Osteoarthrosis (deforming arthrosis) is a chronic degenerative disease of the joints. This disease is characterized by damage to articular cartilage and tissues surrounding the joints. As a rule, the inflammatory process in the joints is not pronounced. The main mechanism for the development of the disease is considered to be a disorder in the cartilage tissue (excessive wear) due to various reasons.
This can be either natural aging of the body, or the development of similar changes in joints at a younger age (premature aging) due to malnutrition of cartilage tissue, which leads to faster wear of cartilage tissue. With the development of osteoarthritis, salts accumulate in the tissues surrounding the joint, joint deformation and inflammation of the joint capsule (synovitis). About 10-12% of the population suffers from osteoarthritis, most often these are women over 40-45 years old, and in the older age group (over 60-65 years old) almost 100% suffer from osteoarthritis.
Most often, large joints are affected, such as the hip joint, knee, ankle joint, and somewhat less frequently, the shoulder and elbow joints. Small joints can also be involved in the process (joints of the hands). Osteoarthritis (OA), as a rule, is often combined with other degenerative diseases of the musculoskeletal system such as osteochondrosis and spondylosis deformans. The etiology of osteoarthritis is not fully understood, but factors that contribute to the development of osteoarthritis can be divided into hereditary and acquired.
There are also primary and secondary deforming osteoarthritis. The causes of primary osteoarthritis include:
Excessive or repeated loads that significantly exceed the physical capabilities of the cartilage tissue of the joints. This can be either sports or associated with heavy physical work.
Congenital abnormalities of the geometric shape of the joints, which leads to disruption of the biomechanics of the joint and a change in the correct distribution of load vectors on the articular cartilage. These may be congenital dysplasia of the joints, deforming diseases of the spine, abnormalities of skeletal development, underdevelopment and hypermobility of ligaments.
Changes in the structure of cartilage tissue of joints due to microtraumatization, microcirculation disorders, joint injuries (intra-articular fractures, dislocations, subluxations, hemarthrosis).
The following conditions are most often considered to be the causes of secondary osteoarthritis:
Inflammatory processes caused by infection or injury, congenital dysplasia of the hip and knee joints, developmental disorders of the joint, instability of the joint (including after injury), endocrine diseases (for example, diabetes mellitus), metabolic changes (gout, hemachromatosis), necrotic changes in bone tissue , intoxication with heavy metal salts, rheumatological diseases such as rheumatoid arthritis, SLE, blood diseases (hemophilia). There are three stages in the development of osteoarthritis:
- Stage 1 is characterized by the presence of minor morphological changes in the joint and is manifested by pain during physical activity (radiologically there will only be a narrowing of the joint space). Morphological changes in articular cartilage at stage 1 are manifested by the appearance of roughness and disintegration of the tissue structure.
- Stage 2 is characterized by constant pain in the joints; radiographically, the narrowing of the joint gap is more pronounced; osteophytes appear; morphologically, this stage is characterized by the appearance of tuberosity on the surface of the cartilage and the development of osteophytes.
- Stage 3 osteoarthritis is characterized not only by pain, but also by the appearance of joint dysfunction. Morphologically, stage 3 is manifested by thinning of the cartilage until it disappears, thickening of the intra-articular ligaments, and a sharp decrease in intra-articular fluid.
Concept and classification of osteoarthritis
Osteoarthritis predominantly affects weight-bearing joints: knees, hips, shoulders and lumbosacral joints.
A 2011 comparative study found that the topical analgesic capsaicin was 50% more effective as a pain reliever for OA than placebo. An inhibitor of neuronal reuptake of serotonin and norepinephrine, a third-generation antidepressant, duloxetine is more effective than placebo in relieving pain in OA. OA is a heterogeneous group of conditions with different etiologies and similar biological, morphological and clinical manifestations. OA primarily affects weight-bearing joints: knees, hips, shoulders, and lumbosacral joints. The distal and proximal interphalangeal joints and metacarpal joints may be affected, but such localization is much less common. Daily loads, which are mostly placed on weight-bearing joints, play an important role in the development of the disease.
Primary, or idiopathic, is osteoarthritis, the cause of which remains unknown. It can be local (one or two joints are affected) or generalized (three or more joints are affected). Local OA is most often associated with damage to the knee joints (gonarthrosis) and hip joints (coxarthrosis). In secondary OA, there is an obvious cause of the disease: trauma, metabolic disorders, a history of other rheumatological diseases, and so on.
Kinds
Most often, the disease is classified depending on the location of the pathological process. Osteoarthritis can be unilateral or bilateral and deform almost any joint:
- knee;
- hip;
- ankle;
- brachial;
- temporomandibular;
- elbow;
- small joints of the foot and hand;
- intervertebral joints.
Depending on the cause, osteoarthritis can be primary (occurs on its own) or secondary (develops against the background of another pathology or injury).
Risk factors for osteoarthritis
The causes of osteoarthritis of the joints may be the following:
- age
- obesity
- injury
- heredity (family history of OA)
- low estrogen levels in women
- muscle weakness
- characteristics of work (for example, regular heavy physical activity)
- infection
- acromegaly
- history of inflammatory arthrosis (for example, rheumatoid arthritis)
- hereditary metabolic disorders (eg, alkaptonuria, hemochromatosis, Wilson's disease)
- hemoglobinopathies (eg, sickle cell anemia, thalassemia)
- neuropathic disorders leading to the development of Charcot's joint (syringomyelia, tabes dorsalis, diabetes mellitus)
- morphological risk factors (eg, congenital hip dislocation)
- damage to bone tissue (Paget's disease, aseptic necrosis and others)
- history of joint surgery (for example, meniscectomy)
What complications can occur in advanced cases or untreated osteoarthritis of the joints?
If the disease develops uncontrolled and there is no treatment, a person will most likely have difficulty moving independently, which significantly increases the risk of injury due to numerous bruises and falls.
Damage to the foot can lead to pain during walking and inflammation of the big toe of the lower extremity.
In the vast majority of cases, the severe form, when refusing to seek medical help, negatively affects the patient’s performance. In some cases, this can be avoided by making some changes.
Other complications include:
- loss of motor ability;
- the occurrence of chronic arthritis and arthrosis;
- loss of spinal column stability;
- complete immobilization of the limb and disability.
It is worth noting that, among other things, there are also risks of postoperative complications, for example, after arthroplasty - inflammation caused by various factors.
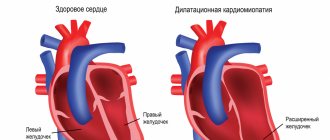
Pathophysiology of OA
Vascularization of cartilage is a feature of the development of osteoarthritis. Blood vessels grow into the cartilaginous continuation of the articular surface, and ossification of the articular capsule begins from the subchondral zone
Primary and secondary OA have a common pathological basis. OA was previously thought to be a degenerative disorder resulting from the biochemical breakdown of hyaline cartilage in synovial joints. However, today a slightly different point of view is accepted, which suggests that not only the articular cartilage suffers, but also the entire joint, including the subchondral bone, synovial membrane and nearby tissues.
Despite the degenerative nature of OA, there is increasing evidence that after the synthesis of cytokines by chondrocytes and the release of cytokines into the joint cavity, an inflammatory process develops. Proinflammatory mediators (cytokines interleukin-1 and tumor necrosis factor) are not involved in matrix degradation [2], but activate chondrocytes in the superficial layer of cartilage, which increases the synthesis of matrix metalloproteinases and, consequently, degeneration of articular cartilage.
In the initial stage of OA, due to increased synthesis of proteoglycans, the main component of the matrix, swelling of the cartilage occurs. This stage can last several years or even decades, and its main manifestation is hypertrophy of the articular cartilage.
Further, as OA progresses, the level of proteoglycans decreases to extremely low values, and their qualitative composition changes. Damaged cartilage is subject to overload, as a result of which the synthesis of metalloproteinases (collagenase, stromelysin and others) increases. They contribute to the further destruction of proteoglycans and the entire collagen network, which determines the progressive degeneration of cartilage. As a result, the cartilage softens and loses its elasticity and becomes increasingly damaged. Microscopically, peeling and vertical clefts are noticeable on the smooth surface of the articular cartilage at this stage of the disease.
OA is characterized by vascularization of cartilage and changes in the subchondral bone. An actively mineralizing osteoid is formed in it, and then subchondral cysts and microfractures form. This leads to the development of subchondral sclerosis.
Degrees
Orthopedists distinguish 4 degrees of the disease:
- Grade 1: there are no symptoms, but with exertion a person may notice slight pain or discomfort; all cartilage damage occurs at the microscopic level;
- 2nd degree: pain occurs not only during exercise, but also at rest; x-rays reveal a narrowing of the joint space and isolated bone growths;
- 3rd degree: destruction reaches its peak, surrounding tissues are involved in the pathological process; the pain becomes constant, and the pictures clearly show deformation, narrowing of the joint space and numerous osteophytes; Often at this stage, dislocations and subluxations of the joint occur due to weakening of the ligaments;
- 4th degree: bone growths completely block the joint, movement is impossible.
Symptoms of osteoarthritis
Typical symptoms requiring treatment:
- joint pain (the first sign of the disease, may appear in the early stages);
- decreased range of motion, crepitus - crunching in the joints (often present);
- feeling of stiffness during or after rest. Joint stiffness is common after sleep, usually for less than 30 minutes.
Symptoms of osteoarthritis of the hands:
- the distal interphalangeal joints are most often affected;
- the proximal interphalangeal joints and the joints at the base of the thumb may be affected;
- Heberden's nodes (palpable osteophytes in the distal interphalangeal joints) are more common in women than in men;
- inflammatory changes, as a rule, are absent or remain unnoticed (mild).
Rheumatoid arthritis (RA) primarily affects the wrists and the metacarpophalangeal and proximal interphalangeal joints. Damage to the distal interphalangeal or lumbosacral joints is not typical for it. In addition, RA is associated with prolonged (more than 1 hour) morning stiffness, swelling, and increased joint temperature.
OA should also be differentiated from:
- avascular necrosis of bone tissue
- fibromyalgia
- gout and pseudogout
- ankylosing spondylitis
- neuropathic arthropathy (Charcot's joint)
- Lyme disease
- patellofemoral syndrome
- psoriatic arthritis
Prevention
Like most diseases, osteoarthritis is much easier to prevent than to cure. Simple rules will help maintain healthy joints and stop the process at an early stage if it has already occurred:
- sufficient physical activity: amateur sports are a good prevention of physical inactivity, help improve microcirculation and form a good muscle frame;
- normalization of body weight: excess weight creates increased stress on the joints, especially the knee, hip and ankle;
- minimizing traumatic factors: vibration, standing work, heavy lifting contribute to the development of joint diseases;
- correct posture and shoes to distribute the load on the joints;
- timely treatment of diseases that can cause secondary osteoarthritis.
Diagnostics
Diagnosis of osteoarthritis is based on clinical and radiological examination data. Clinical studies have examined the ability to measure autoantibodies and synovial fluid markers as indicators of OA [4]. None of these indicators have proven reliable for diagnosing and monitoring OA.
As a rule, indicators of the acute phase of inflammation in OA are within normal limits. In the case of erosive arthritis, an increase in ESR is possible. In the synovial fluid, leukocytes are detected in quantities below 2000 per μl, with a predominance of mononuclear cells.
The method of choice in diagnosing OA is radiographic examination [5]. Some features of articular cartilage and soft tissue that are not visible on radiographs can be visualized using MRI. However, in most patients with OA, MRI is not necessary.
Ultrasound has no role in the routine clinical assessment of a patient with OA. It can be used as a tool for monitoring cartilage degeneration, as well as for intra-articular injections.
Arthrocentesis can help rule out inflammatory arthritis, infection, or crystalline arthropathy associated with deposition of microcrystals of varying composition.
The diagnostic results determine which methods will be used to treat osteoarthritis.
Diet
Proper nutrition is not the main factor in the prevention of osteoarthritis, but it will also make its contribution to maintaining healthy joints. Recommended:
- a diet balanced in calories, macro- and micronutrients;
- sufficient amounts of vitamins and minerals;
- exclusion of spicy, canned, excessively fatty foods, alcohol, as well as products with artificial flavors and dyes;
- minimizing fast carbohydrates.
Collagen and omega-3 acids have a good effect on the condition of cartilage, which is why aspic and sea fish and olive oil should always be present in the diet.
Therapy
Treatment of osteoarthritis is aimed at relieving pain and improving the functional state of the joint. Optimally, patients should receive a combination of non-pharmacological techniques and pharmacotherapy [6].
The inflammatory reaction in the joint is catalyzed by cyclooxygenase (COX) and lipoxygenase (LOX), producing mediators of inflammation and pain (prostaglandins, including prostaglandin E2 and leukotrienes). The latter, in addition to direct participation in the pathogenesis of inflammation, reduce the threshold for pain perception in the affected joint, thereby increasing pain sensations
Non-drug ways to control OA:
- weight normalization [7]
- physiotherapy
- physiotherapy
- occupational therapy
- unloading of some joints (for example, knee, hip)
Advantages of the clinic
“Health Energy” is a multidisciplinary clinic with modern equipment and experienced staff. We are always aware of new developments in the field of treatment and prevention of diseases and offer our patients not only time-tested methods, but also modern, advanced methods.
Come to us if you need:
- fast and effective diagnostics;
- assistance from experienced doctors;
- an integrated approach to the treatment of diseases;
- comfortable conditions in the clinic;
- affordable prices for all medical services.
Osteoarthritis is a disease that begins gradually, develops slowly, but ultimately often leads to disability. Don’t let it change your life, sign up for a consultation with the orthopedists at Energy of Health.
Pharmacotherapy of OA, recommendations of the International Society for the Study of OA (OARSI), 2014
The following drugs are used to treat osteoarthritis:
Paracetamol
Inflammatory mediators can stimulate angiogenesis. Thus, hypoxia, which often occurs during the inflammatory process, stimulates the synthesis of vascular endothelial growth factor (VEGF). Vascular growth can also be stimulated by fibrinogen and inflammatory cells: macrophages, lymphocytes, mast cells and fibroblasts.
A 2010 meta-analysis confirmed the effectiveness of paracetamol as a moderate pain reliever for OA [8]. However, studies have shown an increased risk of side effects associated with paracetamol use, including gastrointestinal (GI) manifestations and multiorgan disorders [8]. In connection with these data, OARSI recommends using the drug strictly in accordance with the dosage and duration of the course.
Capsaicin
A 2011 comparative, double-blind, randomized study of 100 patients with knee OA found that the topical analgesic capsaicin was 50% more effective as an analgesic for osteoarthritis than placebo [9].
Corticosteroids (intra-articular injections)
Recent studies demonstrate a clinically significant short-term analgesic effect [10]. There are several other recommended medications for the treatment of osteoarthritis.
Chondroitin
Four studies examining the use of chondroitin in OA showed mixed results. Some trials showed some analgesic effects, while others showed chondroitin's effect was no different from placebo [11]. In addition, specialists from the International Society for the Study of OA - OARSI note a high degree of heterogeneity of studies and their low quality, and therefore a final assessment of the effectiveness of chondroitin is extremely difficult. Thus, the effect of chondroitin as a symptomatic remedy is considered questionable, and it is not recommended as a drug for the treatment of OA.
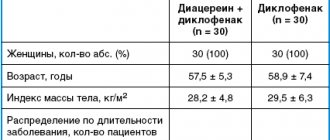
Diacerein
A 2010 meta-analysis examining data from six studies involving 1533 patients found a relatively modest but statistically significant analgesic effect of the non-narcotic analgesic diacerein compared with placebo [12]. The meta-analysis also noted a significant increase in the risk of diarrhea among volunteers taking diacerein. However, diacerein is considered safer than NSAIDs.
Duloxetine
Studies have proven that the inhibitor of neuronal reuptake of serotonin and norepinephrine, the third generation antidepressant duloxetine, is more effective than placebo in relieving pain in OA [13]. However, 16.3% of patients receiving duloxetine experienced side effects (compared to 5.6% in the placebo group). These include nausea, dry mouth, drowsiness, fatigue, decreased appetite, and hyperhidrosis. In this regard, the need for the use of duloxetine for the treatment of OA in persons with concomitant diseases (diabetes mellitus, arterial hypertension and other cardiovascular diseases, renal failure, gastrointestinal bleeding, depression, limitation of physical activity, including due to obesity) is recognized doubtful*.
Glucosamine
A meta-analysis of three randomized controlled trials found a beneficial effect of rosehip powder (5 g/day) as an analgesic for OA compared with placebo, but these data require further study.
Two large studies evaluating the effectiveness of glucosamine in the treatment of OA yielded conflicting results [6]. One study showed a statistically significant analgesic effect, while another showed no effect. The latest meta-analysis, which included a large-scale study, did not prove the effectiveness of glucosamine at all. Based on these data, OARSI experts came to the conclusion that the effectiveness of glucosamine as a symptomatic agent for OA is questionable. It is not recommended as a treatment for OA [6].
Hyaluronic acid (intra-articular injections)
The results of clinical trials (CTs) examining the effectiveness of intra-articular injection of hyaluronic acid (HA) have been controversial [6]. Conflicting data from meta-analyses and individual studies cast doubt on the advisability of using hyaluronic acid preparations for OA of the knee and hip joints. For OA of several joints, GC is not recommended.
Oral NSAIDs
Taking these drugs is included in recommendations for the treatment of osteoarthritis for patients without concomitant diseases. For concomitant gastrointestinal diseases, it is necessary to prescribe proton pump inhibitors along with NSAIDs. For patients at high risk (GI bleeding, myocardial infarction, history of chronic renal failure), oral NSAIDs are strictly not recommended.
Risedronic acid
A review of the literature conducted by Japanese scientists in 2010 suggests that high doses of risedronic acid do not reduce the severity of OA symptoms, but may help reduce the progression of OA by maintaining the structural integrity of the subchondral bone [14]. Laboratoryly, this effect is manifested by a decrease in the level of the cartilage degradation marker CTX-II. Thus, the effectiveness of residronic acid requires further study.
Opioids
Studies have shown moderate effectiveness of codeine and morphine for OA of the knee and hip. A 2006 Cochrane meta-analysis of placebo-controlled trials involving 1019 patients found statistically significant benefits for tramadol compared with placebo [15].
List of sources
- Folomeeva O. M., Erdes Sh. F. Prevalence and social significance of rheumatic diseases in the Russian Federation // Doctor (rheumatology). 2007. No. 10. P. 3–12.
- Poole AR. An introduction to the pathophysiology of osteoarthritis. Front Biosci. 1999 Oct 15. 4: D662–70.
- van Baarsen LG et al. Heterogeneous expression pattern of interleukin 17A (IL-17A), IL-17F and their receptors in synovium of rheumatoid arthritis, psoriatic arthritis and osteoarthritis… Arthritis Res Ther. 2014. 16 (4):426.
- Brandt KD. A pessimistic view of serologic markers for diagnosis and management of osteoarthritis. Biochemical, immunologic and clinicopathologic barriers. J Rheumatol Suppl. 1989 Aug. 18:39–42.
- Recht MP et al. Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology. 1993 May. 187(2):473–8.
- Zhang W et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007 Sep. 15(9):981–1000.
- Felson DT et al. Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study. Ann Intern Med. 1992 Apr 1. 116 (7):535–9.
- Bannuru RRDU, McAlindon TE. Reassessing the role of acetaminophen in osteoarthritis: systematic review and meta-analysis. Osteoarthritis Research Society International World Congress; 2010 Sep 23–26; Brussels, Belgium. Osteoarthritis Cartilage 2010; 18 (Suppl 2):P 250.
- Kosuwon W et al. Efficacy of symptomatic control of knee osteoarthritis with 0.0125% of capsaicin versus placebo. J Med Assoc Thai¼Chotmaihet Thangphaet 2010; 93(10):118e95. Epub 2010/10/27.
- Bannuru RR et al. Therapeutic trajectory of hyaluronic acid versus corticosteroids in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Arthritis Rheum 2009; 61 (12):1704–11.
- McAlindon TE et al. OARSI guidelines for the non-surgical management of knee osteoarthritis //Osteoarthritis and Cartilage. - 2014. - T. 22. - No. 3. - pp. 363–388.
- Bartels EM et al. Symptomatic efficacy and safety of diacerein in the treatment of osteoarthritis: a meta-analysis of randomized placebo-controlled trials. Osteoarthritis and Cartilage/OARS. Osteoarthritis Research Society 2010; 18(3):289–96.
- Citrome L, Weiss-Citrome A. A systematic review of duloxetine for osteoarthritic pain: what is the number needed to treat, number needed to harm, and likelihood to be helped or harmed? Postgrad Med 2012; 124(1):83.
- Iwamoto J. et al. Effects of risedronate on osteoarthritis of the knee //Yonsei medical journal. 2010. No. 2. 164–170 pp.
- Cepeda MS, Camargo F, Zea C, Valencia L. Tramadol for osteoarthritis. Cochrane Database Syst Rev 2006; (3):CD005 522. Epub 2006/07/21.
Treatment of deforming arthrosis
Deforming arthrosis requires long-term complex treatment, including:
- drug therapy;
- non-drug treatment methods;
- traditional methods;
- surgery.
Drug therapy
The primary goal is to relieve sick people from pain. For this purpose, symptomatic treatment is carried out. Depending on the severity of the pain syndrome, drugs from the following drug groups are prescribed intramuscularly, rectally, orally or externally:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), which have an analgesic effect. All NSAIDs are divided into:
- non-selective - the first drugs in this group that suppress the action of the enzyme cyclooxygenase (COX), involved in the synthesis of prostaglandins (PG) - biologically active substances that support inflammation; but there are PGs that are also responsible for other physiological reactions, for example, for protecting the gastrointestinal tract (GIT) mucosa from damage; inhibition of these PGs leads to gastrointestinal irritation, therefore non-selective NSAIDs (Diclofenac, Ibuprofen (Nurofen), Ketorolac (Ketorol), etc.) are contraindicated for ulcerative processes in various parts of the gastrointestinal tract; but these are effective remedies and, in the absence of contraindications for use, they are prescribed for arthrosis;
- selective (selective) - drugs of the latest generation that suppress the action only of the COX-2 enzyme, which is responsible for the synthesis of pro-inflammatory PGs; they do not suppress the effect of COX-1 and do not have side effects on the gastrointestinal tract; these are Nimesulide (Nise), Meloxicam (Movalis), Celecoxib (Celebrex), Etoricoxib (Arcoxia); they can be used for gastrointestinal diseases.
- Muscle relaxants that relieve painful muscle spasms - Mydocalm.
- Local anesthetics (novocaine and lidocaine blockades) - injections into the most painful points.
Pathogenetic therapy (impact on the mechanisms of disease development) includes:
- Preparations containing chondroitin and glucosamine (chondroprotectors) are biologically active substances that promote the restoration of cartilage tissue; they are prescribed in the form of tablets, injections, ointments (Teraflex, Artra, Dona, Structum, Chondroitin).
- Preparations based on hyaluronic acid - intra-articular administration improves the shock-absorbing properties of the joint, prevents injury to cartilage and bone tissue.
Non-drug treatment
Taping for deforming arthrosis
This section of conservative treatment includes: proper balanced nutrition, means of fixing joints, physical therapy, massage, physiotherapeutic methods, etc.
Nutrition
There is no special diet for deforming osteoarthritis. You should adhere to the rules of a rational, nutritious diet, excluding high-calorie foods (fatty meat, canned meat, smoked sausages) and easily digestible carbohydrates (sweets, baked goods, sweet carbonated drinks) from the diet, since it is necessary to maintain normal body weight, preventing obesity.
Joint fixation
The need for fixation arises to give the limb the correct position. For this purpose, they are prescribed to wear orthoses, knee pads (if the patient has deforming arthrosis of the knee joint), fixation of joints using special adhesive tapes (taping), support when walking on canes and crutches.
Therapeutic exercise (physical therapy) and massage
Physical activity stimulates the restoration of joint function. Therefore, exercise therapy complexes are the main type of treatment for deforming arthrosis. Complexes are selected for each patient individually depending on his condition. The first classes must be supervised by a physical therapy instructor, and only after the patient learns to perform all the exercises correctly can they be performed at home. Basic rules for performing exercise therapy:
- regularity of classes;
- no sudden movements;
- increasing loads under the control of pain - as soon as pain appears, the load is reduced.
Swimming and gentle physical exercises (Pilates, yoga) are very beneficial. It is not recommended to jump or play outdoor games that place stress on pathologically altered joints.
Massage activates blood circulation and metabolism in articular and periarticular tissues, promoting their regeneration.
Physiotherapy
Physiotherapy is necessarily part of complex therapy. Procedures are prescribed to eliminate pain, inflammation and swelling during synovitis (electrophoresis with novocaine, hydrocortisone), eliminate muscle spasms (paraffin, ozokerite), stimulate tissue regeneration (magnetic and laser therapy), and increase the body's overall resistance (UVR).
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Folk remedies
These methods allow you to expand the range of complex treatment and reduce the drug load:
- onion broth in vegetable broth; Chop a medium-sized onion, fry in butter, then boil in half a liter of water until the onion is completely boiled; add a glass of vegetable broth (cabbage + carrots + potatoes) to the broth and bring to a boil; divide the resulting broth into 2 servings and drink in two doses half an hour before meals; course from 4 to 6 weeks; perfectly stimulates metabolic processes;
- honey massage before bed; Apply a tablespoon of warm liquid honey to the painful area above the joint and rub in with light circular movements for 3 to 5 minutes; cover with a cotton napkin, wrap and leave overnight.
Surgical treatment of deforming arthrosis
In cases where conservative treatment methods do not help, endoprosthetics is performed - replacing the destroyed joint with an artificial one.
Diagnosis of the disease
Any clinical recommendations for deforming osteoarthritis are prescribed after a thorough examination. Therefore, if you discover its signs, you should see a rheumatologist as soon as possible.
He will prescribe the following diagnostic procedures:
- X-ray diagnostics, thanks to which the degree of narrowing of the joint gap, the size and localization of growths, and features of bone changes will be clearly visible;
- for a more detailed examination - CT and ultrasound of the spine, as well as MRI of the damaged joint;
- puncture of the diseased joint (if necessary);
- endoscopy (arthroscopy) of the damaged knee joint (not mandatory, at the discretion of the specialist).