Ignoring the symptoms, laziness and negligent attitude towards the treatment of type 2 diabetic disease (T2DM) have led to the fact that to the rather small number of patients with insulin-dependent type 1 diabetes (T1DM), every year a huge number of people with severe T2DM are added, who need to control their sugar levels. In the blood serum, injections of the insulin hormone are already required.
Moreover, diabetics with mild to moderate T2DM are recommended to take insulin injections during infectious diseases. Therefore, information about the drug Insulin Humalog will be useful to all diabetics, regardless of the type of diabetic disease.
The processing of glucose in the cells of the human body is impossible without the insulin hormone.
Domestic and foreign pharmacological companies produce a fairly wide range of different insulin preparations administered subcutaneously. They not only have different names and prices, but also different natures of origin, quality and duration of action. This article will talk about medications such as Insulin Humalog, Insulin Humalog Mix (50/50 and 75/25 options).
Pharmacological properties of the drug Humalog mix
Humalog Mix 25 is a DNA recombinant analogue of human insulin, is a mixture of 25% insulin lispro (a fast-acting drug to lower blood glucose levels) and 75% suspension of insulin lispro protamine (an intermediate-acting drug to lower blood glucose levels). Insulin lispro was found to be equivalent to human insulin. It begins to act quickly, the peak of action occurs earlier, and the duration of the glucose-lowering effect is shorter than that of regular human insulin. The earlier onset of action of insulin lispro (15 minutes after administration) is directly related to its faster absorption. This allows insulin lispro to be administered closer to meals (0–15 minutes) compared to regular insulin (30–45 minutes before meals). The main effect of insulin lispro is the regulation of glucose metabolism. In addition, all insulins have several anabolic and anti-catabolic effects on a significant number of body tissues. In muscles and other tissues (except the brain), insulin leads to rapid intracellular transport of glucose and amino acids, stimulates anabolism and inhibits protein catabolism. In the liver, insulin supports the uptake and storage of glucose in the form of glycogen, inhibits gluconeogenesis and ensures the conversion of excess glucose into fats. The onset of action of insulin lispro is noted 15 minutes after subcutaneous administration. The rate of absorption and, accordingly, the onset of action depends on the site of administration.
Expected effects from Insulin Humalog
Medicinal insulin hormones are classified:
- according to the duration of their action - long, medium, short, ultra-short, prolonged and combined;
- according to the origin of the active substance - pork and its semi-synthetic derivatives, genetically engineered human and its modified analogues.
Insulin Humalog is the patented name of the French trademark of a drug with the active substance Lispro (Insulin lispro), a genetically recombinant analogue of a hormonal substance produced by beta cells of the human pancreas. Its only difference from the natural human insulin hormone is the reverse arrangement of proline (No. 28) and lysine (No. 29) amino acid residues in its molecules.
This difference is intentional. Thanks to it, Insulin Humalog and its synonyms can be used both by patients with T1DM, replenishing the deficiency of the transport hormone, and by patients with T2DM, whose cell membranes have developed insulin resistance (immunity) to their own insulin hormone.
Insulin is a transport hormone that “opens” the cell membrane to glucose
Single-dose medicinal products containing genetically recombinant Lispro are classified as ultra-short-acting insulin hormones. The expected time for the drop in plasma glucose concentration is 10-20 minutes after injection under the skin. The maximum peak effect will be observed within 1 to 3 hours, and the total duration of the hypoglycemic effect is 3-5 hours.
For your information. “Experienced” insulin-dependent diabetics know, but “newbies” should remember that an injection of an ultra-short hormone will act on both an adult and a child - after 10 minutes if it is injected under the skin in the lower abdomen, and after 20 minutes if the injection is made in the shoulder. However, the duration of the effects is highly individual and may change over time.
The main mechanism of action is the regulation of carbohydrate-lipid metabolism and assistance in the utilization of glucose by cells, which occurs by replenishing the missing amount of insulin hormone, without which this main source of energy (glucose) cannot penetrate through the cell membranes into their middle.
In addition to the absorption of glucose and lowering its concentration in the blood plasma, Insulin Humalog has the following effects:
- increases the level of fatty acids, glycerol and glycogen in the cells of skeletal muscle fibers;
- increases the production of protein compounds;
- intensifies the use of amino acids;
- reduces the rate of glycogenolysis and gluconeogenesis.
On a note. By the way, compared to human genetically engineered soluble insulin hormone, the degree of reduction in hyperglycemia after meals with Insulins Lizpro is more pronounced.
All insulin drugs are used against the background of a diet and its restriction of 1700-3000 kcal
Analogues of Insulin Humalog
Analogues of the French ultra-short Insulin Lispro (Humalog) are the Danish Insulin Aspart (Novo-Rapid) and the German Insulin Glulisine (Apidra). All ultra-short types of insulin can be injected immediately before or immediately after a meal.
Use of the drug Humalog mix
The dosage of insulin lispro in adult patients is determined individually. The rapid onset of action of the drug allows insulin to be administered closer to meals (0–15 minutes) compared to insulin mixtures that contain regular insulin (30–40 minutes before meals). Humalog Mix 25 must be administered only subcutaneously. The drug cannot be administered intravenously. S/C is administered into the shoulder, thigh, buttock or abdomen. You cannot inject in the same place for a month. Do not inject the product into a blood vessel. Patients must be taught injection techniques. Instructions for preparation and use. Before use, you must turn the Humalog Mix cartridge 10 times between your palms. Holding the cartridge by one end, turn it 180° 10 times so that the glass ball travels the entire length of the cartridge with each turn. The insulin should become uniformly cloudy or milky in color. If this does not happen, you should repeat the previous steps until the components are completely mixed. Insulin cartridges should be checked frequently. Do not use the drug if the insulin substance (white substance) remains seemingly separated from the liquid after mixing. Do not use if the suspension contains lumps or if white particles stick to the bottom or walls of the cartridge, making the glass dull. In order to load the cartridge into the pen-injector, attach the needle and inject insulin, you should refer to the manufacturer's instructions for the pen-injector for administering insulin.
Humalog® Mix 50
The dose of Humalog® Mix 50 is determined by the doctor individually depending on the concentration of blood glucose.
Humalog® Mix 50 can be administered shortly before meals. If necessary, Humalog® Mix 50 can be administered immediately after meals.
Intravenous administration of Humalog® Mix 50 is unacceptable.
The temperature of the administered drug should be at room temperature.
Subcutaneous injections should be given in the upper arm, thigh, buttock or abdomen. Injection sites should be rotated so that the same site is used no more than approximately once a month. When administering Humalog® Mix 50 subcutaneously, care should be taken to avoid the drug entering the blood vessels. After the injection, do not massage the injection site. Patients should be taught proper injection technique.
For Humalog® Mix 50 in cartridges
Humalog® Mix 50 cartridges are only suitable for subcutaneous injection using refillable pens manufactured by Eli Lilly.
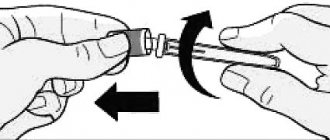
Immediately before use, the cartridge with Humalog® Mix 50 should be rolled between the palms ten times and rocked, turning 180° also ten times to resuspend the insulin until it takes the form of a homogeneous cloudy liquid or milk. Do not shake vigorously as this may cause foam, which may interfere with proper dosage delivery. To facilitate mixing, the cartridge contains a small glass ball.
Do not use insulin if there are flakes in it after mixing.
When installing the cartridge into the pen, attaching the needle, and injecting insulin, you must follow the instructions that come with each pen.
For the drug Humalog® Mix 50 in the KwikPen™ syringe pen
KwikPen™ pens are suitable for subcutaneous injections only.
Using the KwikPen™ pen, you can inject from 1 to 60 units (1 IU to 60 IU) of insulin per injection in 1 unit increments. Before performing an injection, you must read the Instructions for Use of the KwikPen™ syringe pen.
Patients with impaired renal function
Insulin requirements may be reduced if renal function is impaired.
Patients with liver dysfunction
Insulin requirements may be reduced in cases of liver dysfunction due to decreased gluconeogenesis and decreased breakdown of insulin; however, in patients with chronic liver dysfunction, increased insulin resistance may lead to increased insulin requirements.
Use in children
The safety and effectiveness of Humalog® Mix 50 in patients under 18 years of age have not been studied.
Instructions for using the KwikPen™ syringe pen
Humalog®, Humalog® Mix 25, Humalog® Mix 50 100 IU/ml, 3 ml
PLEASE READ THE INSTRUCTIONS FOR USE OF THE QUIKPEN™ PEN BEFORE USING
Read this guide before using insulin for the first time. Each time you receive a new package of KwikPen™ syringe pens, you must read the instructions for use again, because it may contain updated information. The information contained in the instructions does not replace a conversation with your doctor about the disease and your treatment.
The QuickPen™ (“pen”) is a disposable, prefilled pen containing 300 units of insulin. With one pen you can inject several doses of insulin. Using this syringe pen, you can administer a dose with an accuracy of 1 unit. You can administer from 1 to 60 units per injection. If your dose is more than 60 units, you will need to give more than one injection. With each injection, the piston moves only slightly, and you may not notice a change in its position. The plunger will only reach the bottom of the cartridge when you have used up all 300 units contained in the pen.
The syringe pen cannot be shared with other people, even when using a new needle. Do not reuse needles. Do not share needles with other people. The needle can transmit infection, which can lead to infection.
It is not recommended for use in patients with low vision or complete loss of vision without the assistance of well-visioned people trained in the correct use of the pen.
To perform the injection you need:
KwikPen™ syringe pen with insulin.
QuickPen™ pen (Becton, Dickinson and Company (BD) pen needles are recommended).
— A swab soaked in alcohol.
Preparing a syringe pen for insulin administration:
— Wash your hands with soap.
— Check your pen to make sure it contains the type of insulin you need. This is especially important if you use more than 1 type of insulin.
— Do not use pens that have expired, which is indicated on the label.
— Always use a new needle to prevent infections and to avoid needles becoming clogged.
| Stage 1: — Remove the cap of the syringe pen. — Do not remove the label of the syringe pen. — Wipe the rubber disc with a swab soaked in alcohol. |
| Stage 2 (only for Humalog Mix 25 and Humalog Mix 50): — Carefully roll the syringe pen between your palms 10 times. AND |
| — Turn the syringe pen over 10 times. Stirring is important for dose accuracy. The insulin should appear uniform. |
Stage 3:
— Check the appearance of the insulin.
Humalog® should be clear and colorless. Do not use if it is cloudy, discolored, or contains particles or clumps.
Humalog® Mix 25 should be white and cloudy after mixing. Do not use if it is clear or contains particles or clumps.
| Stage 4: — Take a new needle. — Remove the paper sticker from the outer needle cap. | |
| Stage 5: — Place the cap with the needle directly on the syringe pen and turn the needle with the cap until it is tightly fixed | |
| Stage 6: — Remove the outer needle cap. Don't throw it away. — Remove the inner needle cap and discard it. |
Checking the syringe pen for drug intake
This check should be carried out before each injection.
— Checking the syringe pen for the supply of the drug is carried out to remove air from the needle and cartridge, which may accumulate during normal storage, and to ensure the proper operation of the syringe pen.
- If do not do this check before each injection, you may give either too low or too high a dose of insulin.
| Stage 7: — To check the syringe pen for drug delivery, set 2 units by rotating the dose button. | |
| Stage 8: — Hold the pen with the needle pointing up. Lightly tap the cartridge holder to collect air bubbles at the top. | |
| Stage 9: — Continue holding the pen with the needle pointing up. Press the dose button until it stops and an “O” appears in the dose indicator window. While holding the dose button, slowly count to 5. You should see insulin at the tip of the needle. — If does not appear at the tip of the needle, repeat the steps of checking the syringe pen for drug delivery. The check can be carried out no more than 4 times. — If insulin still does not appear, change the needle and repeat checking the syringe pen for drug delivery. |
The presence of small air bubbles is normal and does not affect the administered dose.
Dose selection
- You can administer from 1 to 60 units per injection.
— If your dose is more than 60 units, you will need to give more than one injection.
— If you need help dividing your dose correctly, contact your doctor.
— For each injection, you should use a new needle and repeat the procedure for checking the syringe pen for drug delivery.
| Stage 10: · To dial the dose of insulin you need, turn the dose button. The dose indicator should be in line with the number of units corresponding to your dose. |
| — With one turn, the dose button moves by 1 unit. — Each time you turn the dose button, a click is heard. - Do NOT select the dose by counting the clicks as this may result in the wrong dose being dialed. — The dose can be adjusted by turning the dose button in the desired direction until the number corresponding to your dose appears in the dose indicator window in line with the dose indicator. — Even numbers are indicated on the scale. |
— Odd numbers, after the number 1, are indicated by solid lines.
— Always check the number in the dose indicator window to ensure the correct dose.
— If there is less insulin left in the syringe pen than you need, you will not be able to administer the dose you need using this syringe pen.
— If you need to inject more units than are left in the pen, you can:
— inject the amount remaining in your pen, and then use a new pen to administer the rest of the dose, or
- take a new syringe pen and inject the full dose.
There may be a small amount of insulin left in the pen that you cannot inject.
Carrying out the injection
— Inject insulin strictly in accordance with what your doctor has indicated.
- Change (alternate) injection sites with each injection.
- Do not try to change the dose during the injection.
| Stage 11: — Choose the injection site. Insulin is injected under the skin (subcutaneously) into the anterior abdominal wall, buttocks, thighs, or shoulders. — Prepare the skin as recommended by your doctor. | |
| Stage 12: — Insert the needle under the skin. — Press the dose button all the way. -Hold down the dose button and slowly count to 5, then remove the needle from the skin. |
Do not attempt to inject insulin by turning the dose button. When you rotate the dose button, insulin NOT flow.
Stage 13:
- Remove the needle from the skin.
— It is normal if there is a drop of insulin left on the tip of the needle. This does not affect the accuracy of your dose.
— Check the number in the dose indicator window.
— If the dose indicator window shows “0,” it means that you have administered the dialed dose in full.
| — If you do not see “0” in the dose indicator window, you should not dial the dose again. Insert the needle under the skin again and complete the injection. — If you still think that the dose you have taken has not been administered in full, do not inject again. Check your blood glucose levels and act as directed by your healthcare provider. |
- If you need to give 2 injections to administer the full dose, do not forget to give the second injection.
With each injection, the piston moves only slightly, and you may not notice a change in its position.
If you notice a drop of blood after removing the needle from the skin, gently apply a clean gauze pad or alcohol swab to the injection site. Do not rub this area.
After injection
| Stage 14: Carefully replace the outer needle cap. | |
| Stage 15: — Unscrew the needle together with the cap and dispose of it as described below (see section “Disposal of syringe pens and needles”). — Do not store the pen with a needle attached to avoid insulin leakage, clogging of the needle, and air entering the pen. | |
| Stage 16: Place the cap on the pen by aligning the cap clamp with the dose indicator and pressing it. |
Storing a syringe pen
Unused syringe pens
— Store unused pens in the refrigerator at a temperature between 2°C and 8°C.
— Do not freeze the insulin you use. If it has been frozen, do not use it.
— Unused pens can be stored until the expiration date stated on the label if stored in the refrigerator.
Syringe pen currently in use
— Do not store the pen you are currently using in the refrigerator. A syringe pen that is in use should not be stored in the refrigerator; it should be stored at a temperature not exceeding 30°C for no more than 28 days in a place protected from heat and light.
— When the expiration date indicated on the package expires, the used syringe pen must be thrown away, even if there is insulin left in it.
General information about the safe and effective use of pen syringes
— Keep the syringe pen and needles out of the reach of children.
— Do not use the pen if any part of it appears broken or damaged.
— Always carry a spare pen with you in case your pen gets lost or broken.
Troubleshooting
— If you cannot remove the cap from the syringe pen, carefully twist it and then pull the cap.
— If the dose dial button is difficult to press:
— Press the dose dial button more slowly. By slowly pressing the dose dial button it is easier to inject.
— The needle may be blocked. Insert a new needle and check the syringe pen for drug delivery.
— Dust or other substances may have gotten inside the syringe pen. Throw away this syringe pen and get a new one.
If you have any questions or concerns about using the QuickPen™, please contact Eli Lilly or your healthcare provider.
Side effects of the drug Humalog mix
Allergic reaction, injection site reaction, lipodystrophy, itching, rash, hypoglycemia. Hypoglycemia is the most common side effect of insulin therapy in patients with diabetes. Severe hypoglycemia can lead to loss of consciousness and, in some cases, death. Local allergies in patients may manifest themselves as redness, swelling or itching at the injection site. These minor reactions usually disappear after a few days or weeks. In some cases, these reactions may be due to factors other than insulin, such as detergents that irritate the skin or improper administration technique. Systemic allergy is very rare but is a potentially more serious side effect and is a generalized form of allergic reaction to insulin that can manifest as a rash over the entire body, shortness of breath, wheezing, decreased blood pressure, increased heart rate and sweating. Severe cases of generalized allergies are life-threatening.
Special instructions for the use of Humalog Mix
Humalog Mix 25 differs from other insulin mixtures in that this mixture contains fast-acting insulin lispro. Patients using Humalog Mix 25 may require dosage adjustments. Hypoglycemia is the most common side effect of insulin medications, including Humalog Mix 25. Early warning signs of hypoglycemia may be different or less severe in certain conditions, such as long-term diabetes or during intensive diabetes therapy. Any changes in insulin treatment should be made with caution and only under medical supervision. Changes in insulin dosage, brand (manufacturer), type (e.g., Regular), variety (bovine, porcine, porcine, human, human insulin analog), and/or production method may require dosing changes. During times of illness or emotional distress, insulin requirements may be increased. In the presence of renal or liver failure, the need for insulin may be reduced. Dose adjustments may be necessary if patients change their physical activity or their usual diet. Clinical studies regarding the use of Humalog Mix 25 during pregnancy have not been conducted. Patients with diabetes should inform their doctor if they are pregnant or planning to become pregnant. Patients who are breastfeeding may require adjustments in insulin dosage and/or diet. There is no information whether insulin lispro or protamine lispro suspension is excreted in human milk in clinically significant amounts. Many medications, including human insulin, are secreted into breast milk. Children The safety and effectiveness of Humalog Mix 25 in patients under 18 years of age have not been studied. When insulin was used in recommended therapeutic doses, no effects were noted on the ability to drive a car or operate complex machinery. The ability to concentrate and the speed of psychomotor reactions may be reduced due to hypoglycemia.
Indications, contraindications, side effects and other nuances
The instructions for the drug Insulin Humalog contain the following points:
- Indications: T1DM, T2DM, gestational diabetes, acute subcutaneous insulin resistance, uncorrectable postprandial hyperglycemia, accidentally acquired disease that complicates the course of diabetes, surgical operation for a diabetic patient.
- Contraindications: hyperglycemic conditions, increased individual sensitivity.
- Side effects - temporary insulin presbyopia of the lens, insulin swelling and typical hypoglycemic symptoms:
- headache;
- unnatural pallor of the skin;
- perspiration, increased profuse sweating;
- increased heart rate and heart rate;
- tremor of the limbs, muscle spasms, myoclonic twitching, paresthesia and various types of paresis;
- decrease in intellectual functions;
- sleep disorders;
- anxiety.
A glucagon injection must be included in a diabetic's personal first aid kit.
- Overdose – hypoglycemic precoma and coma. These conditions are treated with subcutaneous or intramuscular administration of glucagon. If there is no such drug or the desired effect is not obtained as a result of its use, an emergency injection of a ready-made glucose solution into a vein is performed.
- Cautions. In patients with problem kidneys and liver, during intense physical activity, in the absence of carbohydrates in food, as well as when treated with beta-blockers, sulfonamides or MAO inhibitors, when taking alcohol or alcohol-containing medications, the need for the drug may be underestimated. An increase in dose may be required during an infectious disease, with emotional distress, with a diet disorder, during therapy with thiazide diuretics, oral contraceptives, tricyclic antidepressants and glucocorticosteroids.
- Dosage. Lispro (Humalog) is injected under the skin, 4 to 6 times a day. The single dose, quantity and time of each injection are selected by the endocrinologist. A single injection with a dose higher than 40 units is allowed only in special cases. When switching to Lispro monotherapy from fast-acting porcine analogues, dosage adjustments may be required. During delivery and immediately after it, the dosage of the drug is recommended to be significantly reduced. A breastfeeding new mother with diabetes may also need dosage and/or diet adjustments.
- Features of storage and use. Insulin medications should be stored on the bottom shelf of the refrigerator. Before administration, the dose is “warmed up” by rolling it between the palms 10 to 20 times. You should also ensure that the injection does not enter a blood vessel.
Warning! When administering a cold drug, when alcohol gets under the skin, or simply due to its anabolic local effect, the formation of a cosmetic defect (lipohypertrophy) is possible, which reduces the absorption of the drug. Therefore, when making injections, you need to constantly change the location of the injections, and when punctures are in one area, for example, on the stomach, leave a distance of 1 cm between them.
Interactions of the drug Humalog mix
The need for insulin may increase when taking drugs with hyperglycemic activity, such as oral contraceptives, corticosteroids or thyroid hormone replacement therapy. Insulin requirements may be reduced by the use of oral hypoglycemic agents, salicylates, sulfonamides and some antidepressants (MAO inhibitors), ACE inhibitors and angiotensin II receptor blockers. Before using other medications in addition to Humalog Mix 25, you should consult your doctor.
Overdose of the drug Humalog mix, symptoms and treatment
Insulin overdose can cause hypoglycemia with associated symptoms, which may include apathy, confusion, palpitations, sweating, vomiting and headache. Hypoglycemia can develop due to excess insulin activity and a mismatch between food intake and energy expenditure, or both. Mild episodes of hypoglycemia can usually be treated with oral glucose. There may be a need for dose adjustment, changes in diet and physical activity. More severe episodes with coma, seizures, or neurological damage are treated with IM or SC administration of glucagon or concentrated IV glucose. Continued carbohydrate intake and evaluation may be necessary as hypoglycemia may recur after apparent clinical recovery.