Hemorrhoids – literally translated from Greek as “bleeding” – are the most common proctological disease associated with hypertrophy and varicose veins of the rectum with the formation of hemorrhoids and the risk of bleeding.
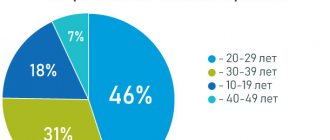
Hemorrhoids occur with equal probability in men and women; they affect about 120-145 people out of 1000, that is, about 25% of the adult population. In the structure of proctological morbidity, it occupies 43%.
Hemorrhoids can be acute or chronic, external, internal or combined (depending on the location of the hemorrhoids), primary or secondary (as a complication of other diseases and conditions), complicated or not.
Causes of hemorrhoids
The appearance of hemorrhoids is associated with congenital insufficiency of the development of veins or venous stasis, varicose veins of the rectum that develop during life.
Risk factors for developing hemorrhoids:
- sedentary lifestyle;
- age from 35 to 55 years;
- sedentary or standing work;
- heavy physical labor, pregnancy and childbirth, causing an increase in intra-abdominal pressure;
- constipation and diarrhea;
- congenital venous insufficiency (weakness of the vascular wall and venous valves of the rectal veins);
- chronic heart failure;
- stagnation in the systemic circulation;
- chronic pelvic inflammation;
- portal hypertension;
- pelvic neoplasms (bacterial salpingoophoritis, prostatitis or cystitis);
- alcoholism;
- errors in nutrition (spicy foods, lack of fluid, lack of fiber, overeating);
- intoxication of various origins (including anabolic steroids, contraceptives, chemotherapy, long-term use of psychotropic drugs).
In the rectal area there are cavernous veins connected by anastomoses to the arteries of the rectum.
These plexuses ensure the retention of feces by the rectum and defecation itself, and participate in the rectal immune barrier. Disruption of venous outflow and increased arterial inflow lead to stagnation of blood in the pelvis, overstretching of the vein wall with the formation of nodes. The trophism of the longitudinal muscle of the submucosal rectum decreases and, as a result, a fibromuscular framework of the hemorrhoidal node is formed, displacing it from the anal canal externally or into the intestinal lumen. At first, they fall out and correct themselves when straining, then they require manual reduction, and in severe cases, surgical treatment.
The scarlet color of arterial blood during hemorrhoidal bleeding is explained by the presence of anastomoses between varicose cavernous veins and rectal arteries.
Desarterization
Termination of access of arterial blood supply to the hemorrhoidal node is the main goal of disarterization. Treatment of hemorrhoids is carried out by “flashing” the arteries that supply the node.
From two to six arteries are sutured by a proctologist using special, state-of-the-art equipment. The coloproctologist learns about the detection of a hemorrhoidal node by the signal that comes from the Doppler, a special sensor placed in the anal canal.
The doctor does the firmware through the anoscope, or more precisely, through its side window. The manipulation lasts up to half an hour, and the patient then needs up to two hours to recover. The procedure is done without general anesthesia.
In the day hospital, the patient is observed for one to two hours after treatment. One procedure is enough to obtain effective treatment for hemorrhoids using the disarterization method.
Symptoms of hemorrhoids
- Constipation.
- Pain in the anus.
- Burning and itching around the anus.
- Maceration of the skin of the perianal area.
- Sphincter weakness.
- Mucous discharge from the rectum.
- Hemorrhoids are painful brown lumps that periodically appear in the anus at the entrance to the rectum or externally during defecation or other straining.
- Discharge of scarlet blood from the anus.
Acute hemorrhoids are characterized by:
- severe pain;
- bleeding from the anus that is difficult to stop.
Chronic hemorrhoids are accompanied by:
- infrequent and less intense pain;
- spotting, scanty, but constant bloody discharge.
Additional signs of hemorrhoids (not always included in the clinical picture):
- weakness, dizziness;
- dyspnea;
- depression;
- sensation of a foreign body and incomplete emptying.
Application of latex ligation
It is possible to eliminate hemorrhoids at the second stage of the disease using a low-traumatic and painless treatment method - latex ligation.
The essence of the technology is to throw special latex rings onto the base of the knot. This is done using a vacuum ligator. The device is placed in the area of the hemorrhoid and the vacuum pushes out a ring that compresses the lower part of the formation.
The nutrition of the hemorrhoid gradually stops and it is reduced and spontaneously exits. The ring is small in size, with an outer diameter of only five millimeters.
The hemorrhoidal node dies after latex ligation after 1-2 weeks. The ring and reduced formation are removed during natural bowel movements.
During this manipulation, which lasts only 15 seconds, the patient does not experience any discomfort or pain. The patient lies on the couch with his knees tucked to his stomach and can even communicate freely with the proctologist.
In agreement with the patient, the doctor uses local anesthesia.
Stages (degrees) of hemorrhoids
I degree:
- acute hemorrhoids: painful, tight-elastic small nodules in the anal area;
- chronic hemorrhoids: occasional bleeding without prolapse of hemorrhoids.
II degree:
- acute hemorrhoids: increased pain; compaction and enlargement of hemorrhoids, capable of prolapse and self-reduction into the intestinal lumen; redness of the skin around the anus; anal sphincter spasm;
- chronic hemorrhoids: prolapse and self-reduction of hemorrhoids, sometimes with bleeding from the rectum. The prolapse of nodes into the intestinal lumen or externally is provoked by straining.
III degree:
- acute hemorrhoids: inflammation and hyperemia spread to surrounding tissues; pain intensifies; around the anus - unreducible purple-bluish, dense, thrombosed painful nodes with foci of necrosis; risk of significant bleeding;
- chronic hemorrhoids: hemorrhoids periodically prolapse into the intestinal lumen or externally, and are reduced manually.
IV degree – chronic hemorrhoids: hemorrhoids fall out and cannot be reduced on their own.
At stages 3 and 4, the weak, thin longitudinal muscle cannot contract normally, so independent reduction of the node is impossible. If you do not manually adjust it in a timely manner, complications such as paraproctitis, fever, bleeding, and anal fissures develop.
Complications of hemorrhoids
- Paraproctitis (inflammation of the tissues around the rectum).
- Anal fissures.
- Hemorrhoidal bleeding.
- Thrombosis of the pelvic veins.
- Incarceration of the hemorrhoidal node.
Bleeding with hemorrhoids can be regarded as one of the most important symptoms, and as a life-threatening condition, depending on the amount of blood loss.
Minor bleeding during bowel movements appears as scarlet drops, usually not mixed with feces. They lead to the development of anemia only in 2% of cases, but they cause anxiety to the patient and require planned treatment by a proctologist. Profuse hemorrhoidal bleeding is life-threatening when the vascular wall of the hemorrhoidal node ruptures. Heavy bleeding from the anus with scarlet blood is accompanied by weakness, dizziness, sticky cold sweat, increased breathing, tachycardia and a weak pulse. These are grounds for an emergency call to emergency medical services.
While waiting for the team to arrive, the patient should be placed with his legs elevated and a cold pack placed on the anus. The patient requires emergency hospitalization.
Conservative techniques
Treatment for external hemorrhoids includes:
- Taking tablets to improve vascular tone and prevent the appearance of new nodes.
- A course of anti-inflammatory medications (to relieve or reduce pain, to relieve the inflammatory process).
- Local therapy (ointments, suppositories, gels - to soften and facilitate bowel movements, prevent injury to hemorrhoids, improve blood circulation and eliminate inflammation).
In combination with medications, on the advice of your doctor, you can use traditional methods. Herbal baths and microenemas will help alleviate the patient’s condition.
If the expected result from the treatment course is not achieved, then effective treatment of hemorrhoids will be obtained using innovative minimally invasive techniques.
How to stop hemorrhoids using latex ligation, laser vaporization, and desarterization will be discussed in more detail below.
Diagnosis of hemorrhoids
Diagnosis begins with collecting anamnesis, clarifying complaints and examination by a proctologist.
The patient is positioned in a gynecological chair with his legs adducted, knee-elbow position, and less often - on his side. A physical examination by a proctologist includes:
- digital examination of the rectum;
- anoscopy (to examine the walls of the anal canal and distal rectum);
- sphincterometry (for chronic hemorrhoids - weakness, and for acute hemorrhoids - sphincter spasm);
- colonoscopy (for differential diagnosis);
- sigmoidoscopy (diagnosis of concomitant diseases of the colon);
- X-ray of the large intestine with barium (enema).
Endoscopic examinations are performed under anesthesia, in some cases under general anesthesia.
Prevention of hemorrhoids
Preventive measures should be carried out both by people with risk factors for the development of hemorrhoids, and by those who have already begun treatment for this disease:
- physical activity: walking, fitness programs without straining, swimming, exercise therapy;
- compliance with the work and rest schedule, for example, organizing food points on the highway for drivers, “physical education” for office employees, sometimes even a temporary change of job;
- compliance with the principles of ergonomics of the work process and labor protection rules;
- a diet that includes a sufficient amount of liquid and plant fiber;
- prevention and treatment of constipation;
- careful hygiene of the anus and perineum.
In this way, it is possible to prevent exacerbation and aggravation of the severity of the disease.
Treatment of hemorrhoids
If the patient consults a proctologist in a timely manner, then at stages 1 and 2 of the disease, conservative treatment is used to relieve pain, itching and bleeding, and then influence the causes of the disease.
Drugs and a diet are prescribed to thin the stool; for pain, a pararectal novocaine blockade is used. The diet for hemorrhoids includes fluid intake (from 2 liters per day), the use of food bran, seaweed, flaxseed and plantain seed in the diet. Diet therapy is used in combination with other treatment methods and does not provide an independent clinical effect.
Various dosage forms are used to treat hemorrhoids.
For local treatment, rectal gels, ointments and suppositories for hemorrhoids are prescribed: for example, Ultraproct, fluocortolone, Relief.
Hemostatic sponges and suppositories: spongostan, collagen hemostatic sponges based on fibrinogen and thrombin, suppositories and ointments with heparin, phenylephrine, belladonna extract.
Tablet preparations are aimed at preventing constipation, increasing venous tone and stimulating blood and lymph flow, restoring microcirculation, and fighting inflammation.
For constipation, enzymes, laxatives with emollient and osmotic effects are prescribed: psyllium preparations, lactulose and macrogol.
Angioprotectors and phlebotropic drugs are recommended to normalize hemodynamics and restore microcirculation. Among the anti-inflammatory drugs used are drugs from the group of non-steroidal anti-inflammatory drugs, although in severe cases hormonal drugs (fluocortolone) are also used.
For thrombosis of hemorrhoids, bioflavonoids are recommended; to reduce the risk of bleeding - purified microgenized flavonoid fraction (diosmin + flavonoids in terms of hesperidin) (MOFF).
Minimally invasive interventions for hemorrhoids
Minimally invasive methods of surgical treatment of hemorrhoids are used on an outpatient basis and do not require general anesthesia, a long period of rehabilitation and pain relief in the postoperative period. These include sclerosis or alloying of hemorrhoids with latex rings, desarterization of the terminal branches of the superior hemorrhoidal artery, and infrared laser photocoagulation.
Surgery for hemorrhoids
At stage III, in advanced cases, surgical treatment of hemorrhoids under general anesthesia is used - removal of the node (hemorrhoidectomy).
Preparation for surgery includes:
- 2 days of a slag-free diet;
- an enema the day before and before surgery or taking Fortrans 1 glass every quarter of an hour;
- in some cases - antibiotics.
The postoperative period includes dressings and a slag-free diet.
The first stool occurs after 5-7 days and may be painful with some bleeding. Hemorrhoids are a serious proctological disease that reduces the quality of life and can, in some cases, pose an immediate threat. The risks of developing complications increase when visiting a proctologist late.
At stages 1 and 2, properly selected treatment can solve the problem or lead to long-term remission, but fear of a proctological examination and a false sense of shame prevent patients from seeking help.
At stages 3 and 4, the intervention of a proctologist-surgeon is required; this requires more time and causes additional discomfort. The arsenal of modern coloproctology has sufficient means for treating hemorrhoids in the early stages, which increases the quality and level of safety of life for a person who is familiar with this common unpleasant disease firsthand.
Non-surgical treatment of acute and chronic hemorrhoids
G
Emorrhoids are one of the most common human diseases.
Although there are no exact statistics on this matter, there is every reason to believe that up to 80% of the adult population suffers from hemorrhoids
. Patients with this disease often seek help not only from coloproctologists, but also from specialists related to the treatment of diseases of the gastrointestinal tract, i.e. internists and gastroenterologists. The ability to correctly diagnose and choose adequate treatment tactics is the main task of a doctor.
Etiology
In the light of modern concepts, hemorrhoids are based on the pathology of cavernous vascular plexuses that arise during normal embryogenesis in the submucosal layer of the distal part of the rectum. There are two theories explaining the development of hemorrhoids: “mechanical” and “hemodynamic”.
According to the “mechanical” theory, hemorrhoids are formed as a result of distal movement of the anal ridges. The latter are a normal anatomical structure and play an important role in retaining the contents of the rectum. The venous plexuses, contained in their submucosal layer, are normally fixed by connective tissue fibers of the longitudinal muscle, and below by the ligament of Parks. As intra-abdominal pressure increases, the ridges move distally. With prolonged straining and other unfavorable conditions, accelerated natural wear of the fixing apparatus occurs. Fiber rupture, degenerative and dystrophic changes are observed. Hemorrhoids increase in size and fall out of the anal canal. According to the “hemodynamic” theory, the formation of nodes is facilitated by stagnation of venous blood, which occurs as a result of mechanical obstacles (hard feces, its constant presence in the ampulla of the rectum) and the lack of relaxation of the internal sphincter during defecation. The reverse flow of venous blood is aggravated by the opening of arteriovenous shunts and spasm of precapillary arterioles. Apparently, both mechanisms are equally involved in the genesis of hemorrhoids. However, venous congestion more often causes thrombosis of nodes, and increased arterial blood flow and the opening of shunts lead to bleeding, varicose veins and inflammatory changes in the rectal mucosa. Predisposing or resolving factors include insufficient dietary fiber, constipation and straining during bowel movements, sedentary lifestyle, hot baths, heavy lifting, pregnancy and childbirth. Loose stools, abuse of laxatives, enemas, excessive anal hygiene, and spicy foods also have a negative impact.
Clinic
Characteristic manifestations of hemorrhoids are bleeding from the anus and prolapse of hemorrhoids.
.
The blood is bright red, without clots. The patient notices its presence most often in the toilet. It is released in drops or streams during bowel movements. Blood is never mixed with feces, as is the case with inflammatory diseases of the colon, and is absent from toilet paper, which is typical for an anal fissure. When hemorrhoids prolapse, blood may stain your underwear. Very rarely, the blood may become dark in color and appear in clots. This occurs due to the accumulation of blood in the ampulla of the rectum and its release during subsequent bowel movements. Pain and discomfort are usually associated with thrombosis of nodes or anal fissure. Anal itching
is a symptom that occurs for many reasons.
These include insufficient hygiene after defecation, fecal contamination of linen, prolapse of nodes with or without mucous discharge. Typically, such a patient complains that after defecation he has to repeatedly use toilet paper in order to properly clean the anus. Sometimes the patient experiences perianal edema due to the filling of the external venous plexus with blood or thrombosis of the external hemorrhoids. Since internal hemorrhoids are covered with columnar epithelium, trauma leads to inflammation and copious secretion of mucus
. The predominance of certain symptoms in the clinical picture of the disease will dictate the choice of appropriate drugs for local treatment.
Clinically, hemorrhoids manifest themselves in two main syndromes:
chronic and acute. These syndromes are phases of the same process. For the first stage of chronic hemorrhoids, a characteristic sign is the discharge of blood from the anal canal without prolapse of hemorrhoids. The second stage is accompanied by the loss of nodes, which are independently retracted into the anal canal. A distinctive feature of the third stage is the need for their manual reduction. Prolapse of nodes occurs not only during bowel movements, but also during heavy lifting and coughing. The fourth stage is characterized by constant loss of nodes and the impossibility of their reduction into the anal canal. With each stage, the symptoms become more diverse. By this time, the connective tissue frame of the anal ridges is significantly damaged and cannot be restored. This classification makes it possible in practice to select a treatment method. The basis for the development of an acute process is thrombosis of hemorrhoids - internal or external.
Treatment
Indications for conservative treatment are the initial stages of chronic hemorrhoids and the acute uncomplicated course of the disease. At the first stage, preference is given to drug treatment or infrared photocoagulation. In the second stage, drug treatment is still acceptable, but ligation with latex rings is considered an alternative. It is also acceptable in the third stage, but in the fourth stage the only adequate treatment method is hemorrhoidectomy. It should be noted that currently minimally invasive methods of treating hemorrhoids have become widespread. They provide a positive effect in 88% of cases, are associated with a low risk of complications, are painless and can be performed on an outpatient basis without loss of ability to work.
Conservative treatment of hemorrhoids
Includes general measures in the form of diet, careful personal hygiene, physical activity, taking analgesics, non-steroidal anti-inflammatory drugs, systemic venotonics, as well as local treatment with combination drugs.
Regardless of the type of hemorrhoids, special attention should be paid to simple hygiene practices
. These include refusing to use toilet paper, using baths or showers at a comfortable temperature with washing both the perianal skin and the anal canal itself with plain water without soap or other detergents. Eliminating fecal contamination reduces inflammation and itching, and warm water relieves pain associated with sphincter spasm.
Some types of exercise
that help eliminate venous stasis, for example, swimming or gymnastics.
It is very important to regulate stool consistency and frequency
. Diarrhea and constipation are equally unacceptable. In case of stool retention and strained bowel movements, irritating laxatives should be avoided. Patients are recommended to increase their intake of plant fiber (vegetables, fruits) and fluids. Additionally, wheat bran, microcrystalline cellulose or other hydrophilic colloids are included - seaweed, flaxseed. It is recommended to take preparations from plantain seeds or macrogol 4000. The choice is quite individual. These drugs are useful both during exacerbation of hemorrhoids, and in preparation for surgery, and in the postoperative period. In controlled studies, plantain seeds - Plantago ovata - have been shown to effectively reduce the incidence of bleeding and other symptoms of stage 1 and 2 hemorrhoids, but have no significant effect on the size and blood supply of hemorrhoids (Perez-Miranda et al., 1996). Patients with diarrhea are prescribed astringents, loperamide, hydrophilic colloids in combination with oral hydration. Drinking alcohol, spicy food, tea or coffee is prohibited.
An important element of the treatment program is the use of phlebotropic drugs
. This should include preparations from horse chestnut fruits, troxerutin, rutoside, escin and others. Purified micronized diosmin has been better tested in clinical trials, which effectively reduces the clinical manifestations of acute and chronic hemorrhoids, and also prevents its exacerbations (Godegere, 1994; Meyer, 1994). Drugs in this group increase the tone of the veins and the speed of lymph flow, improve microcirculation, and reduce capillary permeability caused by ischemia and inflammatory mediators. It should be noted that micronized diosmin can be safely used for acute hemorrhoids in pregnant women (Buckshee et al., 1997), in whom outpatient surgical treatment is contraindicated. The drug is prescribed 4-6 capsules for 7 days, but treatment can be prolonged - 2 capsules per day for many months.
multicomponent ointments and suppositories are widely used.
. Almost all of them include anti-inflammatory, antimicrobial, sclerosing, anticoagulant agents, anesthetics, venotonics and reparants in various combinations. The optimal composition of agents for topical treatment of hemorrhoids has not been precisely established. It remains not entirely clear whether the presence of anticoagulants, antibiotics or anesthetics in the composition has a significant impact on the therapeutic effectiveness, whether they potentiate each other, whether they are necessary and, therefore, mandatory components of therapeutic drugs. In our study (unpublished data), we compared the therapeutic effectiveness of well-known antihemorrhoidal ointments - aurobin, proctosedyl and Hepatrombin G in identical groups of patients with acute hemorrhoids of the first and second stages. The choice of these drugs was determined by the fact that each of them contained a different component. Thus, Hepatrombin G and proctosedyl contained heparin, proctosedyl and aurobin contained an antimicrobial agent, Hepatrombin G and aurobin contained an anesthetic. Thus, Hepatrombin G should be used for conditions such as:
- external and internal hemorrhoids;
— thrombophlebitis of hemorrhoidal veins of the anus;
- fistulas, eczema and itching in the anus;
- anal fissures;
— preparation for surgical intervention in the anorectal area;
- as part of combination therapy for thrombosed and operated hemorrhoids.
The ointment can be applied to the affected areas or inserted into the rectum using a screw-on tip.
When using the drug in recommended doses, no toxic effects are observed.
As the results of the study showed, Hepatrombin G reduced the frequency of bleeding from 80% to 5% within a week.
. Pain and inflammatory manifestations in the nodes and anal canal quickly subsided, and thrombosis of the nodes decreased. Excellent and good results according to the survey of doctors and patients were 90% and 85%, respectively.
If we evaluate the efficiency and cost indicators
, then
undeniable advantages were on the side of Gepatrombin
G.
The conducted study emphasizes the need for a conscious choice of certain agents for local therapy, taking into account their composition and clinical manifestations in a particular patient. In case of thrombosis of external nodes and prolapse of internal nodes, preference should be given to ointments. Suppositories are indicated only for hemorrhoids in the initial stages. They should not be pushed into the ampulla of the rectum, but held by hand until they melt completely into the anal canal. For pain, drugs with lidocaine are prescribed, for predominant inflammatory changes - with corticosteroids (Hepatrombin G, aurobin), for thrombosis - with heparin (Proctosedyl, Hepatrombin G), for swelling and enlargement of nodes - with venotonics. In patients with erosive sphincteritis and anal itching, in order to accelerate reparative processes, drugs that have an immunostimulating effect and improve tissue regeneration are used. Adverse reactions occur rarely. However, you should refrain from long-term use of corticosteroid ointments due to the dryness and microcracks they cause in the anal canal, with infectious diseases of the perianal skin, and during pregnancy. Ointments and suppositories are administered 4-6 times a day during the acute period of the disease for 2-3 weeks.
Two days before surgery and for 2 weeks after it, lactulose is prescribed (20 ml twice a day); administer suppositories with diclofenac 50 mg 3 times a day, as well as 0.2% nitroglycerin ointment; prescribe metronidazole 400 mg 3 times a day for a week; paracetamol and dehydrocodeine as indicated (Carapeti & Phillips, 2000).
Thus, the choice of treatment method for hemorrhoids is determined by the stage of the disease, the severity and nature of the symptoms.
Treatment is carried out as a complex of general measures of medicinal and non-medicinal nature. In this case, the option of modern therapy must necessarily include a combination of systemic venotonics, for example, micronized diosmin, and local treatment agents, for example, Hepatrombin G. The same measures are acceptable before preparing for ligation of nodes with latex rings and hemorrhoidectomy. It is necessary to realistically imagine the purpose and possibilities of conservative treatment, and not try to treat conservatively when the only way to relieve the patient from suffering is surgery. References:
1. Buckshee K., Takkar D., Aggarwal N. Micronized flavonoid therapy in internal hemorrhoids of pregnancy. Int J Gynaecol Obstet, 1997, 57, 145-151.
2. Carapeti EA, Phillips RKS Treatment of hemorrhoids. In: J.Beynon, NDCarr (eds): Recent advances in coloproctology, Springer-Verlag London Limited, 2000, 155-166.
3. Godegere P. Daflon 500 mg in the treatment of hemorrhoidal disease: a demonstrated efficacy in comparison with placebo. Angiology, 1994, 45, 574-578.
4. Meyer OC Safety and safety of Daflon 500 mg in venous insufficiency and in hemorrhoidal disease. Angiology, 1994, 45, 579-584.
5. Orkin B., Schwartz AM, Orkin M. Hemorrhoids: what the dermatologist knows. J Am Acad Dermatol 1999, 41, 449-456.
6. Perez-Miranda M., Gomez-Cenelilla A., Lean-Colombo T. et al. Effect of fiber supplements of internal bleeding hemorrhoids. Hepato-Gastroenterology, 1996, 43, 1504-1507.
Bibliography
- Vovk, E.I. Hemorrhoids: emergency care, treatment strategy, prevention / E.I. Vovk. - Text: electronic // Russian Medical Journal, 2001 - No. 20. — URL: / (date accessed 12/26/2021).
- Clinical recommendations “Hemorrhoids”, 2020. Developer: All-Russian public organization “Association of Coloproctologists of Russia”. - Text: electronic. - URL: (access date 12/26/2021).
- Mudrov, A.A. Perioperative management of patients with chronic hemorrhoids/A.A. Mudrov.-Text: direct //Medical Council, 2012. - No. 3.- P.40-44.
- Rivkin, V.L. Modern ideas about the pathogenesis, forms and treatment of hemorrhoids / V.L. Rivkin. - Text: immediate. // Consilium Medicum, 2017. - No. 19 (7.1. Surgery). – pp. 57-61.
- Savelyev, V.N. Relationship between the incidence of hemorrhoids and professions and gender in the urban district of Izhevsk for 2015 and 2022 / V.N. Savelyev, L.I. Gadelshina, K.A. Merzlikina.- Text: direct // // StudNet, 2020. – No. 12 – pp. 14-19.
- Styazhkina, S.N. Hemorrhoids as a leading problem in proctology/S. N. Styazhkina, A.A. Khairullin, L.I. Gadelshina, K.A. Merzlikina. – Text: immediate // StudNet, 2022. – No. 4 – P. 19-21.