Pharmacological properties of the drug Ramipril
Antihypertensive drug, ACE inhibitor. By suppressing the synthesis of angiotensin II, it reduces its vasoconstrictor effect and stimulating effect on aldosterone secretion. Increases renin activity in blood plasma, inhibits bradykinin metabolism. Reduces peripheral vascular resistance, does not significantly change renal blood flow (and in some cases increases it) and glomerular filtration rate. It has an antihypertensive effect both in the standing and lying position of the patient, and does not cause compensatory tachycardia. It has an antihypertensive effect, both at high and low levels of renin in the blood plasma. After a single dose, the antihypertensive effect is observed within 1–2 hours, reaches a maximum after 3–6 hours and lasts for 24 hours. With daily use, the antihypertensive effect increases gradually over 3–4 weeks and persists with long-term treatment. Sudden withdrawal does not lead to a rapid increase in blood pressure. Ramipril also has a cardioprotective effect due to the inhibition of ACE in the myocardium and, possibly, due to the accumulation of bradykinin. There is evidence that ramipril promotes the reverse development of myocardial hypertrophy in patients with hypertension (arterial hypertension), reduces the frequency of arrhythmias during myocardial reperfusion. The ability of ramipril to prevent contractile changes in the vascular endothelium resulting from eating foods high in cholesterol has been described. After oral administration, it is quickly absorbed in an amount of at least 50–60% of the dose taken. Concomitant food intake does not affect the degree of absorption, but slows down the absorption of the active substance. The maximum level in blood plasma is reached 2–4 hours after administration. Primary metabolism occurs in the liver, resulting in the formation of a pharmacologically active derivative of ramipril - ramiprilat. Ramiprilat is approximately 6 times more active in inhibiting ACE than ramipril. Plasma protein binding is 73% for ramipril, and 56% for ramiprilat. In patients with liver disease, the conversion of ramipril to ramiprilat slows down, the level of ramipril in the blood plasma may increase 3 times, but the maximum concentration of ramiprilat in the blood plasma does not change. In heart failure, there is an increase in the concentration of ramiprilat in the blood by 1.5–1.8 times. In elderly people, pharmacokinetics do not change significantly.
Ramipril price, where to buy
The price of Ramipril varies by region, however, on average, a package containing capsules or tablets has a nominal volume of 2.5 mg. will cost 200 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Ramipril tablets 2.5 mg 28 pcs. JSC Tatkhimfarmpreparaty
87 rub. order - Ramipril tablets 5mg 30pcsOzon LLC
177 RUR order
- Ramipril-Akrikhin tablets 5 mg 30 pcs. JSC Akrikhin
180 rub. order
- Ramipril tablets 5 mg 28 pcs. JSC Tatkhimfarmpreparaty
106 rub. order
- Ramipril-AKOS tab. 0.01g 30pcs JSC Sintez
RUB 178 order
Pharmacy Dialogue
- Ramipril-Akrikhin tablets 10 mg No. 30 Akrikhin JSC
RUB 202 order
- Ramipril-Akrikhin tablets 5 mg No. 30 Akrikhin JSC
167 RUR order
- Ramipril-SZ (5 mg tablet No. 30) North Star ZAO
92 rub. order
- Ramipril (tab. 10 mg No. 30) Synthesis OJSC
RUB 197 order
- Ramipril (5 mg tablet No. 30) Synthesis OJSC
RUB 152 order
show more
Pharmacy24
- Euroramipril N 5 mg/12.5 mg No. 20 tablets Pharma Start TOV, Ukraine
53 UAH order - Euroramipril N 10 mg/12.5 mg No. 20 tablets Pharma Start TOV, Ukraine
74 UAH order
PaniPharmacy
- Euroramipril N tablets Euroramipril N5 tablets. 5mg/12.5mg No. 20 Ukraine, Pharma Start LLC
69 UAH order
- Euroramipril N tablets Euroramipril N10 tablets. 10mg/12.5mg No. 20 Ukraine, Pharma Start LLC
93 UAH order
show more
Use of the drug Ramipril
The initial dose for the treatment of hypertension (arterial hypertension) is usually 2.5 mg 1 time per day (in the morning) on an empty stomach; subsequently, if necessary, the dose is gradually increased every 2–3 weeks. In some patients, a uniform antihypertensive effect is achieved by using ramipril 2 times a day. The maximum daily dose is 10 mg, maintenance - 2.5–5 mg. In the absence of optimal blood pressure reduction, diuretics can be prescribed. For chronic heart failure, the recommended initial dose is 1.25 mg/day. Depending on the patient's response, the dose can be increased (double within 1–2 weeks). If the daily dose is 2.5 mg or more, it is taken in 1 or 2 doses. When treating patients who have suffered myocardial infarction, the recommended initial dose is 2.5 mg 2 times a day. In patients with impaired renal function (creatinine clearance from 30 to 60 ml/min), patients with diabetes mellitus, as well as in patients over the age of 65 years, the initial daily dose should not exceed 1.25 mg, and the maximum - 5 mg.
The importance of the RAAS in the pathogenesis of nephropathy in hypertension
Activation of the RAAS, on the one hand, is the leading physiological mechanism for maintaining renal blood flow; on the other, it is the activity of angiotensin II that is associated with an increase in intraglomerular pressure, leading to the development of nephropathy. The RAAS is activated when perfusion pressure in the kidneys decreases. Angiotensin II is one of the most powerful natural pressor agents, providing
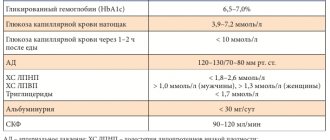
vasoconstriction and maintenance of blood flow, primarily renal. Angiotensin II, in addition to direct vasoconstriction, is involved in the regulation of the synthesis of endothelial relaxation factor - NO, inflammatory mediators, growth factors, matrix metalloproteinases. The effect of angiotensin II on local angiotensin receptors of the first type stimulates cell proliferation and processes called organ and tissue remodeling. In addition to the plasma RAAS, common to the body, the activation of which is of key importance for maintaining hemodynamics during bleeding, a drop in blood pressure, acute myocardial infarction, etc., a local RAAS has been discovered that functions in target organs, primarily in the heart, kidneys, brain, blood vessels, peripheral muscles . In the kidneys, chronic activation of the local RAAS (increased production of angiotensin II and aldosterone) is accompanied by the development of glomerular hypertension with subsequent death of the glomeruli, a gradual decrease in filtration and an increase in proteinuria, loss of electrolytes, decreased diuresis and the appearance of signs of chronic renal failure (CRF). Therefore, to achieve an optimal organoprotective effect, it is important to block not only the systemic, but primarily the tissue RAAS. Use of angiotensin-converting enzyme inhibitors in the treatment of nephropathy To prevent/slow the progression of chronic kidney disease (CKD), strict blood pressure control is primarily necessary. The target blood pressure level in patients with CKD stages 3–5 is blood pressure < 130/80 mmHg. Art., in the presence of proteinuria, the feasibility of achieving more stringent control of blood pressure < 125/75 mm Hg is also discussed. Art. Angiotensin-converting enzyme inhibitors (ACEIs) may be considered the drug of choice. The renoprotective properties of ACE inhibitors have been proven for patients with diabetic nephropathy with type 1 and type 2 diabetes, as well as for non-diabetic nephropathy. A meta-analysis of a number of studies confirmed the nephroprotective properties of ACEIs for individuals with proteinuria more than 0.5 g/day, which is observed regardless of the initial state of renal function and creatinine clearance.
The effectiveness of ACE inhibitors in the treatment of nephropathy was proven for ramipril in patients with non-diabetic nephropathy in the REIN (Ramipril Efficacy in Nephropathy) study, for fosinopril - in the ESPIRAL (Effect of antihypertensive treatment on progression of renal insufficiency) and PREVEND IT (Prevention of Renal and Vascular Endstage) studies Disease Intervention Trial), for lisinopril - in the CALM study (The candesartan and lisinopril microalbuminuria study). Apparently, all ACE inhibitors have renoprotective properties. Therefore, impaired renal function in patients with hypertension is an additional indication for the use of drugs of this class.
It must be taken into account that with a sharp decrease in glomerular filtration rate (GFR), it is necessary to reduce the dose of ACEI. The dose of the drug is reduced when GFR drops by more than 30%. If GFR decreases by more than 50%, ACE inhibitors should be discontinued until GFR is restored to baseline. The state of kidney function must be monitored once every 5–7 days. Once target doses of ACE inhibitors and target blood pressure values are achieved, further monitoring of GFR can be carried out once every 12–24 weeks.
ACEI therapy should be initiated with caution in patients with hypotension: systolic blood pressure <90 mm Hg. Art., blood potassium level above 5 mmol/l and serum creatinine more than 221 µmol/l (2.5 mg/dl).
Side effects of the drug Ramipril
Arterial hypotension, collapse and associated tachycardia, arrhythmia, angina pectoris, myocardial infarction, stroke; the appearance or intensification of renal dysfunction up to the development of acute renal failure (especially with simultaneous use of diuretics), proteinuria, dry cough, bronchitis, shortness of breath, sinusitis, rhinitis, in some cases - bronchospasm; nausea, pain in the epigastric region, dyspepsia, vomiting, diarrhea, constipation, dysphagia, anorexia, increased activity of liver enzymes and bilirubin concentration in the blood serum, hepatitis, cholestatic jaundice, liver failure, pancreatitis, anxiety, depression, dizziness, increased irritability, drowsiness, sleep disturbances, amnesia, tremor, convulsions, neuralgia, neuropathy, paresthesia, hearing loss, tinnitus, blurred vision, itching, rash, urticaria, photosensitivity, angioedema, erythema multiforme, arthralgia, arthritis, myalgia, hyperkalemia, decreased hemoglobin and hematocrit levels, leukopenia, eosinophilia, edema, nosebleeds, impotence, increased sweating, general weakness, weight gain, increased concentrations of uric acid and glucose in the blood.
Side effects
While taking the drug, the following side effects may occur: heart failure, hypotension, angina pectoris, myocardial infarction, syncope, vertigo, arrhythmia, vasculitis, thrombocytopenia, nausea and vomiting, diarrhea, dispersion, constipation, pancreatitis, dysgraphia, liver dysfunction, jaundice , increased salivation, dizziness and headaches, asthenia, amnesia, depressive states, drowsiness, neuropathy, tremor, sleep disorders, hearing loss, liver necrosis, blurred vision, cough, shortness of breath, sinusitis, pharyngitis, rhinitis, laryngitis, photosensitivity, as well as weight loss, angioedema, fever.
Special instructions for the use of Ramipril
Patients are warned to immediately consult a doctor if they develop fever, swollen lymph nodes and/or sore throat (these symptoms may be associated with the development of agranulocytosis). At the beginning of treatment and regularly during therapy, the number of leukocytes, the level of hemoglobin in the peripheral blood, the level of potassium, creatinine and liver enzymes in the blood are monitored, especially in patients with impaired renal function, diffuse connective tissue diseases, receiving immunosuppressants, cytostatic agents, allopurinol or procainamide . Patients who have a decrease in blood volume and/or sodium deficiency (for example, due to long-term use of diuretics, sodium restrictions, hemodialysis, repeated vomiting or diarrhea) are especially at risk of developing significant arterial hypotension when prescribed ramipril. Before starting the use of ramipril in such patients, blood volume and sodium levels are corrected. If ramipril is prescribed to patients already taking diuretics, in order to avoid the development of significant arterial hypotension, these drugs are discontinued within 2–3 days. Then, if blood pressure is not sufficiently controlled by taking ramipril alone, diuretics are added again. If preliminary withdrawal of diuretics is not possible, ramipril is prescribed in the minimum initial dose (1.25 mg/day). In patients with heart failure, ramipril can also cause the development of severe arterial hypotension, which in some cases is accompanied by oliguria or azotemia and (rarely) acute renal failure. Patients with an increased risk of developing arterial hypotension after taking the first dose of ramipril, as well as after increasing the dose of it or a diuretic, should be under strict medical supervision, especially in the first 2 weeks of treatment. During treatment with ramipril, hemodialysis or hemofiltration using membranes based on polyacryl metall sulfonate (for example, “AN 69”) with high ultrafiltration activity is excluded, since in this case there is a risk of developing serious anaphylactoid reactions. In the case of emergency hemodialysis, the patient is first transferred to another antihypertensive drug (but not an ACE inhibitor) or other membranes are used for hemodialysis. In case of development of angioedema, especially spreading to the tongue, pharynx or larynx, adrenaline, corticosteroids, and antihistamines are administered intravenously. Prescribe with caution to patients whose work requires increased attention and speed of mental and motor reactions, especially at the beginning of treatment and during the change of antihypertensive drugs. It is not recommended to drink alcohol at the same time.
Contraindications
It is not recommended to use the drug in case of hypersensitivity to ACE inhibitor substances , hypotension , hyperkalemia , renal failure , as well as during pregnancy and lactation. In addition, it is recommended to avoid Ramipril when treating children under 18 years of age and elderly patients.
The use of the medicine should be limited if there is a history of angioedema, suppression, severe autoimmune diseases, poor circulation, atherosclerosis, stenosis, after a kidney transplant, with diabetes mellitus and some lung diseases, hyponatremia, on dialysis .
Drug interactions Ramipril
When taking antihypertensive, diuretic drugs, opioid analgesics, and anesthetics simultaneously, the antihypertensive effect of ramipril may be enhanced. With simultaneous use of NSAIDs (for example, acetylsalicylic acid, indomethacin), table salt, a decrease in the antihypertensive effect is possible. When taking potassium supplements and potassium-sparing diuretics (for example, amiloride, spironolactone, triamterene), a significant increase in potassium levels in the blood is possible. When taken simultaneously with lithium preparations, it is possible to increase the concentration of lithium in the blood (regular monitoring of lithium levels is necessary). With simultaneous treatment with antidiabetic agents (sulfonylurea derivatives, insulin), the hypoglycemic effect may be enhanced. When used simultaneously with allopurinol, cytostatic agents, immunosuppressants, procainamide, leukopenia may develop. With the simultaneous use of alcohol, a sharp increase in the effect of alcohol is possible.