Roflumilast (Roflumilastum)
Roflumilast is a non-steroidal anti-inflammatory drug intended for the maintenance treatment of patients with severe chronic obstructive pulmonary disease with frequent exacerbations. Due to the fact that in the general population of this disease there is a significant predominance of patients over the age of 40 years, when prescribing the drug to patients under 40 years of age, spirometric confirmation of the diagnosis of chronic obstructive pulmonary disease is required.
According to the indications for use of the drug, it is necessary that the value of the post-bronchodilator forced expiratory volume in the first second be less than 50% of the calculated proper value.
Roflumilast is not intended for the treatment of acute attacks of shortness of breath (acute bronchospasm). The patient should be warned that to relieve an acute attack, it is important to always have the drug prescribed by the doctor to stop the attack. Roflumilast is not effective in this case.
In studies conducted over a one-year period, weight loss was more common in patients receiving roflumilast compared to patients receiving placebo. After stopping the drug, most patients regained their body weight within 3 months.
In patients with low body weight, it should be monitored at every visit to the doctor. Patients should be advised to regularly monitor their body weight. In case of unexplained or clinically significant decrease in body weight, it is necessary to stop taking roflumilast and monitor the dynamics.
Due to the lack of sufficient experience, treatment with roflumilast should not be initiated in patients receiving continuous maintenance therapy with oral glucocorticosteroids, with the exception of short-term courses of systemic glucocorticosteroids.
Experience with the use of roflumilast in patients with latent infections such as tuberculosis, viral hepatitis, viral herpes and herpes zoster is limited.
The use of roflumilast is associated with an increased risk of mental disorders such as insomnia, anxiety, nervousness and depression. Clinical studies have identified rare cases of suicidal thinking and behavior. Therefore, if patients report previous or current psychiatric symptoms, or if concomitant therapy with other drugs associated with the potential for psychiatric disorders is planned, a careful assessment of the risks and benefits associated with initiation or continuation of treatment with roflumilast. Patients should be instructed to notify the prescriber of any changes in behavior, mood, or suicidal ideation of any nature.
Although adverse reactions such as diarrhea, nausea, abdominal pain and headache occur mainly in the first weeks of treatment and in most cases resolve with continued treatment, treatment with roflumilast should be reconsidered if these symptoms persist.
Intolerance may occur in special patient populations, particularly black non-smoking women or patients treated with the CYP1A2 inhibitor fluvoxamine or the two CYP3A4/1A2 inhibitors enoxacin and cimetidine.
There are no clinical data regarding concomitant treatment with theophylline as maintenance therapy. Therefore, concomitant treatment with theophylline is not recommended.
Roflumilast: new possibilities for pharmacotherapy of COPD
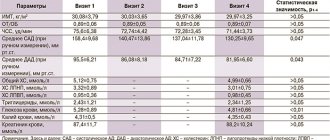
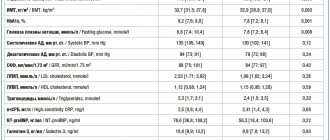
Traditionally, the disease treatment program uses bronchodilators (m-anticholinergics, β2-agonists) and glucocorticosteroids (GCS), which have universal anti-inflammatory activity. New pharmacotherapeutic opportunities are due to the appearance on the pharmaceutical market of drugs that can suppress specific inflammation in COPD. In 2010, a representative of a new class of drugs, roflumilast (Daxas®), was registered in the European Union and Canada. In March 2011, its use for the treatment of patients with COPD was approved by the US Food and Drug Administration (FDA), and in September of the same year, roflumilast was registered in the Russian Federation. Mechanism of action According to modern concepts, a key role in the pathogenesis of COPD is played by the inflammatory process, in the implementation of which phosphodiesterase type 4 (PDE4) is also involved, an enzyme that regulates the metabolism of cyclic adenosine monophosphate (cAMP). A cyclic nucleotide is a secondary intracellular messenger in the effects of hormones and biologically active compounds that do not penetrate into the cell. Under the influence of the latter, membrane adenylate cyclases (ACs) are activated in cells, catalyzing the formation of cAMP from adenosine triphosphate (ATP), resulting in the accumulation of cyclic nucleotide. Its concentration is many times higher than the concentration of the biologically active substance acting on the cell. The action of cAMP is based on the ability to interact with cellular protein kinase A (PK A). The binding of a cyclic nucleotide to the regulatory subunit of the enzyme leads to its dissociation and activation of the catalytic subunit, which, freed from the regulatory part, carries out phosphorylation of effector proteins [4]. The result of modification of protein molecules is, among other things, a decrease in the production of pro-inflammatory mediators, a slowdown in cell proliferation and apoptosis and, as a consequence, a decrease in the severity of inflammation (Fig. 1). The action of the cyclic nucleotide is limited by the activity of phosphodiesterase (PDE). Currently, 11 isoforms of this enzyme are known, catalyzing the cleavage of cAMP and another cyclic nucleotide, guanine monophosphate (cGMP), the effects of which are often opposite to those of cAMP [6]. PDE types 4, 7 and 8 are tropic to cAMP, types 5, 6 and 9 are tropic to cGMP. Enzymes of types 1–3 and 10–11 act on both cyclic nucleotides. The distribution of individual types of PDE in the cells of various organs and tissues differs significantly. It should be noted that the predominant isoform of the enzyme expressed by pro-inflammatory and immune cells responsible for the development of chronic inflammation in COPD is PDE4. This type of enzyme, in turn, has several subtypes. The action of all enzyme subtypes is aimed at activating the hydrolysis of cAMP and the formation of its inactive form - adenosine monophosphate (AMP). A decrease in the concentration of cyclic nucleotide is accompanied by an increase in the pro-inflammatory potential of cells, including neutrophils, T-lymphocytes (CD8+) and macrophages. By releasing various mediators, these cells trigger a cascade of inflammatory reactions, leading to limitation of bronchial patency and the development of systemic inflammation [7]. Suppression of PDE4 activity, on the contrary, leads to the accumulation of cAMP in cells and the implementation of the anti-inflammatory effects of hormones and mediators, the mediator of which is the cyclic nucleotide (Table 1). The decrease in pro-inflammatory cell activity observed when PDE4 is suppressed has led to particular interest in the possibilities of pharmacological inhibition of the enzyme as a way to influence the severity of chronic inflammation in COPD. Currently, a number of drugs are known that can block the action of PDE. Some, being non-selective, interact with different types of enzyme (theophylline), others, having high selectivity, suppress the activity of one isoform of the enzyme (PDE3 inhibitor - milrinone, PDE5 - ildenafil). The action of theophylline, which is a non-selective inhibitor of almost all types of PDE and, in addition, an antagonist of adenosine receptors, is associated with the development of a large number of diverse effects, among which mention should be made of the effect on the contractile activity of smooth muscles, mucociliary clearance, blood vessel tone, frequency and strength of heart contractions , acidity of gastric contents, etc. At the same time, the activity of theophylline against PDE4, and hence its anti-inflammatory effect, is minimally expressed. The use of the drug is associated with a high risk of adverse reactions and clinically significant drug interactions. An important circumstance limiting the therapeutic potential of theophylline in COPD is the decrease in its effectiveness in smokers. The first selective PDE4 inhibitor was cilomilast, a significant disadvantage of which is its predominant activity against the D subtype of the enzyme. The effect of cilomilast on PDE4D, present in the parietal cells of the gastric mucosa and cells of the vomiting centers, has led to the frequent occurrence of nausea and vomiting associated with the drug, which has served as a reason to limit its use. A new representative of selective PDE4 inhibitors, roflumilast, is superior to its predecessor in terms of its effect on the enzyme and, unlike it, has the same activity against all subtypes of the enzyme. The effect of roflumilast is to reduce the activity of cells involved in the development of inflammation in COPD. Suppression of PDE4 activity of bronchial smooth muscle cells, as shown by the results of studies, is not accompanied by pronounced bronchodilation, and therefore the drug cannot be used to relieve bronchospasm. Pharmacokinetics The effectiveness and safety of drugs is largely determined by their pharmacokinetic profile. The favorable pharmacokinetic characteristics of roflumilast make it attractive for practical use. The drug is quickly and fairly completely (bioavailability is 80%) absorbed in the gastrointestinal tract. Maximum serum concentrations are achieved 0.5–2 hours after administration of roflumilast. Being metabolized by enzymes of the cytochrome P450 system (CYP 3A4 and 1A2), the PDE4 inhibitor forms an active metabolite - roflumilast N-oxide, which is superior in pharmacokinetic parameters to the original molecule (Table 2). The formation of inactive metabolites of roflumilast N-oxide is carried out using isoenzymes CYP3A4 and 2C19. The use of roflumilast in a therapeutic dose, as evidenced by the results of studies, is not accompanied by significant inhibition of the enzymatic system. The long half-life of the PDE4 inhibitor and its active metabolite allows the drug to be administered once a day. Elimination of the drug is carried out mainly by the kidneys (70%) in the form of inactive metabolites [9]. It should be noted that the participation of enzymes of the cytochrome P450 system in the metabolism of roflumilast determines the likelihood of clinically significant drug interactions with such pronounced inducers of liver enzymes as rifampicin, phenobarbital and carbamazepine, as well as CYP 3A4 and 1A2 inhibitors enoxacin and cimetidine. At the same time, no data have been obtained on the interaction of the drug with warfarin, digoxin, theophylline, midazolam, or antacids. The presence of severe liver failure (Child-Pugh classes B and C) is accompanied by a significant increase in Cmax and AUC0–∞ of the PDE4 inhibitor and serves as a contraindication for its use. Simultaneous food intake, while reducing the maximum serum concentration of roflumilast, nevertheless does not affect the pharmacokinetic characteristics of its active metabolite. Smoking also does not affect the pharmacokinetic profile of the PDE4 inhibitor and does not reduce its effectiveness [11]. Clinical efficacy Evidence of the effectiveness of roflumilast in the treatment of patients with COPD was obtained from numerous placebo-controlled clinical studies. The results of the most significant studies are presented in Table 3. Analysis of the data presented indicates that the use of the drug is accompanied by a significant increase in forced expiratory volume in 1 s (FEV1) compared to placebo. It should be noted that patients taking a PDE4 inhibitor as part of the studies had severe bronchial obstruction (FEV1<60% of the expected values). A significant improvement in the ventilation function of the lungs was noted after 4 weeks. use of roflumilast and persisted throughout the entire treatment period. According to available data, the degree of bronchial obstruction correlates with the severity of inflammation in the airways, which helps explain the increase in FEV1 when taking a drug that is not a bronchodilator. The effect of a PDE4 inhibitor on the incidence of exacerbations of the disease deserves special attention. As recent studies have shown, it is the frequency of exacerbations that is one of the most important factors determining the quality of life of patients with COPD, the rate of disease progression and economic losses [18,19]. According to the opinion of international experts, reflected on the pages of the Global Strategy for the Diagnosis, Treatment and Prevention of COPD (Global Initiative for Chronic Obstructive Lung Disease (GOLD)), reducing the frequency and severity of exacerbations is one of the main goals of treating the disease [20]. In a pooled analysis of data from the RATIO and OPUS studies, roflumilast was shown to significantly reduce the incidence of severe and moderate exacerbations of COPD compared with placebo. This effect of the drug was most pronounced in patients whose clinical picture of the disease was characterized by the presence of symptoms of chronic bronchitis. The use of a PDE4 inhibitor in this category of patients reduced the frequency of exacerbations of the disease by 26.2%, while in patients with emphysema and without chronic bronchitis - by only 1.1% [15]. The use of roflumilast was also more effective in patients taking inhaled corticosteroids (ICS). The reduction in the frequency of exacerbations among patients taking ICS (at a daily dose equivalent to ≤ 2000 mcg of beclomethasone) and patients not taking them was 18.8 and 7.7%, respectively [15]. In addition, a retrospective analysis of data obtained during 52-week studies of the drug revealed a correlation between the reduction in the frequency of exacerbations while taking roflumilast and the number of exacerbations in the patients' history. It has been shown that the presence of frequent exacerbations of COPD (2 or more in the previous 12 months) is associated with greater effectiveness of the drug (Fig. 2). The use of a PDE4 inhibitor in combination with bronchodilators, as evidenced by the results of studies, increases the effectiveness of disease therapy. Thus, the addition of roflumilast (500 mcg 1 time/day) to tiotropium significantly increased prebronchodilator FEV1 compared with placebo [17]. The use of the drug in patients taking long-acting β2-agonists was also accompanied by a significant improvement in bronchial obstruction and a decrease in the frequency of severe and moderate exacerbations of COPD (Fig. 3). Safety profile In 2011, data on the tolerability of roflumilast were published from an analysis of 14 placebo-controlled studies (Table 4). According to the data obtained, taking a PDE4 inhibitor is most often associated with diarrhea and nausea (10.1 and 5.2%, respectively). In addition, the use of roflumilast may be associated with the development of adverse reactions such as dizziness, headache, insomnia, and an increased risk of mental disorders. No data have been obtained on the effect of the drug on the incidence of respiratory tract infections. It should be noted that adverse events (AEs) associated with the use of roflumilast usually occur in the first weeks of treatment and subsequently resolve without requiring discontinuation of the drug [11]. During clinical studies, a rather unexpected effect of the PDE4 inhibitor was revealed - a decrease in the body weight of patients, observed, as a rule, during the first 6 months. treatment. Thus, according to data obtained from the AURA and HERMES studies, in the group of patients receiving roflumilast, this indicator decreased by an average of 2.1 kg [16]. The greatest loss of body weight was observed among patients who were obese (body mass index >30 kg/m2) (Fig. 4). This effect is mainly due to the direct lipolytic effect of the drug. Discontinuation of roflumilast is reported to be associated with restoration of baseline body weight. Dosage and use Roflumilast is prescribed for adults orally at 500 mcg 1 time / day, regardless of meals. In elderly patients, as well as in the presence of renal failure, no dose adjustment is required. Conclusion The appearance of roflumilast in the arsenal of drugs used to treat COPD expands the possibilities of pharmacotherapy of the disease, making it possible to influence its pathogenetic mechanisms. According to research results, the use of a PDE4 inhibitor is most justified in patients with symptoms of chronic bronchitis, severe bronchial obstruction (FEV1<50%) and frequent exacerbations of the disease (≥2/12 months). According to existing recommendations for the treatment of COPD, the drug can be used as an additional therapy in the most severe category of patients (group D) [20].
References 1. Atsou K., Chouaid C., Hejblum G. Variability of the chronic obstructive pulmonary disease key epidemiological data in Europe: systematic review // BMC Medicine. 2011. Vol. 9. R. 7. 2. Menezes AM, Perez–Padilla R., Jardim JR, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): A prevalence study // Lancet. 2005. Vol. 366. R. 1875–1881. 3. World Health Organization Website. Chronic Obstructive Pulmonary Disease https://www.who.int./respiratory/copd. 4. Houslay MD: Underpinning compartmentalised cAMP signaling through targeted cAMP breakdown // Trends Biochem Sci. 2010. Vol. 35. R. 91–100. 5. Rabe KF. Roflumilast for the treatment of chronic obstructive pulmonary disease // Expert Rev Respir Med. 2010. Vol. 4 (5). R. 543–555. 6. Jeon Y., Heo Y., Kim C. et al. Phosphodiesterase: overview of protein structures, potential therapeutic applications and recent progress in drug development // Cell. Mol. Life Sci. 2005. Vol. 62 (11). R. 1198–1220. 7. Barnes PJ, Hansel TT Prospects for new drugs for chronic obstructive pulmonary disease // Lancet. 2004. Vol. 364. R. 985–996. 8. Page CP, Spina D. Selective PDE inhibitors as novel treatments for respiratory diseases // Curr Opin Pharmacol. 2012. Vol. 12. R. 275–286. 9. Tenor HHA, Beume R., Lahu G., Zech K., Bethke T. Pharmacology, clinical efficacy and tolerability of phosphodiesterase–4 inhibitors: impact of human pharmacokinetics. In: Francis SH et al. (eds). In “Phosphodiesterases as drug targets, handbook of experimental pharmacology 204”. Berlin Heidelberg: Springer–Verlag, 2011. 10. Taegtmeyera A.V., Leuppib JD, Kullak–Ublicka GA Roflumilast – a phosphodiesterase-4 inhibitor licensed for add-on therapy in severe COPD // Swiss Med Wkly. 2012. Vol. 142:w13628. 11. Rabe KF Update on roflumilast, a phosphodiesterase 4 inhibitor for the treatment of chronic obstructive pulmonary disease // Br J Pharmacol. 2011. Vol. 163(1). R. 53–67. 12. Rabe KF, Bateman ED, O'Donnell D. et al. Roflumilast – an oral antiinflammatory treatment for chronic obstructive pulmonary disease: a randomized controlled trial // Lancet. 2005. Vol. 366. R. 563–571. 13. Calverley PM, Sanchez–Toril F., McIvor A. et al. Effect of 1–year treatment with roflumilast in severe chronic obstructive pulmonary disease // Am J Respir Crit Care Med. 2007. Vol. 176(2). R. 154–161. 14. FDA. Center for Drug Evaluation and Research. Application number 022522Orig1s000. Medical Review(s). Available at https://wwwaccessdatafdagov/drugsatfda_docs/nda/2011/022522Orig1s000MedRpdf. 15. Rennard SI, Calverley PM, Goehring UM, et al. Reduction of exacerbations by the PDE4 inhibitor roflumilast – the importance of defining different subsets of patients with COPD // Respir Res. 2011. Vol. 12. R. 18. 16. Calverley PM, Rabe KF, Goehring UM et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomized clinical trials // Lancet. 2009. Vol. 374. R. 685–694. 17. Fabbri LM, Calverley PM, Izquierdo–Alonso JL et al. Roflumilast in moderate–to–severe chronic obstructive pulmonary disease treated with longacting bronchodilators: two randomized clinical trials // Lancet. 2009. Vol. 374. R. 695–703. 18. Hurst JR, Vestbo J, Anzueto A et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease // N Engl J Med. 2010. Vol. 363. R. 1128–1138. 19. Soler–Cataluna JJ Martinez–Garcia MA, Serra PC Frequent exacerbations contribute to the mortality of COPD // Thorax. 2005. Vol. 64. R. 925–931. 20. Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2011. Available from: https://www.goldcopd.org/. 21. Bateman E, Calverley PM, Fabbri LM et al. Efficacy of roflumilast in patients with a history of frequent exacerbations: Pooled data from pivotal 12'mont studies. European Respiratory Society Annual Congress 2010. Barcelona, 2010. P. 4003.
Roflumilast: truth is born in dispute
In 2010, the first oral phosphodiesterase type 4 inhibitor, roflumilast, was registered in the European Union and Canada. In March 2011, the US Food and Drug Administration approved its use for the treatment of patients with chronic obstructive pulmonary disease (COPD). In August of the same year, roflumilast was registered in Russia. During this time, new data have emerged on the effectiveness and safety of the drug, its ability to reduce the frequency of exacerbations of COPD, and adverse events that occur during its use. This article analyzes recent publications on the results of experimental and clinical studies of the mechanism of action of roflumilast, discussing data on its effectiveness and safety profile.
Approaches to the treatment of chronic obstructive pulmonary disease (COPD) are constantly being improved. However, achievements in this area are quite modest, since no real ways to modify the course of the disease have yet been found [1].
Over the past 30 years, prospects for the development of COPD therapy have been associated primarily with bronchodilators and inhaled steroids. The refusal to register the first phosphodiesterase type 4 (PDE-4) inhibitors, in particular cilomilast [2, 3], reduced the interest of a number of pharmaceutical companies in them. Today the situation is different: the first clinically significant PDE-4 inhibitor, roflumilast, has been approved in 61 countries around the world. The renewed interest in PDE-4 inhibitors led not only to the appearance of roflumilast on the medical market, but also to the development of new molecules and delivery methods, various combinations with PDE-4 inhibitors [4].
Some experts call roflumilast a selective theophylline. Meanwhile, theophylline was introduced into practice as a bronchodilator, a weak and non-selective inhibitor of PDE isoenzymes of groups 1–11, the leading mechanism of which was antagonism with adenosine [5, 6]. Theophylline has a low therapeutic index and is inferior in effectiveness to long-acting inhaled bronchodilators [6].
Roflumilast was initially considered not as a bronchodilator, but as an anti-inflammatory drug of a fundamentally new class, selectively affecting PDE-4.
PDEs are a large group of enzymes that catalyze the breakdown of cyclic adenosine monophosphate (cAMP) and/or cyclic guanosine monophosphate (cGMP) to an inactive form. PDE-4 is highly expressed in leukocytes and other inflammatory cells involved in the pathogenesis of inflammatory lung diseases such as asthma and COPD. This determined the prognosis for the practical use of PDE-4 inhibitors as anti-inflammatory drugs with a significant therapeutic effect.
Roflumilast was the only PDE4 inhibitor that managed to reach the pharmaceutical market due to its good efficacy/tolerability ratio. The drug was recommended for the treatment of patients with COPD with severe obstruction, symptoms of chronic bronchitis and a history of exacerbations, that is, for those patients whose disease is not adequately controlled by therapy with long-acting bronchodilators.
The results of clinical studies of roflumilast create the prerequisites for expanding the indications for its use in COPD and other respiratory (for example, bronchial asthma) and non-respiratory inflammatory and metabolic diseases (in particular, diabetes) [7].
The mechanism of action of roflumilast remains the subject of careful study. It was shown that the drug increased the release of vascular endothelial growth factor (VEGF) both when interacting with E-prostanoid 2 receptors and their agonists, increased the level of prostaglandin E2-induced cAMP in the cytoplasm and the release of VEGF under the influence of other agents , which use a signaling pathway involving cAMP. The stimulating effect of roflumilast on the release of VEGF was reproduced in fibroblasts from both healthy people and patients with COPD [8].
The introduction of roflumilast into the complex therapy of COPD is aimed at solving the problem associated with disease progression. It is exacerbations of COPD that are accompanied by an increase in the severity of the disease and mortality and can accelerate the progression of the disease. The best predictor of subsequent exacerbations is a history of exacerbations. This allows us to determine the phenotype of a patient with frequent exacerbations.
A group of English scientists conducted a retrospective analysis of the effectiveness of roflumilast, a drug that can reduce the frequency of exacerbations of COPD, at a dose of 500 mcg once a day in patients with symptomatic COPD and severe airway obstruction. This study used the results of two one-year placebo-controlled randomized clinical trials (RCTs) (M2-124 and M2-125, ClinicalTrials.gov identifiers NCT00297102 and NCT00297115) with a follow-up period of 1 year. Among the 3091 patients included in the analysis, 62.5% were diagnosed with stage III COPD and 29.2% were diagnosed with stage IV according to the GOLD (Global initiative for chronic obstructive lung disease) classification. Based on data on the frequency of exacerbations in the anamnesis, patients were distributed according to the phenotype of the disease: frequent (≥ 2 per year) and rare (
After the main clinical trials were completed and roflumilast began to be used in everyday practice for the treatment of COPD, several publications appeared on adverse events associated with the drug [10, 11, 12] and initiated a lively debate [13].
One of the studies [10] reported that the Spanish pharmacosafety system received several reports of the development of adverse events from the gastrointestinal tract (GIT) and mental disorders while taking roflumilast. In this regard, it was noted that patients receiving this drug should be closely monitored. The authors of the publication described a single case of the development of severe diarrhea and severe weight loss shortly after starting the use of roflumilast. Possible reactions from the gastrointestinal tract at the beginning of therapy are also noted in the instructions for use of roflumilast. However, it should be recognized that to assess the effectiveness and safety of the drug, experts from the United States Food and Drug Administration (FDA) were presented not only with individual publications, but also with samples of more than 12,000 patients with analysis the potential significance of rare but significant events that are difficult to analyze in individual studies. Based on these data, regulatory agencies in 61 countries, including the United States and the European Union, concluded that roflumilast has a favorable risk/benefit ratio for its intended use [14]. The FDA expert report stated that about 90% of gastrointestinal adverse events in clinical studies were mild to moderate and self-limiting.
Another critical article was presented by employees of the University of Missouri (USA) [11]. Based on the results of eight RCTs selected according to the relevant inclusion criteria, the authors noted that roflumilast significantly reduced the incidence of moderate exacerbations (RR 0.85; 95% CI (confidence interval) 0.80–0.91) compared with placebo, but not had an effect on severe exacerbations (RR 0.83; 95% CI 0.68–1.01). However, this does not contradict the conclusions of the publication of experts in the field of COPD, who, based on the results of two RCTs that included patients with severe COPD, concluded that roflumilast demonstrated effectiveness in reducing the risk of exacerbations in patients with severe COPD, symptoms of bronchitis and exacerbations in medical history [15].
In contrast to the conclusions about the risks associated with the administration of roflumilast, the article by S. Siddiqui [13] noted that the meta-analysis by Y. Oba, NA Lone (2013) is not entirely objective, since comparisons and generalizations on roflumilast were made outside the target patient population, which the drug was indicated, that is, the populations were not focused on identifying adverse reactions. At the same time, scientists from Missouri confirmed that roflumilast significantly improved lung function compared to placebo.
Particular attention in the publications of opponents is paid to the safety of the use of roflumilast - disorders of the gastrointestinal tract, cardiovascular (CV) and central nervous system. It was noted that adverse events (RR 1.11; 95% CI 1.03–1.19) and treatment discontinuation due to adverse events (RR 1.63; 95% CI 1.45–1.84) were more frequent in roflumilast group than in the placebo group. However, in the COPD safety population (12,054 patients), there were generally no differences in the incidence of serious adverse events between groups [11].
Note that any strong drug is characterized by a number of established adverse effects. The most effective and necessary drugs have repeatedly become the subject of debate. As you know, diarrhea occurs while taking many antibiotics. Even in children with otitis media, diarrhea occurred in 17.5% of cases when using amoxicillin and in 8.2% when using azithromycin [16]. However, both drugs are considered the “gold standard” in the treatment of bacterial respiratory infections. Amoxicillin/clavulanate in 2008 became the leader in hepatotoxic reactions among penicillins (12.8–14% of cases) and the most common cause of hospitalizations associated with drug-induced liver damage [17]. But this did not affect the clinical significance of the drug. Its generics were created and more advanced forms of the brand appeared.
Epidemiological studies show that a significant proportion of deaths from COPD are associated with cardiovascular disorders [18]. Atrial fibrillation (0.4% vs 0.2%; p = 0.02) was more common in the roflumilast group than in the placebo group [11]. However, the opposite data on cardiovascular risk were obtained in 2013 by researchers from the United States and Switzerland: they conducted a meta-analysis of 14 placebo-controlled RCTs of 12 and 52 weeks duration to assess the risk of serious cardiovascular adverse events with roflumilast. Of 12,054 patients with moderate, severe and very severe COPD, 6563 received roflumilast, 5491 received placebo. All deaths and significant nonfatal cardiovascular events were assessed by an independent committee blinded to the nature of the therapy being administered. Among those receiving roflumilast, there were 52 patients with severe cardiovascular adverse events (14.3 per 1000 patient-years); among those receiving placebo, the number of such patients was 76 (22.3 per 1000 patient-years). That is, the overall incidence of severe cardiovascular adverse events was significantly lower in the roflumilast group compared to the placebo group (RR 0.65; 95% CI 0.45–0.93; p = 0.019). The possibility of a positive effect of roflumilast on CVS requires further evaluation in RCTs [19]. The positive effect of roflumilast on CVS may be associated with a decrease in vascular inflammation.
These conflicting data have also become the subject of discussion. Critics of roflumilast noted that the incidence of nonfatal stroke was the only component of severe cardiovascular events that had a significant trend. Thus, it is fair to say that roflumilast reduces the incidence of cerebrovascular events, but not cardiovascular events or mortality, since the incidence of the latter did not differ from the incidence in the placebo group. It has been suggested that the CV safety profile of roflumilast may change if subsequent studies include patients at high cardiac risk [12].
The response article [13] said the following. Although serious adverse events such as atrial fibrillation were more common in the roflumilast group than in the placebo group, a comprehensive population-based study of COPD patients to assess the safety of atrial fibrillation showed that all cases of fibrillation (placebo (n = 9) ; roflumilast (n = 24)) were assessed by the investigators as unlikely to be related or not related to the drug. Moreover, the results of 24-hour Holter ECG monitoring in 55 patients (RCT M2-124) showed no differences between groups in heart rate or the occurrence of arrhythmias [14]. The FDA concluded that roflumilast has an acceptable risk/benefit ratio for marketing authorization. The instructions for use of the drug contain all the necessary warnings [20]. The results of Holter monitoring confirm the opinion of some authors that episodes of atrial fibrillation while taking roflumilast were most likely a coincidence. All deaths and significant non-fatal cardiovascular events in the population to assess the safety of roflumilast in COPD were assessed by an independent expert committee blinded to the treatment [19]. This analysis showed that serious cardiovascular adverse events (death, non-fatal myocardial infarction and stroke) were significantly less common with roflumilast compared with placebo (RR 0.65; 95% CI 0.45–0.93; p = 0.019 ). This indicates not only the absence of danger from the use of roflumilast, but also the potential benefit of this treatment in relation to cardiovascular disease, which should be taken into account in future RCTs.
Research into the cardiotropic effect of PDE-4 inhibitors continues at the experimental level. PDE limits the positive inotropic effect of beta-adrenergic receptor stimulation by destroying cAMP. Therefore, PDE inhibitors increase sensitivity to catecholamines and can be used as positive inotropes. In this case, the positive inotropic effect is accompanied by an increase in energy consumption, the risk of cell death and arrhythmias.
For many years, PDE-3 was considered the main isoenzyme responsible for controlling the force of heart contraction and rhythm. However, recent studies in rodents have shown that PDE-4 is also involved in these processes. It is necessary to take into account that in cAMP mouse cardiomyocytes the hydrolytic activity of PDE-4 is about 30–50%, and in human cardiomyocytes it is no more than 10%, which is associated with the high activity of other PDEs (types 1, 2 and 3) [ 21].
A study in healthy volunteers showed that roflumilast (500 mcg orally) and salbutamol (200 mcg 3 times daily via metered-dose inhaler) for 7 days had no mutual effects on pharmacokinetics and were well tolerated. No increase in the incidence of serious adverse events was noted [22]. Experimental and clinical data support the good cardiovascular safety of PDE4 inhibitors.
Analysis of the frequency of hospitalizations allows us to judge changes in the costs of therapy for patients with COPD in the case of the use of roflumilast. In a budget impact model, an assessment of the impact of including roflumilast in COPD therapy showed a reduction in medical costs, which was largely due to a decrease in the number of hospitalizations [23]. A retrospective analysis of key RCTs (M2-124/125) demonstrated that roflumilast, compared with placebo, significantly reduced the incidence of severe exacerbations leading to hospitalization [24]. Additional analysis of real-world medical studies is currently underway to evaluate the effect of roflumilast on reducing hospitalization and readmission rates [13].
Publications from 2013 indicate the cost-effectiveness of the use of roflumilast in patients with severe and very severe COPD with a history of exacerbations. A cohort analysis conducted in Switzerland with Markov modeling showed that the inclusion of roflumilast in complex therapy reduces the costs of the healthcare system and is a cost-effective method of treating patients with COPD with frequent exacerbations [25]. In Germany, the cost-effectiveness of combining roflumilast with a LABA in the treatment of severe and very severe COPD was proven [26]. A similar cost-effectiveness analysis of the use of roflumilast as an adjunct to a LABA in the treatment of severe and very severe COPD with clinical signs of bronchitis and a history of frequent exacerbations was conducted in the UK. Based on the country’s economic attitudes, this combination was also considered profitable [25].
A retrospective analysis of two phase III RCTs showed that roflumilast reduced the frequency of exacerbations in patients with severe and very severe COPD who were simultaneously receiving ICS, while among those who did not receive ICS, this effect on the frequency of exacerbations was not detected [24]. In two other RCTs in patients with severe COPD, roflumilast reduced the incidence of exacerbations in patients not receiving ICS [23]. That is, the inhibition of PDE-4 was sufficient to achieve a therapeutic effect. Given that roflumilast is recommended as an adjunctive agent in the treatment of severe COPD, most such patients will need to receive a combination of LABA/ICS. Canadian researchers tested whether roflumilast is able to increase the effect of GCS through the induction of genes with anti-inflammatory activity. Using a GC response element (GRE) luciferase reporter transfected into human airway epithelial cells (bronchial epithelium + adenovirus 12-SV40 (BEAS-2B) hybrid culture and primary culture), it was shown that roflumilast enhanced the induced fluticasone propionate GRE-dependent transcription. Roflumilast also caused a leftward shift in the concentration-response curve, which was described as an increase in GRE-dependent gene transcription by the LABA formoterol. In BEAS-2B cells and primary epithelial culture, roflumilast, when interacting with formoterol, improved the expression of several GCS-inducible genes with anti-inflammatory potential. The authors concluded that the combination of roflumilast and formoterol is superior to ICS monotherapy, or PDE4 inhibitor alone, or ICS/LABA. Therefore, roflumilast may be particularly effective in patients with severe COPD [27]. A new class of bronchodilators with dual pharmacological action targeting beta-2 adrenergic receptors and PDE-4 have been developed and synthesized by combining the pharmacophores of salmeterol and roflumilast or phthalazinone. All components were characterized by high activity against beta-2 adrenergic receptors (pEC(50) = 8.47–9.20) compared with the reference substance salmeterol (pEC(50) = 8.3) and good inhibitory activity against PDE- 4B2 (IC(50) = 0.235–1.093 μM) [28].
Another mechanism for reducing the incidence of exacerbations of COPD when treated with roflumilast may be its effect on respiratory syncytial virus. Spanish researchers published the results of experimental work in which they showed that roflumilast N-oxide suppresses this virus in cultured bronchial epithelial cells and reduces the cytopathological changes associated with it [29].
Thus, based on the large number of studies conducted, it can be concluded that the first oral PDE-4 inhibitor, roflumilast, which recently appeared in clinical practice, has an encouraging efficacy and safety profile. Recent publications indicate both the positive effect of including roflumilast in combination therapy for COPD and the potential benefit of the drug in relation to CVS in patients with severe and very severe COPD with frequent exacerbations.
Daxas®
Daxas is a non-steroidal anti-inflammatory drug intended for the maintenance treatment of patients with severe COPD with frequent exacerbations. Due to the fact that in the general COPD population there is a significant predominance of patients over the age of 40 years, when prescribing the drug to patients under 40 years of age, spirometric confirmation of the diagnosis of COPD is required.
According to the indications for use of the drug, it is necessary that the post-bronchodilator FEV1 value be less than 50% of the calculated proper value.
Daxas is not intended for the treatment of an acute attack of shortness of breath (acute bronchospasm). The patient should be warned that to relieve an acute attack, it is important to always have the drug prescribed by the doctor to stop the attack. Daxas is not effective in this case.
In studies conducted over a one-year period, weight loss was more common in patients receiving Daxas compared to patients receiving placebo. After discontinuation of Daxas, most patients regained their body weight within 3 months.
In patients with low body weight, it should be monitored at every visit to the doctor. Patients should be advised to regularly monitor their body weight. In case of unexplained or clinically significant weight loss, you should stop taking Daxas and monitor the dynamics.
Due to the lack of sufficient experience, treatment with Daxas should not be started in patients receiving continuous maintenance therapy with oral corticosteroids, with the exception of short-term courses of systemic corticosteroids.
Experience with the use of Daxas in patients with latent infections such as tuberculosis, viral hepatitis, viral herpes and herpes zoster is limited.
The use of Daxas is associated with an increased risk of mental disorders such as insomnia, anxiety, nervousness and depression. Clinical studies have identified rare cases of suicidal thinking and behavior. Therefore, if patients report previous or current psychiatric symptoms, or if concomitant therapy with other drugs associated with the potential for psychiatric disorders is planned, a careful assessment of the risks and benefits associated with initiation or continuation of treatment with Daxas. Patients should be instructed to notify the prescriber of any changes in behavior, mood, or suicidal ideation of any nature.
Despite the fact that adverse reactions such as diarrhea, nausea, abdominal pain and headache occur mainly in the first weeks of treatment and in most cases resolve with continued treatment, if these symptoms persist, treatment with Daxas should be reconsidered.
Intolerance may occur in special patient populations, particularly black non-smoking women or patients treated with the CYP1A2 inhibitor fluvoxamine or the two CYP3A4/1A2 inhibitors enoxacin and cimetidine.
There are no clinical data regarding concomitant treatment with theophylline as maintenance therapy. Therefore, concomitant treatment with theophylline is not recommended.
Impact on the ability to drive vehicles and operate machinery
Due to the possibility of developing adverse reactions, patients should be careful when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.