated by many chronic diseases.
In addition, minimally invasive intervention assumes: ___• outpatient nature (does not require hospitalization), ___• a short recovery period with minor restrictions (prohibition of physical activity and thermal procedures), ___• mild postoperative pain syndrome, easily relieved with standard painkillers.
Minimally invasive methods have one single, but serious drawback : they are not effective for all patients. At stages IV and V of the development of the process (unremovable nodes), as well as in cases of complicated hemorrhoids, it is necessary to resort to traditional surgery to remove hemorrhoids
Treatment of hemorrhoids
If the patient consults a proctologist in a timely manner, then at stages 1 and 2 of the disease, conservative treatment is used to relieve pain, itching and bleeding, and then influence the causes of the disease.
Drugs and a diet are prescribed to thin the stool; for pain, a pararectal novocaine blockade is used. The diet for hemorrhoids includes fluid intake (from 2 liters per day), the use of food bran, seaweed, flaxseed and plantain seed in the diet. Diet therapy is used in combination with other treatment methods and does not provide an independent clinical effect.
Various dosage forms are used to treat hemorrhoids.
For local treatment, rectal gels, ointments and suppositories for hemorrhoids are prescribed: for example, Ultraproct, fluocortolone, Relief.
Hemostatic sponges and suppositories: spongostan, collagen hemostatic sponges based on fibrinogen and thrombin, suppositories and ointments with heparin, phenylephrine, belladonna extract.
Tablet preparations are aimed at preventing constipation, increasing venous tone and stimulating blood and lymph flow, restoring microcirculation, and fighting inflammation.
For constipation, enzymes, laxatives with emollient and osmotic effects are prescribed: psyllium preparations, lactulose and macrogol.
Angioprotectors and phlebotropic drugs are recommended to normalize hemodynamics and restore microcirculation. Among the anti-inflammatory drugs used are drugs from the group of non-steroidal anti-inflammatory drugs, although in severe cases hormonal drugs (fluocortolone) are also used.
For thrombosis of hemorrhoids, bioflavonoids are recommended; to reduce the risk of bleeding - purified microgenized flavonoid fraction (diosmin + flavonoids in terms of hesperidin) (MOFF).
Minimally invasive interventions for hemorrhoids
Minimally invasive methods of surgical treatment of hemorrhoids are used on an outpatient basis and do not require general anesthesia, a long period of rehabilitation and pain relief in the postoperative period. These include sclerosis or alloying of hemorrhoids with latex rings, desarterization of the terminal branches of the superior hemorrhoidal artery, and infrared laser photocoagulation.
Surgery for hemorrhoids
At stage III, in advanced cases, surgical treatment of hemorrhoids under general anesthesia is used - removal of the node (hemorrhoidectomy).
Preparation for surgery includes:
- 2 days of a slag-free diet;
- an enema the day before and before surgery or taking Fortrans 1 glass every quarter of an hour;
- in some cases - antibiotics.
The postoperative period includes dressings and a slag-free diet.
The first stool occurs after 5-7 days and may be painful with some bleeding. Hemorrhoids are a serious proctological disease that reduces the quality of life and can, in some cases, pose an immediate threat. The risks of developing complications increase when visiting a proctologist late.
At stages 1 and 2, properly selected treatment can solve the problem or lead to long-term remission, but fear of a proctological examination and a false sense of shame prevent patients from seeking help.
At stages 3 and 4, the intervention of a proctologist-surgeon is required; this requires more time and causes additional discomfort. The arsenal of modern coloproctology has sufficient means for treating hemorrhoids in the early stages, which increases the quality and level of safety of life for a person who is familiar with this common unpleasant disease firsthand.
Radical treatment of pathology
Minimally invasive methods
Doctors treat chronic hemorrhoids with surgical methods. At the initial stages of the disease, preference is given to minimally invasive techniques, which are carried out on an outpatient basis (without placing the patient in a hospital) and provide for a short rehabilitation period.
An important advantage of low-traumatic operations is a short list of contraindications. The list of methods that are suitable for most patients includes: • sclerotherapy (injection into dilated veins of substances that cause “soldering” of the walls of dilated veins); • infrared coagulation (cauterization of the leg of the node); • ligation of the internal hemorrhoid with latex rings.
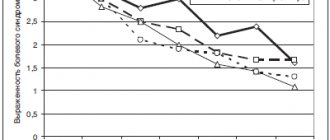
Sclerotherapy and infrared coagulation are used at stages I – II of the development of internal hemorrhoids. The effectiveness of these methods at stage I is 85%, and at stage II – about 72%. If the node is ligated with latex rings, the effectiveness exceeds 93%.
Operation hemorrhoidectomy
Hemorrhoidectomy is the removal of enlarged hemorrhoids using surgical methods, that is, using a scalpel.
Such treatment must be carried out in a hospital. The rehabilitation period is much longer and is less well tolerated by patients. Therefore, surgical removal of nodes is carried out only in the last stages of the disease , when minimally invasive techniques are no longer effective.
Hemorrhoidectomy can be combined with disarterization of hemorrhoids under ultrasound control. This method is often used for stage III internal hemorrhoids.
The choice of surgical intervention method depends on the number of enlarged nodes, their location, as well as the presence of complications and concomitant pathologies.
Bibliography
- Vovk, E.I. Hemorrhoids: emergency care, treatment strategy, prevention / E.I. Vovk. - Text: electronic // Russian Medical Journal, 2001 - No. 20. — URL: / (date accessed 12/26/2021).
- Clinical recommendations “Hemorrhoids”, 2020. Developer: All-Russian public organization “Association of Coloproctologists of Russia”. - Text: electronic. - URL: (access date 12/26/2021).
- Mudrov, A.A. Perioperative management of patients with chronic hemorrhoids/A.A. Mudrov.-Text: direct //Medical Council, 2012. - No. 3.- P.40-44.
- Rivkin, V.L. Modern ideas about the pathogenesis, forms and treatment of hemorrhoids / V.L. Rivkin. - Text: immediate. // Consilium Medicum, 2017. - No. 19 (7.1. Surgery). – pp. 57-61.
- Savelyev, V.N. Relationship between the incidence of hemorrhoids and professions and gender in the urban district of Izhevsk for 2015 and 2022 / V.N. Savelyev, L.I. Gadelshina, K.A. Merzlikina.- Text: direct // // StudNet, 2020. – No. 12 – pp. 14-19.
- Styazhkina, S.N. Hemorrhoids as a leading problem in proctology/S. N. Styazhkina, A.A. Khairullin, L.I. Gadelshina, K.A. Merzlikina. – Text: immediate // StudNet, 2022. – No. 4 – P. 19-21.
Use of ointments and suppositories
Inexpensive ointment for hemorrhoids: Relief
Conservative treatment of hemorrhoids is not complete without suppositories and ointments. In pharmacies you can find a huge number of different remedies for hemorrhoids. They actively and quickly relieve pain, inflammation, and promote the resorption of cones.
The doctor should select the medications. It is not always possible to choose a suitable remedy on your own, since all suppositories and ointments have different components and have different properties: increase the tone of the veins, relieve swelling and pain, stop bleeding, heal, etc.
Symptoms of external hemorrhoids
The first symptoms of external hemorrhoids often begin to bother the patient before visible changes appear in the anorectal area. As a rule, the disease manifests itself:
- itching in the anal area;
- a feeling of discomfort during bowel movements and any other physical stress.
As the disease worsens, these symptoms are accompanied by pain during bowel movements. If the stool is too hard, blood may be present in the stool. This phenomenon means that the surface of the skin has been injured. Sometimes such bleeding occurs due to anal fissures. They arise due to deterioration of local blood circulation.
In addition, external hemorrhoids, which were not treated in the early stages, manifest themselves by periodic swelling of the nodes. At moments of exacerbation of the disease, they are not only palpable, but also visible upon examination. The patient also feels sharp pain when visiting the toilet or while sitting.
What are the dangers of external hemorrhoids - complications
The external form of hemorrhoids is not dangerous in terms of the sudden occurrence of rectal bleeding, but if the disease is not treated, it can have a number of unpleasant consequences. Most often, the lack of treatment for external hemorrhoids is complicated by inflammation of the tissues surrounding the node changed by the disease. This complication can be recognized by redness of the skin near the anus, swelling and increased body temperature. In the absence of therapy, inflammation is complicated by tissue necrosis and suppuration - purulent paraproctitis is diagnosed.
The second dangerous complication of external hemorrhoids is thrombosis of the hemorrhoid. Symptoms of this complication are bursting pain in the anus at rest and acute pain with straining and defecation. When thrombosis occurs, the node becomes bluish and swells. Often the swelling spreads to the buttocks and perineum.
How to deal with the disease at different stages
The expansion of hemorrhoidal veins requires an immediate response already at the initial stage of its development. In this case, it is necessary to clearly establish why hemorrhoids occurred in a particular situation, and try to reduce the negative influence of factors to a minimum. In addition, it is important to begin eliminating the consequences of changes as early as possible in accordance with the stage of the disease:
- At the first stage of hemorrhoids, drug treatment with topical drugs with anti-inflammatory, regenerating, analgesic and venotonic effects is recommended. Sclerosis of hemorrhoidal veins can also be used. Patients are also advised to follow a diet and increase physical activity.
- The second stage of hemorrhoids involves the same treatment as in the first stage, but with the use of oral medications (local ones are also included in the treatment regimen). In addition, radical methods for eliminating hemorrhoids are used: sclerotherapy, ligation, laser removal of nodes, cryotherapy or coagulation of nodes.
- The third stage of hemorrhoids requires more radical measures, and therefore conservative therapy gives way to surgical treatment - hemorrhoidectomy and vein disarterization and the use of various technologies (laser, radio waves). Latex ligation of nodes is also used at this stage.
- The fourth stage of hemorrhoids is complicated by complete prolapse of the nodes and a high probability of thrombosis and heavy bleeding. Effective methods of treating hemorrhoids at this stage are laser coagulation and hemorrhoidectomy (laser or radio wave). For vein thrombosis, thrombectomy is performed. Conservative therapy for this degree of disease is ineffective.
Regardless of what stage of hemorrhoids occurs, in parallel with the methods described above, it is necessary to apply preventive measures. They are most often aimed at eliminating the causes of hemorrhoids. This allows you to lengthen the relapse-free period and avoid further progression of the disease.
What is external hemorrhoids
External hemorrhoids are a form of disease in which the venous plexuses undergo pathological changes characteristic of this disease. They expand, acquire a heterogeneous structure and cannot perform their functions normally due to weakening of the valves.
Nodes in external hemorrhoids are localized not under the mucous membrane of the rectum, but in the subcutaneous layer near the anal sphincter. The main difference between this form of the disease and the internal one is the extremely low likelihood of bleeding and more pronounced pain during exacerbations of the disease.
Surgical treatment of external hemorrhoids
Surgical treatment of external hemorrhoids is indicated for frequent exacerbations of the disease, its rapid progression and the absence of a positive effect from drug therapy.
If blood clots are present, a thrombectomy is performed - a procedure for surgically hiding the node and then removing the blood clots. The procedure is carried out on an outpatient basis and lasts no more than half an hour and consists of several stages:
- Administration of local anesthesia.
- Opening the node - the doctor makes a small incision. For these purposes, a high-frequency coagulator or laser can be used.
- Removal of a blood clot.
- Restoring the integrity of the hemorrhoidal mucosa through suturing.
An improvement in the patient's condition is observed already in the first hours after the thrombectomy procedure. His ability to work remains, hospitalization is not required. For several days after surgery, the patient is recommended to maintain careful hygiene of the perineum and anal area, apply antibacterial ointment externally, and take painkillers.
In addition, to remove external hemorrhoids, radical hemorrhoidectomy according to the Milligan-Morgan method is used, during which part of the perianal anoderm is removed and the vessel supplying the node is intersected. Such operations are carried out using both the classical method - using a scalpel, and using a laser, high-frequency electrocoagulator. Such surgical interventions require a longer recovery.