RELEVANCE
Elderly and senile people are characterized by a high prevalence of osteoporosis, which increases the risk of fractures, also recurrent ones.
Fractures that occur with osteoporosis in old age lead to catastrophic consequences and are an unfavorable complication of the disease. The prevalence of osteoporotic fractures increases progressively with increasing age. Currently, the cumulative incidence of hip fractures in women over 80 years of age is about 30% [1]. The proportion of vertebral body fractures in women over 80 years of age is up to 40% of all vertebral osteoporotic fractures [2]. Osteoporosis and osteoporotic fractures remain a serious medical, economic and social problem to this day, despite the enormous advances made in the diagnosis and treatment of this disease. When working with elderly and senile patients with osteoporosis, great attention should be paid to their functional activity and the presence of senile asthenia syndrome (SA), or “frailty”. This is a “comprehensive” geriatric syndrome characterized by an age-associated decrease in the physiological reserve and functions of many body systems, leading to increased vulnerability of the elderly person’s body to the effects of endo- and exogenous factors, with a high risk of adverse health outcomes, loss of autonomy and death [3 ].
For screening assessment of the geriatric status of an elderly patient, the “Age is not a hindrance” questionnaire, consisting of 7 questions, is recommended (Table 1). Patients with a score of 5 or more on this questionnaire are recommended to be referred to the geriatric office for a comprehensive geriatric assessment and development of an individual management plan. Patients with a score of 3–4 points are recommended to undergo a short battery of tests of physical functioning to clarify geriatric status [3].
Table 1. Questionnaire “Age is not a barrier”
| 1 | Have you lost 5 kg or more in the last 6 months? | Not really |
| 2 | Do you experience any limitations in your daily activities due to decreased vision or hearing? | Not really |
| 3 | Have you had a fall-related injury within the last year? | Not really |
| 4 | Have you been feeling depressed, sad or anxious in recent weeks? | Not really |
| 5 | Do you have problems with memory, comprehension, orientation, or ability to plan? | Not really |
| 6 | Do you suffer from urinary incontinence? | Not really |
| 7 | Do you have difficulty moving around the house or outside? (Walk up to 100 meters or climb 1 flight of stairs) | Not really |
A number of studies have found that SA is associated with an increased risk of falls, a decrease in bone mineral density, a deterioration in the quality of life, functional capabilities and, accordingly, an increase in mortality in patients with this condition [4]. This, in turn, increases the risk of spontaneous falls: in older people, the frequency of falls increases by 10% every 10 years. Falls cause serious injuries in 10–15% of cases, and fractures in 5% of cases [5].
There is a direct relationship between the number of previous fractures and the likelihood of developing new fractures - the so-called “fracture cascade” in osteoporosis. Moreover, the risk of a recurrent fracture is significantly higher if fractures in typical osteoporosis localizations (proximal femur, vertebrae and shoulder) have previously been noted.
Elderly patients with osteoporotic fractures should be classified as “frail” elderly with a high risk of recurrent fractures and decreased functional activity, quality of life, and increased mortality [6].
Despite the increasing incidence of osteoporosis and its complications in older people, this disease remains underdiagnosed and underestimated, especially in people over 80 years of age. Elderly patients aged 80+ have been rarely included in known randomized clinical trials (RCTs), and patients with AS have not been described in any osteoporosis studies.
A serious problem in the treatment of osteoporosis in older people is the ineffectiveness of antiresorptive therapy due to age-related decrease in bone formation. There are frequent cases of continued decrease in bone density and the occurrence of recurrent fractures during osteoporosis therapy [7].
Prevention of recurrent fractures in geriatric patients is a system of preventive, rehabilitation and therapeutic measures aimed at reducing the risk of falls, choosing effective therapy, and reducing the risk of recurrent fractures.
Teseo
Infectious and parasitic diseases
uncommon: urinary tract infections, including cystitis, upper respiratory tract infections, including pharyngitis and sinusitis; rarely: sepsis, including death.
Disorders of the blood and lymphatic system: uncommon: anemia; rarely: eosinophilia, thrombocytopenia.
Immune system disorders
rarely: anaphylactic reaction, hypersensitivity.
Metabolic and nutritional disorders
uncommon: hyperkalemia; rarely: hypoglycemia (in patients with diabetes mellitus).
Mental disorders:
uncommon: insomnia, depression; rarely: anxiety.
Nervous system disorders: uncommon: fainting; rarely: drowsiness.
Violations of the organ of vision: rarely: visual disturbances.
Hearing and labyrinthine disorders: uncommon: vertigo.
Cardiac disorders: uncommon: bradycardia; rarely: tachycardia.
Vascular disorders
uncommon: marked decrease in blood pressure, orthostatic hypotension.
Respiratory, thoracic and mediastinal disorders
uncommon: shortness of breath, cough; very rare: interstitial lung disease. Gastrointestinal disorders
uncommon: abdominal pain, diarrhea, dyspepsia, flatulence, vomiting; rarely: dry mouth, discomfort in the stomach, disturbance of taste. Liver and biliary tract disorders: rare: liver dysfunction/liver damage.
Skin and subcutaneous tissue disorders
uncommon: skin itching, hyperhidrosis, rash; rare: angioedema (also fatal), eczema, erythema, urticaria, drug rash, toxic skin rash.
Musculoskeletal and connective tissue disorders: uncommon: back pain (sciatica), muscle spasms, myalgia; rare: arthralgia, pain in limbs, pain in tendons
(tendenitis-like syndrome).
Renal and urinary tract disorders
uncommon: renal dysfunction, including acute renal failure.
General and administration site disorders
uncommon: chest pain, asthenia (weakness); rarely: influenza-like syndrome. Influence on the results of laboratory and instrumental studies is infrequent: increased concentration of creatinine in blood plasma; rarely: decreased hemoglobin content, increased uric acid in the blood plasma, increased activity of liver enzymes and creatine phosphokinase (CPK).
Overdose.
Symptoms: the most pronounced manifestations of overdose were a marked decrease in blood pressure and tachycardia, bradycardia was also reported,
dizziness, increased serum creatinine concentrations and acute renal failure.
Treatment: telmisartan is not eliminated by hemodialysis. Patients should be carefully monitored and treated symptomatically as well as supportively. The treatment approach depends on the time elapsed after taking the drug and the severity of symptoms. Recommended measures include inducing vomiting and/or gastric lavage; it is advisable to take activated charcoal. Plasma electrolytes and creatinine levels should be regularly monitored. If a pronounced decrease in blood pressure occurs, the patient should take a horizontal position with raised legs, and it is necessary to quickly replenish the volume of blood volume and electrolytes.
CASE DESCRIPTION
Patient T., 89 years old, complained of pain in the bones, thoracic and lumbar spine, aggravated by movements, difficulty walking, fear of falling, memory loss, loss of appetite, and urinary incontinence.
From the anamnesis it is known that menopause occurred at 42 years old, she did not receive glucocorticosteroids, there were no episodes of poor nutrition or malabsorption syndrome during her life, she does not limit dairy products. From the age of 69 years, she suffered multiple fractures that occurred with minimal trauma: at 69 years old - a fracture of the right radius, from 70 to 75 years old - compression fractures ThXI and LI, at 78 years old - a fracture of the neck of the right femur (endoprosthetics), at 83 years old – ThIX and LIII, at 88 years old – ThXII.
The mother denies any fractures, but recalls that she had severe kyphosis in old age.
Among the concomitant diseases, hypertension is noteworthy, for which he constantly takes perindopril 5 mg per day, torsemide 10 mg per day.
The diagnosis of osteoporosis was made at the age of 78 years, when, after compression fractures of the vertebral bodies were identified, densitometry was performed, which showed a decrease in bone mineral density (BMD) according to the T-criterion in the vertebrae to –4.9 SD (Table 2).
Table 2. Dynamics of laboratory and instrumental blood parameters of patient T. initially and during anti-osteoporotic treatment
| Parameter | 78 years old | 88 years old (10 years of antiresorptive therapy) | 89 years old (12 months of teriparatide therapy) | Reference values, units of measurement |
| Total calcium | 2,21 | 2,22 | 2,36 | 2.15–2.55 mmol/l |
| Phosphorus | 1,10 | 1,12 | 1,03 | 0.87–1.45 mmol/l |
| Creatinine | 86 | 84 | 81 | 44.0–80.0 µmol/l |
| Alkaline phosphatase | 69 | 40 | 83 | 0–240 U/l |
| Parathyroid hormone | – | 78,9 | 39,2 | 15–65 pg/ml |
| 25(OH)D3 | – | 8,9 | 44,9 | Target value from 30 ng/ml |
| Type 1 collagen C-terminal telopeptide (Ctx) | – | 0,01 | 0,127 | 0.01–0.28 ng/ml |
| Procollagen type 1 N-terminal propeptide (P1NP) | – | 12,3 | 106,7 | 15–115 ng/ml |
| Osteocalcin | 8,0 | 46,4 | 15–46 ng/ml | |
| L1 | –4,1 | –3,7 | –2,6 | T-test, SD |
| L2 | –4,4 | –3,3 | –2,7 | T-test, SD |
| L3 | –4,9 | –4,0 | –2,9 | T-test, SD |
| L4 | –4,1 | –3,2 | –3,1 | T-test, SD |
| L1–L4 | –4,9 | –3,9 | –3,1 | T-test, SD |
| Neck | –3,7 | –2,7 | –2,4 | T-test, SD |
| Total hip | –3,0 | –2,8 | –2,3 | T-test, SD |
| FRAX for all fractures | 46 | 23 | 19 | % |
| FRAX for hip fractures | 29 | 17 | 11 | % |
The 10-year FRAX fracture risk at diagnosis was 46% for all fractures and 29% for hip fractures. For 5 years, the patient received antiresorptive therapy with alendronate, then for two years with an oral form of ibandronate, then three consecutive infusions of zoledronic acid were performed, however, repeated low-traumatic fractures occurred during this therapy. Periodically took combined calcium and vitamin D supplements.
The patient lives with her daughter in a 3-room apartment (7th floor of a 10-story building) in a separate room. Moves around the apartment independently without a cane. Goes outside, accompanied by relatives, 1–2 times a week, and uses a cane while walking. Relatives prepare food and buy groceries. Meals – 2-3 times a day. Medicines are taken under the supervision of relatives according to the list. Specialized secondary education, technologist by profession.
Examination results at the age of 88 years (2017).
Height 153 cm (height loss since youth 8 cm), weight 49 kg, BMI = 20.9 kg/m2.
The result of the assessment on the “Age is not a hindrance” questionnaire is 4 points (presence of injuries associated with a fall, decreased memory and planning ability, urinary incontinence, difficulties in movement).
The result of a short battery of tests of physical functioning, including a balance test (feet together, semi-tandem position and tandem foot position), a walking speed test and a 5-hands-free chair rise test, was 6 points, indicating the presence of in a patient with SA syndrome.
Next, a comprehensive geriatric assessment (CGA) was carried out, including an assessment of physical health, functional status, cognitive function, emotional state and social status (Table 3).
Table 3. Comprehensive geriatric assessment of patient T.
| Test | Result | Interpretation |
| Brief nutrition rating scale, points | 22,5/30 | Risk of developing malnutrition |
| Basic functional activity (Barthel index), points | 90/100 | Moderate dependence on outside help |
| Instrumental functional activity (Lawton scale), points | 4/8 | Significant reduction in instrumental activity |
| Walking speed, m/s | 0,7 | Decreased mobility and imbalance. High risk of falls |
| Test "Get up and go", with | 16 | |
| Ability to maintain balance, with | “feet together” for more than 10 s semi-tandem position – 3 s | |
| Hand dynamometry, kg | right hand – 22 left hand – 16.5 | Carpal muscle strength is at the lower limit of normal |
| Clock drawing test, scores | 10/10 | Moderate cognitive disorder of multifunctional non-amnestic origin |
| Brief mental status scale, points | 28/30 | |
| Montreal Cognitive Rating Scale, points | 25/30 | |
| Geriatric Depression Scale, scores | 4/15 | Low risk of depression |
Assessment of physical health showed the presence of stress urinary incontinence, 2 episodes of falls over the past year - at home and outside the home - during the day, decreased vision in both eyes, the presence of orthostatic hypotension, chronic pain syndrome (pain in the lumbar spine, which lasted more than 3 months, with an intensity of up to 8 points on a visual analogue scale) and the presence of a risk of developing malnutrition. Difficulties in chewing food, especially meat, were identified, associated with poorly fitted dentures.
The patient's functional status corresponded to moderate dependence on outside assistance (requires assistance with climbing stairs, moving outside the home, housekeeping, taking medications, preparing food). Decreased walking speed, impaired balance and a history of repeated falls indicated a high risk of future falls; the risk of falls on the Morse scale was also high, amounting to 65 points. The results of tests to assess cognitive functions were consistent with moderate cognitive impairment of multifunctional non-amnestic origin as part of cerebrovascular disease. Assessment of emotional state did not reveal signs of depressive disorder.
The geriatrician gave recommendations on nutrition (a varied diet with sufficient protein content - at least 70 g per day, the use of additional nutrition in the form of sipping), drinking regimen (about 1.5 liters per day), classes with a physical therapy instructor (exercises for training balance and muscle strength), recommendations for home improvement to reduce the risk of falls, selection of shoes, cognitive training, consultations with an ophthalmologist and an orthopedic dentist were recommended, drug therapy was adjusted (withdrawal of torasemide taking into account urinary incontinence and the presence of orthostatic hypotension, increasing the dose of perindopril to 10 mg – target blood pressure level is defined at 135–145/70–80 mmHg).
The examination revealed a pronounced deficiency of vitamin D3 (25(OH)D3) (8.9 ng/ml with an increase in PTH to 78 pg/ml), and therefore, at the first stage, correction was carried out by taking an oil solution of colecalciferol 50,000 IU 2 times per week for 6 weeks, with levels maintained by taking 15,000 IU per week, and a combination of calcium carbonate (500 mg) and vitamin D3 (200–400 IU) was taken daily.
To assess the possibility of continuing and predicting the effect of further antiresorptive therapy, bone metabolism markers were assessed, the levels of which were low: osteocalcin - 8.0 ng/ml (11-43), C-terminal telopeptide of type 1 collagen (CTX) - 0.01 ng/ml (0.01–0.28), N-terminal propeptide of type 1 procollagen (P1NP) – 12.3 ng/ml (15–115).
Taking into account the laboratory and instrumental studies, the patient was diagnosed with severe senile osteoporosis with the presence of multiple pathological fractures of the skeleton. The 10-year risk of fracture according to FRAX is 46%. Vitamin D deficiency. Senile asthenia syndrome.
Taking into account the complete suppression of bone metabolism, the persistence of low BMD, a significant decrease in CTX during 11 years of treatment with bisphosphonates and, despite this, new severe low-energy fractures that occurred, the effectiveness of further use of antiresorptive drugs was assessed as low and the patient was prescribed teriparatide 20 mcg daily subcutaneously .
The first injection of the drug was given under the guidance of a nurse, the patient’s relatives were trained, and the patient carried out further injections independently under the guidance of relatives.
During 11 months of treatment, there were no new fractures, while the patient noted an increase in tolerance to physical activity and a significant decrease in pain in the lumbar spine - up to 5 points on a visual analogue scale. Surgical treatment was performed to replace the lens of the left eye, glasses were selected and dentures were replaced. The patient increased her physical activity: she began to walk every day for at least half an hour a day.
When performing CGO over time a year later, a slight increase was noted in mobility (walking speed 0.8 m/s, “Stand up and walk” test 15 s) and hand muscle strength of the patient (right hand 24 kg, left hand 19 kg), as well as improvement in nutritional status (the patient gained 2 kg of weight, the Brief Nutritional Scale score was 24/30 points). Assessment of cognitive function showed no deterioration. The emotional state remained stable.
The result of an X-ray densitometric study after 12 months of treatment with teriparatide is presented in Figure 2. A decision was made to continue therapy with teriparatide for another 6–8 months, followed by transferring the patient to antiresorptive therapy (denosumab).
The main results of treatment of the patient with teriparatide were the absence of new fractures, reduction of back pain, and increase in functional status.
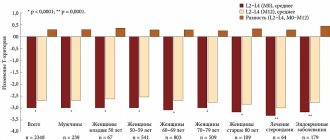
Densitometry revealed an increase in BMD in the vertebrae by +21% (up to –3.1 SD), in the hip by +4% (–2.3 SD). Osteocalcin increased by +580%, P1NP (+867%) and CTX +1270% increased significantly, which reflects the activation of bone metabolism under the influence of teriparatide (Table 2).
Teriparatide
International name of the medicinal substance:
Teriparatide The list of drugs containing the active substance Teriparatide is given after the description.
Pharmacological action:
Parathyroid hormone analogue, which is a sequence of 84 amino acid residues, is the main regulator of Ca2+ and phosphorus metabolism in bone tissue and kidneys.
Teriparatide is an active fragment of endogenous human parathyroid hormone. The physiological effect of parathyroid hormone is to stimulate bone formation through a direct effect on osteoblasts. Indirectly increases intestinal absorption and tubular reabsorption of Ca2+, as well as phosphate excretion by the kidneys. The biological effect of parathyroid hormone is carried out by binding to specific receptors on the surface of cells. Teriparatide binds to the same receptors and has the same effect on bone tissue and kidneys as parathyroid hormone. Single daily administration of teriparatide stimulates the formation of new bone tissue on the trabecular and cortical (periosteal and/or endosteal) surfaces of bones with preferential stimulation of osteoblast activity relative to osteoclast activity. This is confirmed by an increase in the content of markers of bone tissue formation in the blood serum: bone-specific ALP and procollagen-1 carboxy-terminal propeptide. An increase in the content of bone tissue formation markers is accompanied by a secondary increase in the concentration of bone resorption markers in urine: N-telopeptide and deoxypyridinoline, which reflects the physiological interaction of the processes of bone tissue formation and resorption in skeletal remodeling. 2 hours after administration of teriparatide, a short-term increase in the concentration of serum Ca2+ is observed, which reaches maximum values after 4-6 hours and returns to the initial level within 16-24 hours. In addition, transient phosphaturia and a slight short-term decrease in the concentration of phosphorus in the blood serum may be observed. . During treatment with teriparatide, bone mineral density (BMD) of the whole body increases by 5-10% (including the lumbar spine, femoral neck and femur). Mineralization processes occur without signs of toxic effects on bone tissue cells, and bone tissue formed under the influence of teriparatide has a normal structure (without the formation of reticulofibrous bone tissue and bone marrow fibrosis). Teriparatide reduces the risk of fractures regardless of age, baseline bone turnover, or BMD (relative reduction in the risk of new fractures is 65%). Pharmacokinetics:
Well absorbed after subcutaneous administration. Absolute bioavailability - 95%. Volume of distribution - 1.7 l/kg. TCmax - 30 minutes after subcutaneous administration of 20 mcg of the drug, Cmax exceeds 4-5 times the upper limit of the normal concentration of parathyroid hormone, followed by its decrease to undetectable values within 3 hours. T1/2 - 1 hour. Metabolized in the liver through nonspecific enzymatic mechanisms followed by excretion through the kidneys. Like endogenous parathyroid hormone, teriparatide does not accumulate in bones or other tissues. There was no effect of age (age group from 31 to 85 years) on the pharmacokinetics of teriparatide. In patients with mild or moderate chronic renal failure (creatinine clearance 30-72 ml/min), the pharmacokinetics do not change.
Indications:
Treatment of osteoporosis in postmenopausal women.
Treatment of primary osteoporosis or osteoporosis caused by hypogonadism in men. Contraindications:
Hypersensitivity, previous hypercalcemia, severe chronic renal failure, metabolic bone diseases, with the exception of primary osteoporosis (including hyperparathyroidism and Paget's disease), increased ALP activity of unknown origin, previous radiation therapy of skeletal bones, history of bone metastases or bone tumors, pregnancy, period lactation, age up to 18 years. With caution.
Urolithiasis (in the acute stage or recently suffered); Moderate chronic renal failure, hypovitaminosis D, hypocalcemia (clinically significant), simultaneous use of cardiac glycosides. Side effects:
Most often (more than 10%): pain in the extremities.
Common (more than 1% and less than 10%): anemia, hypercholesterolemia, depression, headache, dizziness, sciatica, palpitations, shortness of breath, dyspnea, nausea, vomiting, increased sweating, muscle cramps, general weakness, chest pain, asthenia. Rarely (more than 0.1% and less than 1%): tachycardia, decreased blood pressure, emphysema, urinary incontinence, polyuria, painful urge to urinate, erythema and irritation at the injection site. Overdose. Symptoms: prolonged hypercalcemia, orthostatic collapse, nausea, vomiting, dizziness, headache. Treatment: drug withdrawal, monitoring serum Ca2+ concentration, symptomatic therapy. There is no specific antidote. Interaction:
No clinically significant interaction with hydrochlorothiazide and furosemide was observed.
Co-administration of teriparatide with raloxifene or hormone replacement therapy does not affect the concentration of Ca2+ in serum and urine. A single administration of teriparatide has no effect on the pharmacodynamics of digoxin. Hypercalcemia is a predisposing factor to the development of intoxication with digitalis preparations. Special instructions:
In case of a break in treatment with the drug, patients can continue treatment with other drugs.
Additional administration of calcium and vitamin D is recommended in case of insufficient dietary intake. Blood sampling to determine the concentration of Ca2+ in the blood should be done no earlier than 16 hours after the last administration of the drug, due to possible short-term hypercalcemia after administration of teriparatide. Constant monitoring of Ca2+ concentrations during treatment is not required. When taking the drug, rare episodes of short-term orthostatic hypotension may occur, which occur within 4 hours after administration of the drug and go away on their own within a few minutes to several hours (the patient must be placed in a horizontal position, lying on his back) and are not a contraindication for further administration drug. Due to the lack of clinical data on long-term treatment with teriparatide, the recommended treatment period should not exceed 18 months. The drug should not be used if the solution in the syringe pen is cloudy, colored or contains foreign particles. Preparations containing the active substance Teriparatide:
Forsteo
The information provided in this section is intended for medical and pharmaceutical professionals and should not be used for self-medication. The information is provided for informational purposes only and cannot be considered official.
DISCUSSION
Management of patients with SA syndrome requires a particularly careful weighing of risks and benefits, since often aggressive treatment, frequent hospitalizations, excessive diagnostic procedures, massive drug therapy in non-life-threatening situations can lead to an excess of the risk over the benefits of such measures and to a decrease in functional status and quality of life of the patient.
Assessment of the geriatric status of elderly patients should be multifaceted and include information about the presence of medical problems, functional abilities, cognitive function, the presence of emotional disorders, and social problems of the patients. A comprehensive assessment is important for the development and organization of management and rehabilitation plans, and the determination of goals for long-term medical care, including at the final stage of life.
The examination methods presented in Table 4 are based on a domain-specific geriatric approach, designed for routine use in everyday medical practice by doctors and nurses and do not require extensive training. This domain assessment is not required for every patient encounter, but should be scheduled as part of the annual assessment and when clinically indicated. At a minimum, during the consultation it is necessary to find out what the patient’s functional capabilities are, as well as assess the state of his cognitive functions. The main purpose of such an assessment is to discover the patient's problems or needs that can be corrected. For example, early recognition of the need for mobility aids, nutritional intervention, identification of cognitive impairment, or the need for self-care support may be fundamental in older patients and lead to improved clinical outcomes.
Table 4. Components of a comprehensive geriatric assessment
| Domain | Domain Components | Assessment Tools |
| Physical health | Chronic diseases | Anamnesis and medical documentation data |
| Vision and hearing | Whisper speech test Rosenbaum table | |
| Orthostatic hypotension | Orthostatic test | |
| Anthropometry | Height and weight measurement | |
| Nutrition status | Body mass index | |
| Brief Nutritional Rating Scale | ||
| Drug therapy | STOPP/START criteria Algori Anticholinergic load scale | |
| Availability of required vaccinations | Medical history, outpatient card data | |
| Functional activity | Basic functional activity | Barthel Index |
| Instrumental functional activity | Lawton scale | |
| Mobility | Test "Get up and go" Walking speed Balance Test Brief Physical Functioning Test Battery | |
| Muscle strength | Carpal dynamometry | |
| Mental health | Cognitive functions | Clock drawing test Mini Cog Mini Mental Status Rating Scale Montreal Cognitive Rating Scale Frontal Dysfunction Test Battery |
| Emotional condition | Geriatric Depression Scale Health rating scale Cornell Depression Scale | |
| Socio-economic problems | · Marital status, presence of a spouse or partner · Circle of communication and social contacts · Living conditions · Financial opportunities · Work activity, profession · Education · The ability to engage in normal activities – cleaning the house, cooking, shopping for groceries, etc. · Patient care needs and preferences related to care · Loss of loved ones, stress that has happened in life, psychological problems, the ability to cope with them and with psychological problems · Alcohol abuse, drug addiction among loved ones and people around the patient · Religiosity · Cruel treatment · Household safety | |
The presented clinical example presents an elderly patient with SA syndrome and severe osteoporosis, aggravated by multiple pathological fractures. Vitamin D3 deficiency plays an important role in the pathogenesis of both osteoporosis and SA syndrome and sarcopenia. Prospective epidemiological studies have shown that vitamin D3 deficiency in old age is associated with cognitive decline and an increased risk not only of AS syndrome, but also of cognitive impairment, including Alzheimer's disease. A reduction in vitamin D3 levels below 10 ng/ml is considered critical in this regard [8]. A decrease in the concentration of vitamin D3 in elderly and senile age occurs due to a decrease in the absorption of calcium in the intestines, a decrease in its intake from food, and a slowdown in its formation in the skin from provitamin D3. The greatest significance in the pathogenesis of senile osteoporosis is the deficiency of active metabolites of vitamin D due to a decrease in its synthesis in the kidneys. In senile osteoporosis, various manifestations of resistance to vitamin D3 also play a role - i.e. deficiency of 1,25(OH)2D3 receptors. These changes cause the development of transient hypocalcemia, a negative calcium balance in the body, which leads to proliferation of parathyroid cells and increased production of parathyroid hormone, which is compensated by bone resorption [9]. Deficiency of sex hormones in old age, together with a lack of active metabolites of vitamin D3, leads to muscle weakness, disorders of neuromuscular conduction, coordination of movements and the development of cognitive impairment [10]. These phenomena contribute to an increased incidence of falls in older people and an increased risk of bone fractures, among which the most serious are fractures of the proximal femur. In this clinical example, the patient was diagnosed with a severe deficiency of vitamin D3, which was corrected by taking cholecalciferol to target values.
In older people, a priori, the risk of falls and associated fractures is higher than in young and middle age. Therefore, it is recommended that all patients 60 years of age and older be interviewed regarding falls with or without injury in the previous 12 months, changes in gait and/or balance, and fear of falling. The doctor should ask the patient 3 key questions:
- During the last year, have you had a fall-related injury or a fall without injury?
- Do you feel unsteady when standing or walking?
- Are you afraid of falling?
A positive answer to any of these questions requires a fall risk assessment, which is performed using the Self-Assessment of Falls Risk Questionnaire and the Morse Fall Risk Scale for Hospitalized Patients (Tables 5–7).
Table 5. Morse Fall Scale
| Categories | Answer options | Number of points |
| History of fall | No | 0 |
| Yes | 25 | |
| Comorbidities (≥1 diagnosis) | No | 0 |
| Yes | 15 | |
| Does the patient have a mobility aid? | Bed rest/nurse assistance | 0 |
| Crutches/stick/walker | 15 | |
| Clings when moving behind furniture | 30 | |
| Carrying out intravenous therapy (presence of an IV catheter) | No | 0 |
| Yes | 20 | |
| Walking function | Normal/bed rest/immobilized | 0 |
| Weak | 10 | |
| Violated | 20 | |
| The patient’s assessment of his own capabilities and limitations (mental/mental status) | Knows his limitations | 0 |
| Overestimates one's capabilities or forgets one's limitations | 15 | |
| Total: | 65 |
Note. The patient's answers are highlighted in color.
Table 6. Fall risk assessment
| Risk assessment | Points | Actions |
| No risk | 0 | Thorough basic medical care |
| Low level | 5–20 | |
| Average level | 25–45 | Implementation of standardized interventions to prevent falls |
| High level | ≥46 | Implementation of specific interventions aimed at preventing falls |
Note. The patient's answers are highlighted in color.
Table 7. Fall risk self-assessment scale
| Circle Yes or No for each statement. | ||
| Yes = 2 points | No = 0 points | I've been falling for the past year. |
| Yes = 2 points | No = 0 points | I use (or have been advised to use) a cane or walker to get around safely. |
| Yes = 1 point | No = 0 points | Sometimes I feel unsteady when walking. |
| Yes = 1 point | No = 0 points | I lean on furniture when moving around the house |
| Yes = 1 point | No = 0 points | I'm afraid of falling. |
| Yes = 1 point | No = 0 points | I need to use my hands to get up from a chair. |
| Yes = 1 point | No = 0 points | I have trouble getting up onto the curb. |
| Yes = 1 point | No = 0 points | I often have an urgent need to go to the toilet to urinate |
| Yes = 1 point | No = 0 points | My legs have lost feeling. |
| Yes = 1 point | No = 0 points | I take medications that make me dizzy or make me feel more tired than usual. |
| Total: 10 points 4 or more points – high risk of falls Less than 4 points – low risk of falls | ||
Note. The patient's answers are highlighted in color.
It is also necessary to evaluate risk factors for falls: decreased vision and hearing, urinary incontinence, cognitive impairment, depression, decreased mobility, polypharmacy, orthopedic problems, improperly selected canes and walkers, etc. Each of the identified risk factors and geriatric syndromes requires correction.
Older adults who have had a single fall are 2 to 3 times more likely to have repeated falls. Between 20 and 30% of falls result in injuries such as lacerations, fractures and brain injuries. About 90% of fractures in older people are associated with falls. And once a fracture occurs in an elderly person, it triggers a “cascade of fractures” or a “domino effect”: after the first fracture, the probability of a subsequent fracture increases by 3 times, after the second - by 5 times, and after the third - by 8 times. By 2050, the worldwide incidence of proximal femoral fractures is projected to increase by 310% in men and 240% in women. Osteoporotic fractures are associated with more days of hospitalization than other diseases such as breast cancer, myocardial infarction, diabetes mellitus, etc. The mortality rate is 20–24% during the first year after a hip fracture. At the same time, the number of fractures during therapy for senile osteoporosis increases with age and depends on the decrease in bone formation processes in old age [11].
Our patient, having suffered multiple fractures, experienced a reasonable fear of falling. At the same time, according to the geriatric examination, the risk of falls was high. As part of an integrated approach to the prevention and treatment of falls syndrome and osteoporosis, the patient herself and her relatives who care for and live with her in the apartment were trained in the principles of reducing the risk of falls: rules for arranging the apartment and everyday life, ensuring safety in the bathroom, equipping corridors with handrails and patient rooms, the presence of anti-slip mats, etc.
The past few years have seen significant advances in the diagnosis and treatment of osteoporosis, but despite this, the scale of the problem remains significant and catastrophic for patients, healthcare, and society. A wide selection of anti-osteoporotic drugs in elderly and senile people often does not provide significant results in the treatment of osteoporosis due to the fact that the principle of action of the vast majority of drugs is the suppression of osteoclast-mediated bone resorption. In the described clinical example, the patient has a classic “cascade of fractures”: 7 fractures over 19 years. According to the latest consensus statement issued by the International Osteoporosis Foundation (IOF) [12], treatment failure is characterized by at least one of the following:
- During treatment, two or more low-energy fractures occurred; during treatment, in two consecutive measurements, a loss of BMD of 4% in the hip and 5% in the vertebrae was noted;
- There was no decrease in bone resorption markers of 25% or more for antiresorptive drugs or an increase in bone formation markers of more than 25% when anabolic therapy was used in combination with BMD loss.
The presence of 4 low-energy fractures during osteoporosis treatment in this patient indicates the ineffectiveness of drug therapy and dictates the need to change the class of anti-osteoporotic drug. In the present patient, given the low levels of bone formation markers, bone anabolic therapy with teriparatide is the treatment of choice.
Teriparatide is a recombinant human parathyroid hormone (PTH 1–34) administered daily subcutaneously at a dose of 20 mcg/day using a prefilled pen. Periodic use of parathyroid hormone leads to an increase in the number and activity of osteoblasts, which leads to an increase in bone mass and improvement in the skeletal architecture of both trabecular and cortical bone tissue [13, 14]. The membranes of the “dormant” osteoblasts and stromal cells of the bone marrow lining the bone surface express receptors for parathyroid hormone on their surface, and an intermittent increase in it in the blood stimulates these cells through modulation of the levels of cAMP and cAMP-dependent protein kinase A. The PTH receptor is also activated by protein kinase-C. calcium regulatory pathway that stimulates the proliferation of mesenchymal cells into osteoblasts [14]. The exact signaling pathway responsible for the anabolic effect of parathyroid hormone is unknown, but different pathways may determine its subsequent anabolic and catabolic effects.
Inhibition of the Wnt-β-catenin pathway antagonist, sclerostin, is one explanation for the anabolic effects of teriparatide; Stimulation of the regulatory pathways MAPK (mitogen-activated protenkinase), phospholipase A and D also contributes to the anabolic effects of teriparatide, thus influencing the differentiation, proliferation and activity of osteoblasts, stimulating the differentiation and activation of resting bone lining cells, increasing the life expectancy of osteoblasts and osteocytes by inhibition of their apoptosis [15]. The anabolic effect of teriparatide is expressed in an increase in bone mineral density by 9.7% in the vertebrae and 2.8% in the femoral neck after 18 months of therapy, an increase primarily in bone formation markers, a reduction in the risk of vertebral fractures by 65%, and the appearance of new severe or multiple vertebral fractures by 84–94% and non-vertebral fractures – by 53% [16].
In this patient, daily self-injections of teriparatide were not particularly difficult for her and her relatives, which may be explained by the convenient form of teriparatide release. Adherence to treatment was high. Already after 7 months of treatment, a positive effect on BMD and the risk of fractures, pronounced clinical improvements in the form of increased physical activity, a decrease in the severity of pain, without any adverse effects, were noted. Laboratory and instrumental studies showed activation of bone metabolism and an increase in bone mineral density. No new fractures were observed.
FORSTEO
Pharmacodynamics
| Mechanism of action |
Teriparatide is a recombinant human parathyroid hormone produced using a strain of Escherichia coli (using DNA recombination technology).
Endogenous parathyroid hormone (PTH), which is a sequence of 84 amino acid residues, is the main regulator of calcium and phosphorus metabolism in the bones and kidneys. Teriparatide (recombinant human PTH (1-34)) is an active fragment of endogenous human PTH. The physiological effect of PTH is to stimulate bone formation through a direct effect on osteoblasts. PTH indirectly increases intestinal absorption and tubular reabsorption of calcium, as well as renal excretion of phosphate. Pharmacodynamic properties The biological effect of PTH is due to binding to specific PTH receptors on the surface of cells. Teriparatide binds to the same receptors and has the same effects on bones and kidneys as PTH.
Single daily administration of teriparatide stimulates the formation of new bone tissue on the trabecular and cortical (periosteal and/or endosteal) surfaces of bones with preferential stimulation of osteoblast activity relative to osteoclast activity. This is confirmed by an increase in the levels of markers of bone tissue formation in the blood serum: bone-specific alkaline phosphatase and carboxy-terminal propeptide of type I procollagen (PICP). The increase in the content of bone tissue formation markers is accompanied by a secondary increase in the level of bone resorption markers in urine: N-telopeptide (NTX) and deoxypyridinoline (DPD), which reflects the physiological interaction of the processes of bone tissue formation and resorption in skeletal remodeling. 2 hours after administration of teriparatide, a short-term increase in serum calcium concentration is observed, which reaches maximum values after 4-6 hours and returns to baseline values within 16-24 hours. In addition, transient phosphaturia and a slight short-term decrease in serum phosphorus levels may occur.
Clinical effectiveness
Postmenopausal osteoporosis
The main clinical trial of teriparatide included 1637 patients with postmenopausal osteoporosis, with a mean age of 69.5 years.
At the start of the study, 90% of patients had suffered 1 or more vertebral fractures and the mean vertebral bone mineral density (BMD) was equivalent to a T-score of -2.6. All patients took 1000 mg of calcium daily and. at least 400 IU vitamin D.
Results of teriparatide therapy for up to 24 months (mean duration of therapy was 19 months) indicate a statistically significant reduction in the incidence of fractures. The incidence of new vertebral fractures (>1 fracture, as measured by radiography at the beginning and end of the study) in the teriparatide group and in the placebo group was 5.0% and 14.3%, respectively (p < 0.001 compared with the placebo group, a relative decrease risk - 65%).
The incidence of multiple vertebral fractures (>2 fractures, as determined by radiography at the beginning and end of the study) in the teriparatide group and in the placebo group was 1.1% and 4.9%, respectively (p < 0.001 compared with the placebo group, relative risk reduction - 77%).
The incidence of nonvertebral low-energy fractures (minimal trauma fractures) in the teriparatide group and placebo group was 2.6% and 5.5%, respectively (p < 0.025 compared with placebo group, relative risk reduction 53%).
The incidence of major nonvertebral low-energy fractures (femur, radius, humerus, ribs, pelvis) in the teriparatide group and placebo group was 1.5% and 3.9%, respectively (p < 0.025 compared with the placebo group, decreased relative risk - 62%).
After 19 months of treatment (median duration of therapy), there was an increase in BMD at the lumbar spine and proximal femur compared to placebo by 9% and 4%, respectively (p < 0.001). Post-therapy follow-up: After completion of teriparatide therapy, 1262 women with postmenopausal osteoporosis from the main study were included in a follow-up study. The primary objective of the study was to collect data on the safety of teriparatide. During this observation period, other osteoporosis therapy was permitted and additional evaluation of vertebral fractures was performed. At an average of 18 months after discontinuation of teriparatide therapy, the number of patients with at least one new vertebral fracture in the teriparatide-experienced group was 41% lower than in the placebo group (p=0.004).
| In an open-label study, 503 patients with postmenopausal severe osteoporosis and fragility fractures (minimal trauma fractures) within the previous three years (83% had previously received treatment for osteoporosis) received teriparatide for 24 months. After 24 months, BMD at the lumbar spine, proximal femur, and femoral neck increased from baseline by an average of 10.5%, 2.6%, and 3.9%, respectively. From 18 to 24 months, BMD at the lumbar spine, proximal femur, and femoral neck increased by 1.4%, 1.2%, and 1.6%, respectively. Osteoporosis in men |
In a clinical study of men with osteoporosis due to hypogonadism (defined by low morning free testosterone or elevated follicle-stimulating hormone or luteinizing hormone concentrations) or
| 437 patients with idiopathic osteoporosis took part, with an average age of 58.7 years. At the start of the study, the BMD of the vertebrae and femoral neck according to the T-criterion ranged from -2.2 to -2.1, respectively. At the start of the study, 35% of patients had a history of vertebral fractures, and 59% of patients had fractures of other locations. All patients took 1000 mg calcium and at least 400 IU vitamin D daily. Significant increases in lumbar spine bone mineral density were noted after 3 months. After 12 months of therapy, BMD at the lumbar spine and proximal femur increased by 5% and 1%, respectively, compared with placebo. |
Osteoporosis with long-term therapy
| glucocorticosteroids The effectiveness of teriparatide in osteoporosis caused by long-term treatment with glucocorticosteroids was proven in an 18-month randomized, double-blind clinical trial with an active comparator (alendronate 10 mg/day; 428 patients, mean age 57 years). At the start of the study, 28% of patients had 1 or more vertebral fractures. All patients took 1000 mg of calcium and 800 IU of vitamin D daily. The study included 277 postmenopausal women, 67 premenopausal women and 83 men. After 18 months of therapy, BMD of the lumbar spine increased by 7.2% (by 3.4% in the alendronate group, p < 0.001), BMD of the proximal femur increased by 3.6% (by 2.2% in the alendronate group, p<0.01), femoral neck BMD increased by 3.7% (by 2.1% in the alendronate group, p<0.05). |
In patients taking teriparatide,
| study period from 18 months to 24 months of therapy, BMD of the lumbar spine, proximal femur, and femoral neck increased by an additional 1.7%, 0.9%, and 0.4%, respectively. In the teriparatide group, after 36 months of therapy, new vertebral fractures were detected in 1.7% of patients (7.7% in the alendronate group, p = 0.01), new non-vertebral fractures were detected in 7.5% of patients (7.0% in the alendronate group, p =0.84). In premenopausal women after 18 months of therapy, the increase in BMD was significantly higher in the teriparatide group compared with alendronate: lumbar spine BMD increased by 4.2% (-1.9% in the alendronate group, p < 0.001), proximal BMD femur increased by 3.8% (0.9% in the alendronate group, p = 0.005). |
Mineralization processes occur without signs of toxic effects on bone tissue cells, and bone tissue formed under the influence of teriparatide has a normal structure (without the formation of reticulofibrous bone tissue and bone marrow fibrosis). Teriparatide reduces the risk of fractures regardless of age, baseline bone turnover, or BMD (relative risk reduction for new fractures is 65%).
ADDITIONAL INFORMATION
Patient consent. The patient voluntarily signed informed consent for the publication of personal medical information in anonymized form in the journal Obesity and Metabolism.
Source of financing. The preparation and publication of the manuscript was carried out at the personal expense of the team of authors.
Conflict of interest. The authors declare that there are no obvious or potential conflicts of interest related to the publication of this article.
Authors' participation. All authors made significant contributions to the research and preparation of the article, and read and approved the final version of the article before publication.