Indications for use
Tocolytics are used for premature birth in late pregnancy, as well as the threat of miscarriage in order to preserve pregnancy in its early stages, habitual miscarriage - private miscarriages.
In addition, tocolytic agents are used in obstetric practice to relax the uterus before manually turning the fetus in its transverse position; with prolapse of the umbilical cord; before a cesarean section.
Certain tocolytic agents, in particular β2-adrenomimetics, in addition to obstetric practice, are used in the treatment of bronchial asthma and chronic obstructive pulmonary disease, which are accompanied by respiratory failure due to bronchospasm.
Other tocolytics (progesterone) are used to treat infertility and menstrual disorders.
Tocolytic drugs in the treatment of threatened preterm labor
The effect of drugs on the uterus can be both direct and indirect. The main links at which the action of drugs during prematurity is directed are: regulation of the level of sex hormones, effects on adrenergic, cholinergic, serotonergic receptors, as well as changes in the level of oxytocin, prostaglandins, melatonin, kinins, histamine, influence on the activity of phosphodiesterase, ionic conductivity of membranes myocytes (in particular, Ca2+ and K+), changes in relaxin content, etc.
Currently, some success has been achieved in the treatment of threatened premature birth thanks to drugs that suppress the contractile activity of the uterus, which include tocolytics. Among them, the following main groups can be distinguished: β2-adrenomimetics, α2-adrenomimetics, neurotropic and myotropic antispasmodics, calcium ion antagonists, magnesium sulfate, purinergic receptor blockers, GABAergic agents, phosphodiesterase inhibitors, serotonin receptor antagonists, antibradykinin agents, antagonists and blockers oxytocin receptors, potassium channel activators, nitrates, as well as drugs that indirectly inhibit uterine contractility (progesterone, relaxin, melatonin), inhibitors of prostaglandin biosynthesis, oxytocin release, benzodiazepine receptor antagonists.
In practical obstetrics, magnesium sulfate is often used. Although the mechanism of action of Mg2+ ions on smooth muscles has not been fully established, it is believed that they are able to influence the process of interaction of agonists with the receptor, the ion permeability of the plasma membrane of myocytes, and modulate intracellular signaling. Mg2+ ions can also slow down the release of Ca2+ from the intracellular store, thereby reducing the tone and contractile activity of the myometrium. An increase in the extracellular concentration of Mg2+ ions enhances the contraction of myometrial smooth muscles induced by oxytocin. An important aspect of the use of magnesium sulfate in obstetric practice is the presence of an anticonvulsant effect in the drug, which makes it possible to use it for the treatment of preeclampsia and eclampsia, as well as the low probability of overdose, which is also easily eliminated by the administration of calcium gluconate. When there is a threat of premature birth, the prophylactic use of magnesium sulfate as monotherapy has a less pronounced effect.
Despite the fact that the experience of using magnesium sulfate goes back several decades, in recent years a number of reports have been published about serious side effects observed with its use. Long-term monitoring has shown that quite often after administration of the drug there is a dose-dependent decrease in the fetal heart rate (HR), which is a consequence of fetal sinus bradycardia. Cardiotocograms show a significant decrease in slow and short-term heart rate variability and a decrease in the total number of oscillations. There is evidence that the administration of magnesium sulfate is accompanied by significant changes in fetal hemodynamics: in the middle cerebral artery, the speed of blood flow in diastole decreases. The stroke volume of the fetal right ventricle decreases, and the left one increases, which leads to an increase in cardiac output. Neurosonography in newborns revealed severe brain changes in the form of periventricular leukomalacia without or with grade III and IV intraventricular hemorrhages. After long-term (more than 6 weeks) use of magnesium sulfate for the purpose of tocolysis, pathology of the metaphyses of long bones is radiologically detected, which is eliminated during the first year of life. The nature of the pathology and its severity depend not only on the dose of magnesium sulfate and duration of use, but also on the stage of pregnancy in which the drug was used. Starting from the second trimester of pregnancy, long-term infusions can cause inhibition of the function of the parathyroid glands of the fetus with the subsequent development of rickets-like conditions. In the mother's body, after prolonged use of magnesium sulfate, disturbances in calcium homeostasis are observed: bone density decreases, hypercalciuria and osteoporosis develop, bleeding time increases, and neuromuscular transmission is disrupted.
In recent decades, both foreign and domestic researchers have accumulated significant experience in the use of calcium channel blockers
, especially for diseases accompanied by increased blood pressure (hypertension, preeclampsia), as well as in case of threat of miscarriage. What is common in the pathogenesis of these diseases is an increase in the tone and contractile activity of smooth muscles due to an increase in the concentration of free calcium (Ca2+) in smooth muscle cells, which enters through the receptor and voltage-dependent calcium channels. Blocking the latter reduces the contractile activity of vascular smooth muscles and myometrium. Based on the strength of the inhibitory effect on the uterus, these drugs were ranked as follows: nitrendipine, nicardipine, nifedipine, verapamil, diltiazem. The most commonly used drug is nifedipine, which inhibits the spontaneous contractile activity of the myometrium, effectively and quickly reducing the amplitude and frequency of contractions, as well as the basal tone of the myometrium. Later, it was reported that nifedipine inhibited the contractile activity of the myometrium caused by exogenous prostaglandins, which made it possible to successfully use the drug to treat the threat of premature birth. However, the use of calcium channel blockers as tocolytics during preterm pregnancy is often accompanied by undesirable effects: flushing, tachycardia and arterial hypotension. In large doses, the drugs disrupted atrioventricular conduction and increased the fetal heart rate.
Progesterone
, although not a tocolytic in the literal sense of the word, is increasingly used in tocolytic therapy protocols for preterm birth. The close connection between progesterone production and miscarriage has been known for a long time, and the use of this drug in cases of threatened miscarriage has been around for decades. And only in recent years have the basic (primarily immune) mechanisms of gestagens performing their protective function in relation to the fetus been revealed. The concentration of progesterone in the blood and urinary excretion of its main metabolite, pregnanediol, begin to increase from the moment of ovulation in the conception cycle and further progressively increase during physiological pregnancy, reaching a maximum by the 36th week. Initially, the hormone is formed in the corpus luteum, and in later stages of pregnancy - mainly in the placenta. About 30% of secreted progesterone reaches the fetus, and this amount can increase with fetal pathology (in particular, with stress, chronic hypoxia and fetal malnutrition). Since the fetus is immunologically foreign to the mother’s body, quite complex and not fully explored phylogenetic mechanisms of immunomodulation are formed during pregnancy, aimed at protecting the fetus. During normal pregnancy, a physiological increase in progesterone production induces the formation of receptors for both progesterone itself and PIBF; Thus, this hormone is involved in the immune mechanisms of protecting the embryo, maintaining and preserving pregnancy.
After implantation, simultaneously with an increase in progesterone secretion, a natural change in the level of progesterone receptors occurs, which is noted not only in the decidual tissue, but also in the myometrium: the concentration of nuclear receptors increases, and the concentration of cytosolic receptors decreases. The presence of a sufficient level of progesterone and its receptors ensures the functioning of the mechanisms involved in the suppression of uterine tone and contractile activity. Thus, progesterone reduces the synthesis of prostaglandins in the uterus, and the main metabolite of progesterone, 5α-pregnanediol, by blocking oxytocin receptors, reduces the sensitivity of the myometrium to oxytocin and prostaglandin F2α, and the number of α-adrenergic receptors in it. Inhibition of the latter occurs without their simultaneous modification, as a result of which the expression of α-adrenergic receptors becomes dominant. This circumstance allows, against the background of the use of progesterone, to significantly reduce the doses of β2-adrenergic agonists used, which is important in practical terms, since it makes it possible to avoid the side effects characteristic of β2-adrenergic agonists while maintaining their therapeutic benefits.
It is equally important that sufficient levels of progesterone ensure the maintenance of the appropriate ultrastructural organization of the myometrium - the formation of intercellular gap junctions through which impulses are transmitted is prevented. This makes it difficult to generalize the contraction of individual muscle fibers in the contraction of the entire uterus in response to various types of stimulation. Due to the presence of antiandrogenic activity in progesterone, it is able to protect the female fetus from androgens synthesized in the maternal body, the level of which increases during pregnancy and significantly exceeds physiological values in diseases such as polycystic ovary syndrome and congenital adrenal hyperplasia.
As is known, the decisive role in the regulation of the contractile function of the uterus during childbirth is assigned to biologically active substances of lipid nature - prostaglandins.
(especially PGF2α). The tocolytic effect of prostaglandin synthesis inhibitors has been proven experimentally and as a result of clinical observations. 2-3 hours after the administration of indomethacin, the amplitude and tone of the uterus decreases, the duration of contractions decreases, as a result of which complete normalization of contractile activity occurs 3-4 days from the start of therapy. Similar data were obtained from clinical trials of acetylsalicylic acid, metamizole sodium, flufenamic acid, naproxen, etc.
However, having not selective properties, but a wide spectrum of pharmacological action, inhibitors of prostaglandin synthesis cause undesirable effects on the fetus and newborn. The most severe complications manifest themselves in premature closure of the arterial flow and a pronounced increase in pulmonary arterial pressure. The serious effect of salicylic acid preparations on the processes of hematopoiesis and the blood coagulation system is reported that they cause a significantly higher incidence of anemia in pregnant women, etc.
organic nitro compounds – can be used for tocolysis
. The ability of exogenous nitric oxide (NO) to relax myometrial smooth muscle cells has generated interest in investigating NO donors as potential tocolytic agents. Since the contractile activity of human myometrial smooth muscle cells is insensitive to NO synthesis blockers, it is believed that a possible source of NO synthesis in the uterus is the vascular endothelial cells of the uterus and placenta, which synthesize it at the level of increased estrogen levels in the blood during pregnancy. During full-term pregnancy, its concentration decreases, which contributes to the development of labor. On the contrary, the concentration of NO in the cervix on the eve of labor increases due to the expression of induced NO synthase, which may be one of the factors stimulating cervical ripening. In obstetric practice, nitroglycerin is used as an NO donor for tocolysis using its transdermal route of administration. In women with preeclampsia and its combination with the threat of premature birth, nitroglycerin provides a significant reduction in maternal blood pressure without changing the fetal heart rate and, most importantly, significantly reduces blood flow resistance in the uteroplacental and fetal placental circulation. It should be noted, however, that reports on the effectiveness of NO donors are still sporadic, and the issue of their effectiveness and safety of use in pregnant women requires further study.
Also, one of the promising drugs for the treatment of premature birth is atosiban.
– antagonist of oxytocin receptors. It is known that the density of oxytocin receptors on the membrane of myometrial smooth muscle cells increases sharply on the eve of childbirth, causing an increase in the sensitivity of the myometrium to physiological concentrations of oxytocin. A similar increase in receptor density is observed during premature birth, which indicates the role of oxytocin in the development of this pathology. Obviously, blocking oxytocin receptors with the competitive antagonist of oxytocin and vasopressin atosiban, which has such properties, may be a therapeutic alternative in the treatment of preterm labor.
Currently widespread and successful use throughout the world β
2
-mimetics indicates
Pharmacologically, they are sympathomimetic amines whose starting compound is phenylethylamine with a long carbon chain near the nitrogen atom. The plasma membrane of myometrial smooth muscle cells contains several types of β-adrenergic receptors, the selective activation (or inhibition) of which is accompanied by relaxation or contraction of the myometrium. In cases of labor disturbances, different expression of the receptor protein, the amount of mRNA, transforming growth factor (TGF)-adrenoreceptors types I and II, and TGF-β1 are observed. When there is a threat of premature birth, the level of TGF-β-adrenergic receptors type I does not change, while the level of TGF-β-adrenergic receptors type II sharply decreases. An increase in the density and activity of β-adrenergic receptors, especially type II, ensures a natural state of uterine tone during the physiological course of pregnancy. A decrease in activity or expression is observed during premature labor, and their stimulation with β-adrenergic agonists inhibits untimely uterine contractions.
According to modern concepts, the mechanism of the uterorelaxing effect of β2-adrenomimetics lies in the activation of the cell membrane enzyme adenylate cyclase, which they cause, with the subsequent formation of cyclic adenosine-3,5-monophosphate from its precursor, adenosine triphosphate. Further activation of protein kinase and other enzymes causes a decrease in the concentration of freely circulating calcium ions in the cytosol, which is accompanied by relaxation of the muscle cell and the myometrium as a whole. β-mimetics cause an increase in blood flow through tissues and organs, an increase in perfusion pressure and a decrease in vascular resistance. The effect on the cardiovascular system is manifested by an increase in heart rate, a decrease in systolic and diastolic pressure. This cardiotropic effect must be taken into account when carrying out therapy with these drugs, especially when they interact with other drugs. Before administering β-mimetics, it is necessary to monitor blood pressure and pulse rate. To reduce adverse cardiovascular effects, calcium channel blockers - finoptin, isoptin, verapamil - must be prescribed. As a rule, compliance with the rules for the use of β-mimetics, the dosage regimen, and strict monitoring of the state of the cardiovascular system allow one to avoid serious side effects.
Additional effects from the use of β-mimetics include: an increase in circulating blood volume and heart rate, as well as a decrease in peripheral vascular resistance, blood viscosity and plasma colloid-oncotic pressure.
Drugs acting on β2-adrenergic receptors include isoxsuprine, dilatol, orciprenaline sulfate, terbutaline, ritodrine, partusisten, salbutamol, Ginipral.
Despite the common mechanism of action of β2-mimetics on the uterus, they all differ in the degree of tocolytic activity, which depends on the dose, methods of drug administration, endocrine and physiological changes caused by pregnancy.
More than 20 years ago, isoxsuprine was used for the first time in obstetric practice to maintain pregnancy. When using it, a positive effect was observed in 75–80% of cases. By reducing the basal tone, amplitude and frequency of contractions, it significantly increases the adaptive capabilities of the newborn in the treatment of intrauterine fetal asphyxia. Dilatol was 2–3 times more active than isoxsuprine.
Orciprenaline sulfate effectively inhibits uterine contractions, reducing the amplitude by 70–90%. When it treats discoordinated labor, a decrease in intrauterine pressure is observed, contractions become more coordinated and regular.
Adrenergic agonists with pronounced tocolytic activity and a selective effect on β2-adrenergic receptors include terbutaline sulfate. Clinical observations indicate that it effectively blocks spontaneous and oxytocin-induced labor. Tocolysis performed with terbutaline allowed in 83.3% of cases to prolong pregnancy until the birth of a viable child.
Ritodrine plays an important role in tocolytic therapy. It is characterized by significantly greater specificity of action than isoxsuprine and terbutaline, and since 1981 it has been the drug of choice for the treatment of preterm labor. Using the drug to prevent recurrence of premature birth, according to data, allows you to prolong pregnancy by more than 38 days. Despite the fairly widespread use of β-adrenergic agonists, their use is limited by the presence of a number of side effects in these drugs, which require not only dose adjustment, but also, in some cases, drug withdrawal. Thus, ritodrine is capable of causing peri- and intraventricular hemorrhages of III and IV degrees, which are ultrasonographically recorded in 15% of newborns. In pregnant women, ritodrine causes a decrease in the number of red blood cells, hemoglobin content and hematocrit, an increase in blood glucose levels, and possible jaundice and myocardial ischemia. β-adrenergic agonists, especially ritodrine, reduce the sensitivity of the vagal cardiac baroreflex and vagal modulation of heart rate, and increase heart rate variability mediated by the sympathetic nervous system. Depending on the dose, ritodrine rapidly increases the level of renin activity, the concentration of total and active renin and the blood plasma. This, in turn, may be accompanied by disturbances in fluid balance and the risk of developing pulmonary edema, the most dangerous complication during treatment with ritodrine.
Among the proven tocolytics is partusisten, which, even in small therapeutic doses, normalizes the frequency of contractions and hypertonicity of the uterus, thereby having a pronounced relaxing effect. Due to the combination of high antispasmodic activity with minimal effect on the cardiovascular system, it is most often used in obstetric clinics in many countries.
In recent years in Russia, the most common and frequently used drug from the group of β-mimetics is hexoprenaline, a selective β2-sympathomimetic that relaxes the muscles of the uterus. Under its influence, the frequency and intensity of uterine contractions decreases. The drug inhibits spontaneous and oxytocin-induced labor contractions; During childbirth, it normalizes excessively strong or irregular contractions. Under the influence of hexoprenaline, in most cases, premature contractions stop, which, as a rule, allows the pregnancy to be prolonged to full term. Due to its selectivity, hexoprenaline has little effect on the cardiac activity and blood flow of the pregnant woman and fetus.
Hexoprenaline consists of two catecholamine groups, which in the human body are methylated by catecholamine-O-methyltransferase. While the effect of isoprenaline is almost completely abolished by the introduction of one methyl group, hexoprenaline becomes biologically inactive only if both of its catecholamine groups are methylated. This property, as well as the drug’s high ability to adhere to surfaces, are considered the reasons for its long-lasting effect.
Indications for the use of hexoprenaline are:
•
Acute tocolysis - inhibition of labor contractions during childbirth with acute intrauterine asphyxia, immobilization of the uterus before cesarean section, before turning the fetus from a transverse position, with umbilical cord prolapse, with complicated labor. As an emergency measure in case of premature birth before taking the pregnant woman to the hospital.
•
Massive tocolysis is the inhibition of premature labor contractions in the presence of a smoothed cervix and/or dilatation of the uterine pharynx.
•
Long-term tocolysis is the prevention of premature birth during intensified or frequent contractions without smoothing the cervix or dilating the uterus. Immobilization of the uterus before, during and after surgical correction of isthmic-cervical insufficiency.
Contraindications to the use of this drug: hypersensitivity to one of the components of the drug (especially for patients suffering from bronchial asthma and hypersensitivity to sulfites); thyrotoxicosis; cardiovascular diseases, especially cardiac arrhythmias occurring with tachycardia, myocarditis, mitral valve disease and aortic stenosis; cardiac ischemia; severe liver and kidney diseases; arterial hypertension; intrauterine infections; lactation.
Dosage
. For acute tocolysis, use 10 mcg of hexoprenaline, diluted in 10 ml of sodium chloride or glucose solution, administered over 5–10 minutes. slowly intravenously. If necessary, continue administration by intravenous infusion at a rate of 0.3 mcg/min. (as in massive tocolysis).
For massive tocolysis - at the beginning, 10 mcg of hexoprenaline slowly intravenously, then - intravenous infusion of the drug at a rate of 0.3 mcg/min. The drug can be administered at a rate of 0.3 mcg/min. and without prior intravenous injection. Administer intravenously (20 drops = 1 ml).
As a first line of help in cases of threatened miscarriage after 24–25 weeks of pregnancy or threatened premature birth, hexoprenaline is prescribed at the rate of 0.5 mg (50 mcg) in 250–400 ml of saline intravenously, gradually increasing the dose and rate of administration (maximum 40 drops /min.), combining the infusion with the intake of calcium channel blockers (finoptin, isoptin, veropamil) under the control of pulse rate and blood pressure parameters. 20 minutes before the end of the drip, 1 tablet of hexoprenaline (5 mg) per os
and then every 4 hours.
A reduction in the dose of hexoprenaline should be carried out after the threat of interruption has been completely eliminated, but not less than after 5–7 days (reduce the dose, and not extend the time interval between taking the drug dose).
Thus, the accumulated domestic and foreign experience indicates that despite the ever-increasing arsenal of tocolytic agents, today there are no more effective means for suppressing uterine contractility (that is, the threat of premature birth) than β-mimetics, in particular, hexoprenaline .
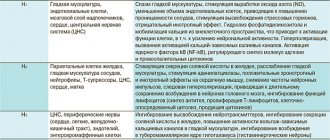
Classification of drugs that relax the muscles of the uterus
The classification of tocolytics is quite diverse and is based primarily on the mechanism of action of the drugs:
- β2-Adrenergic agonists - stimulants of β2-adrenergic receptors of the myometrium: hexoprenaline, fenoterol, terbutaline, salbutamol.
- Progestin preparations are progesterone receptor stimulants: progesterone, hydroxyprogesterone.
- Oxytocin antagonists - oxytocin receptor blockers: atosiban.
- Anticholinergics - M-cholinergic receptor blockers: butylscopolamine.
- Calcium antagonists - calcium channel blockers: magnesium sulfate.
In addition, sedatives (anxiolytics) - for example, diazepam, as well as anesthetics - for example, enflurane (the so-called central muscle relaxant effect) relax the muscles of the uterus due to the influence on the centers of the brain and spinal cord responsible for muscle tone.
Particular attention is paid to non-steroidal anti-inflammatory drugs (NSAIDs), which inhibit the synthesis of biologically active substances (mediators) - prostaglandins. Prostaglandins are responsible not only for the implementation of inflammation - pain, swelling, increased body temperature, but also significantly stimulate the tone of the uterus. Therefore, all NSAIDs (in particular, indomethacin, acetylsalicylic acid, naproxen, etc.) have a tocolytic effect.
Tocolytic
There is no definitive first-line tocolytic agent. [12]
Various types of agents are used with varying degrees of success and side effects. Some medications are not specifically approved by the US Food and Drug Administration (FDA) for use in stopping uterine contractions in preterm labor and are instead used off-label.
| Medicine | Mechanism of action | Description | Possible contraindications | Maternal side effects | Side effects for the fetus and newborn |
| Terbutaline (bretin) | β2 agonist | Off-label use, the FDA has advised that terbutaline injection should only be used in emergency situations and should never be used in the oral form of the drug [3] | Cardiac tachyarrhythmias, poorly controlled diabetes mellitus, hyperthyroidism, prolonged tocolysis (>48–72 hours) [4] | Tachycardia, palpitations, hypotension, shortness of breath, chest pain, hypokalemia, hyperglycemia, lipolysis, pulmonary edema, myocardial ischemia [5] | Fetal tachycardia, hyperinsulinemia, hypoglycemia, myocardial and septal hypertrophy, myocardial ischemia [ citation needed ] |
| Ritodrine (Utopar) | β2 agonist | No longer FDA approved [6] | Poorly controlled thyroid disease and diabetes [ citation needed ] | Metabolic hyperglycemia, hyperinsulinemia, hypokalemia, antidiuresis, thyroid dysfunction, physiological tremor, palpitations, nervousness, nausea or vomiting, fever, hallucinations [ citation needed ] | Neonatal tachycardia, hypoglycemia, hypocalcemia, hyperbilirubinemia, hypotension, intraventricular hemorrhage [ citation needed ] |
| Fenoterol | β2 agonist | Diabetes | |||
| Salbutamol (INN) or albuterol (USAN) | β2 agonist | Diabetes | |||
| Hexoprenaline (Ginipral) | β2 agonist | Not FDA approved | Hyperthyroidism, cardiovascular diseases, glaucoma, placental abruption, vaginal bleeding, inflammatory diseases of the internal genital organs, 1st trimester of pregnancy, breastfeeding [7] [8] | Dizziness, anxiety, tremor, hyperhidrosis, tachycardia, hypotension, hyperglycemia, edema | Hypoglycemia, bronchospasm, anaphylactic shock [8] |
| Nifedipine (Procardia, Adalat) | Ca 2+ channel blocker | It is one of the most commonly used tocolytic agents. [9] | Heart diseases. [10] It should not be used simultaneously with magnesium sulfate [ citation needed ] | Hot flashes, headache, dizziness, nausea, transient hypotension. Calcium channel blockers should be prescribed with caution to patients with renal failure and hypotension. Concomitant use of calcium channel blockers and magnesium sulfate may lead to cardiovascular collapse [ citation needed ] | Nothing noted yet [ citation needed ] |
| Atosiban | Oxytocin receptor antagonist | Fewer side effects than β2 agonists [ citation needed ] | |||
| Indomethacin | NSAIDs | Late pregnancy (ductus arteriosus), significant renal or liver failure [ citation needed ] | Nausea, heartburn [ link needed ] | Narrowing of the ductus arteriosus, pulmonary hypertension, reversible decrease in renal function with oligohydramnios, intraventricular hemorrhage, hyperbilirubinemia, necrotizing enterocolitis [ citation needed ] | |
| Sulindak | NSAIDs | Coagulation disorders or thrombocytopenia, NSAID-sensitive asthma, other NSAID sensitivity [ citation needed ] | |||
| Magnesium sulfate [11] | Myosin light chain inhibitor | It has not been shown to be effective in delaying labor or stopping early labor. [11] Meta-analyses have not supported it as a tocolytic agent [11] [12] [13] | Absolute contraindication : myasthenia gravis [ quote ]. Use as a tocolytic agent may result in fetal or infant death. [eleven] | Hot flashes, lethargy, headache, muscle weakness, diplopia, dry mouth, pulmonary edema, cardiac arrest [ citation needed ] | Lethargy, hypotension, respiratory depression, demineralization with long-term use [ citation needed ] |
| Ethanol | GABA A receptor PAM | It has been shown to be ineffective. Was a commonly used tocolytic in the mid-20th century, but more recent double-blind studies [14] showed that it was not effective. |
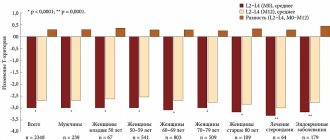
Calcium channel blockers (eg, nifedipine) and oxytocin antagonists (eg, atosiban) may delay delivery by 2 to 7 days, depending on how quickly the medication is administered. [15] Otherwise, tocolysis is rarely successful after 24–48 hours because current medications do not alter the basis of labor activation. [12] However, delaying preterm birth by 48 hours appears to be sufficient to allow pregnant women to be transferred to a center specialized in the management of preterm labor and thus allow the administered corticosteroids to reduce organ immaturity in the newborns.
The effectiveness of β-adrenergic agonists, atosiban and indomethacin represents a reduced odds ratio (OR) of delivery within 24 hours by 0.54 (95% confidence interval (CI): 0.32-0.91) and 0.47 within 48 hours (OR 0.47, 95). % CI: 0.30-0.75). [1]
Antibiotics may also delay the onset of labor in women with premature rupture of membranes, but this is not usually characterized as tocolysis.
Basics of treatment with drugs that relax the muscles of the uterus
Tocolytic drugs are prescribed only by a highly qualified obstetrician-gynecologist. Typically, the use of tocolytic drugs is carried out in a hospital setting, while the patient is under the constant supervision of medical personnel, her physical activity is limited, which can provoke premature contractions or miscarriage. This set of activities is colloquially called “conservation.”
Tocolytic drugs are usually used for a long time - several months, sometimes - the entire gestation period.