Many patients, in search of drugs to normalize blood pressure, are faced with the problem of whether to choose Lozap or Losartan, since both drugs have a similar spectrum of action. To make the right choice, it is necessary to study the composition, indications and features of the effect of medications on the body.
To normalize blood pressure, you can use Lozap or Losartan.
Compound similarities
Both drugs are available in tablet form. The compositions of the medications are identical, because they contain the same active ingredient - losartan potassium. The auxiliary components are also the same: magnesium stearate, silicon dioxide, macrogol (a substance that provides a laxative effect), white dye, lactose monohydrate.
Considering the fact that the main component of both drugs is the same, their indications for use do not differ:
- arterial type hypertension;
- chronic heart failure;
- diabetic nephropathy;
- left ventricular hypertrophy;
- hyperkalemia (in this case, the drugs are prescribed as potent diuretics);
- as a prophylaxis to reduce the risk of diseases and pathologies of the heart muscle and vascular system in the presence of provoking factors.
The effects of Lozap and Losartan on the body are also the same - the main component helps thin the blood, thereby reducing the risk of blood clots. Losartan potassium reduces the concentration of the hormones aldosterone and norepinephrine, which, when excessively released into the blood, negatively affect the vessels, narrowing the lumen between them. The medications have a pronounced diuretic effect.
Medicines stabilize the concentration of urea, lower blood pressure, normalizing its levels and thereby reducing the load on the heart muscle and vascular system, which is one of the best preventions of heart and vascular diseases, including heart attack and stroke. The drugs have no effect on the central nervous system. The effect on the concentration of the hormonal substance norepinephrine, which narrows the lumen between the walls of blood vessels, is short-lived.
Lozap stabilizes the concentration of urea, lowers blood pressure, normalizing its levels and thereby reducing the load on the heart muscle.
Comparison of side effects of Losartan and Lozap
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Losartan has almost the same level of adverse events as Lozap. They both have few side effects. This implies that the frequency of their occurrence is low, that is, the indicator of how many cases of an undesirable effect of treatment are possible and registered is low. The undesirable effect on the body, the strength of influence and the toxic effect of Losartan are similar to Lozap: how quickly the body recovers after taking it and whether it recovers at all.
Differences between Lozap and Losartan
Despite the fact that both medicines contain the same active ingredient and an almost identical list of auxiliary components, there are some differences between them.
Losartan contains slightly more additional substances, so the likelihood of side symptoms and the range of contraindications will be slightly greater. Additional excipients of Lozap are:
- mannitol;
- cellulose;
- silica;
- talc.
We recommend reading: Comparison of Ketoprofen and Diclofenac
From Losartan:
- magnesium stearate;
- lactose monohydrate;
- calcium carbonate;
- starch.
The diuretic effect of Lozap is provided by the substance mannitol, and in the second drug - magnesium stearate. Due to the presence of mannitol in the medicine, Lozap is strictly forbidden to be taken simultaneously with medications that have a diuretic effect. In addition, throughout the entire therapeutic course it is necessary to regularly undergo laboratory tests to check calcium concentration and water-salt balance.
Medicines and manufacturers differ: Lozap is produced in the Czech Republic, Losartan - in Israel, but there is also a more budget option, which is produced in Belarus.
Losartan contains slightly more additional substances, so the likelihood of side symptoms and the range of contraindications will be slightly greater.
The period of onset of the therapeutic effect also differs between the agents. Lozap begins to act within 2-3 hours, the effect lasts for 1-1.5 days, Losartan - from 5 hours with the therapeutic effect remaining throughout the day. These figures are averaged, since the effectiveness of the drugs depends on the individual characteristics of the body and the severity of the patient’s condition, the severity and intensity of the symptomatic picture.
The risks of occurrence and the nature of side effects also differ between drugs, which is associated with some differences in the excipients in the composition.
Comparison of addiction between Losartan and Lozap
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “syndrome o” in Losartan is quite similar to the similar values in Lozap. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible. At the same time, Losartan has a fairly small value of the “syndrome”, however, the same as Lozap.
Contraindications
Losartan should not be taken in the following cases:
- individual intolerance to individual components;
- pregnancy, lactation;
- severe liver failure;
- Age limit: up to 6 years.
Contraindications to the use of Lozap:
- allergic reaction to the main component or excipients in the composition;
- liver dysfunction with intense symptoms;
- pregnancy;
- breastfeeding period;
- age limit - up to 18 years (there is no data on the specific effects of the medication on the child’s body).
Both medications are strictly prohibited from being taken in combination therapy with medications that contain the substance aliskiren (regardless of its concentration) and ACE inhibitors.
How to take Lozap and Losartan?
The tablets are taken orally, regardless of food intake. Dosages for treatment with Lozap:
- Arterial hypertension - therapy must be started with a minimum dosage of 50 mg (1 tablet with 50 mg of the active ingredient or ½ tablet of 100 mg). To achieve a better effect, the dosage can be gradually increased to 100 mg per day. This amount of the drug is the maximum allowed.
- Patients 75 years of age and older (including those with abnormalities in the thyroid gland) - the dosage is reduced to 25 mg or ½ tablet of 50 mg.
- As a prophylactic agent to prevent diseases of the heart and vascular system - 50 mg per day.
- Nephropathy in people with diabetes - 50 mg per day. After a few weeks of the course, it is recommended to increase the dosage to 100 mg.
We recommend reading: Thyrotoxicosis: instructions for using the drug Mercazolil
Recommendations for the use of Losartan and dosages depending on the clinical case are identical to the use of the first drug.
Practical possibilities of using losartan in the treatment of patients with arterial hypertension
For citation. Libov I.A., Itkin D.A., Moiseeva Yu.N. Practical possibilities of using losartan in the treatment of patients with arterial hypertension // RMZh. 2015. No. 27. pp. 1584–1589.
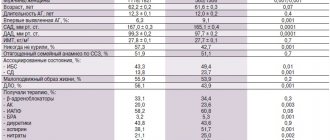
Arterial hypertension (HTN) remains the most important risk factor for the development of cardiovascular diseases (CVD). Control over blood pressure (BP) levels in Russia has not improved significantly in recent years. Achievement of target blood pressure levels remains very low, despite the fact that, according to the latest European and Russian recommendations, blood pressure reduction is <140/90 mmHg. Art. is sufficient (for patients with diabetes – <140/85 mm Hg) [1, 2]. Among patients who are aware of their disease and take antihypertensive drugs, the target blood pressure level is achieved in approximately 23% (Fig. 1) [2, 3]. The emergence of a large number of new drugs that lower blood pressure, on the one hand, expands treatment options, and on the other, requires the practitioner to rationally select a drug, taking into account the presence of risk factors (RFs), target organ damage (TOD) and concomitant diseases. In the case of monotherapy, patients with hypertension are usually prescribed 1 of 5 main classes of antihypertensive drugs: diuretics, beta-blockers (BAB), calcium channel antagonists, angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs, sartans). C. Thomopoulos, G. Parati, A. Zancheti in the latest meta-analysis (2015) based on 68 randomized placebo-controlled trials (RCTs) showed that lowering blood pressure with any of the 5 main classes of antihypertensive drugs leads to a reduction in the number of strokes and major cardiovascular events events [4]. However, the rate at which these events are prevented is related not only to the degree of blood pressure reduction and the statistical power of the study, but also to the class of drug used, as well as other additional factors.
Prior to the results of the LIFE study [5], many comparative studies to identify the “best” class of antihypertensive drugs did not show a significant difference between classes in the number of cardiovascular events. This may have been due to different endpoints in these original studies. For example, some did not include complications such as transient ischemic attacks (TIAs), development of angina, need for revascularization, and nonfatal heart failure. Therefore, the authors' final meta-analysis included 55 studies, including 5 main antihypertensive classes and centrally acting drugs. It is important to understand that the evaluation of such antihypertensive classes as diuretics, beta blockers, ACE inhibitors was most often carried out in comparison with placebo, while the analysis of the effectiveness of sartans that appeared later was carried out on the basis of comparative studies with other classes of antihypertensive drugs (for example, sartans vs beta blockers , sartans against ACE inhibitors or combinations thereof). This emphasizes the importance of conducting meta-analysis or direct comparative studies of drugs with each other, taking into account the homogeneity of patient groups, the presence of additional risk factors, the selection of adequate doses and appropriate representatives of these classes. This meta-analysis included all major studies on the treatment of patients with hypertension that ended before August 31, 2014, studies where patients with hypertension accounted for 40% or more and in which diseases such as acute myocardial infarction (AMI), acute stroke were not included in the inclusion criteria , heart failure, as well as patients on hemodialysis. A meta-analysis by C. Thomopoulos et al., which assessed the effect of sartans on primary endpoints excluding coronary heart disease (CHD), showed the high effectiveness of this class and the possibility of reducing cardiovascular mortality during treatment for 5 years by an average of 7–9 %. When treating 1000 patients with hypertension with ARBs for 5 years, the development of 9 strokes, 7 cases of severe CHF and 20 major cardiovascular complications can be prevented (NNT=114, 144 and 50, respectively). These 5 groups of antihypertensive drugs can be used not only for monotherapy, but also as a basis for combination treatment. In European (2013) and Russian recommendations, sartans have the largest number of additional indications for the treatment of patients with hypertension [1, 2]. If in 2001, in the Russian recommendations for the treatment of hypertension, the indication for the use of sartans was the appearance of cough while taking ACE inhibitors, then as the data obtained in RCTs accumulated, the indications for their use gradually expanded (Table 1).
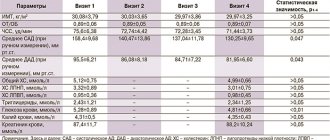
The use of monotherapy, unfortunately, allows achieving the target blood pressure level only in 50% of patients with stage I hypertension or in the presence of 1-2 risk factors. In more severe patients with 3 or more risk factors or a higher degree of hypertension, combination therapy is required in most cases. According to the latest statistics, the prevalence of monotherapy in Russia is higher than in other countries. Being the founder of ARB drugs, losartan has a pronounced hypotensive effect and, according to a number of studies, is not inferior to representatives of this group. Thus, in a multicenter RCT, losartan was administered at a dose of 50 mg/day for 12 weeks. allowed to achieve by the 6th week. treatment of blood pressure control in 48% of patients with mild and moderate hypertension [5]. In case of failure to achieve blood pressure control, the dose was doubled, which was noted in 61% of patients, and made it possible to increase blood pressure control to 54%. In starting doses and after titration, losartan and valsartan 80 and 160 mg showed comparable effectiveness in lowering blood pressure in patients with mild and moderate hypertension (grades I and II according to the modern classification). This thesis has been confirmed by a number of studies (Table 2).
A number of studies noted a more pronounced hypotensive effect of other angiotensin II antagonists when compared with losartan, but here the differences were insignificant [6]. In a multicenter RCT that compared the effectiveness of olmesartan, losartan, valsartan, and irbesartan in patients with essential hypertension, losartan was only slightly inferior to olmesartan in reducing diastolic blood pressure and was not inferior to 2 other ATI angiotensin II receptor blockers [7]. The use of ARBs together with NSAIDs can reduce their hypotensive effect, since the latter disrupt the synthesis of prostaglandins I2 and E2, which are powerful stimulators of renin secretion, and a decrease in RAAS activity weakens the hypotensive effect of ARBs. However, in the work of M. Olsen M. et al. (1998–1999) assessed the hemodynamic effects of losartan at a dose of 50–100 mg/day in a double-blind crossover method in 10 patients with hypertension against the background of 7-day use of indomethacin 50 mg 2 times/day or placebo. A significant increase in body weight and extracellular fluid volume was detected while taking indomethacin, but the data from repeated measurements of office blood pressure in a sitting position and the data from 24-hour blood pressure monitoring did not change significantly. There was a tendency to increase systolic blood pressure during the day and decrease it in the evening and at night. The authors do not exclude that longer use of NSAIDs may have a greater effect on the hypotensive effect of losartan. In another work, P. Conlin et al. (2000) use of indomethacin retard at a dose of 75 mg/day. during the treatment of 111 patients with hypertension, losartan at a dose of 50–100 mg with 24-hour blood pressure monitoring significantly increased the level of SBP and DBP (more than 68% of patients), which shows a weakening of the hypotensive effect of losartan when combined with NSAIDs [8–12]. The effect of acetylsalicylic acid (ASA) in the treatment of patients with hypertension with ATI receptor blockers is also controversial. A number of meta-analyses, in particular in patients with CHF, have shown the absence of a negative effect of ASA on the antihypertensive effectiveness of sartans; in other studies and meta-analyses, this effectiveness decreased. Taking into account modern recommendations, when using acetylsalicylic acid, it is necessary to strive for its use in minimal doses - 75–100 mg / day, and in cases where the positive effect of aspirin is in doubt, one should refrain from using it together with BRAS. Discussing the effectiveness of the main classes of antihypertensive drugs, it should be noted that, despite their slight differences in their effect on lowering blood pressure and main endpoints, according to recent meta-analyses, some features have been noted: for example, diuretics have shown to be significantly better in terms of preventing heart failure , and beta blockers are the least effective for preventing strokes. At the same time, calcium antagonists appear to be better than others in preventing cerebral complications and overall mortality, but are less effective than others in patients with CHF. ACE inhibitors turned out to be very useful for the prevention of coronary artery disease and are somewhat inferior in the prevention of stroke. All RAAS blockers are most effective for the prevention of heart failure, but sartans are inferior to ACE inhibitors in the prevention of coronary artery disease [4]. Therefore, comparison of different classes of antihypertensive drugs does not allow us to definitely recommend any of them depending on the situation, but one or another class or their rational combination may be preferred. The combination of a renin-angiotensin-aldosterone system (ARAS) blocker (ACEI or sartans) with calcium antagonists and/or diuretics is currently considered the most rational and frequently used. At the same time, as indicated, the prognosis of the disease, along with achieving the target blood pressure level, is also determined by the influence on the modification of risk factors, the prevention of POM and CVD. Left ventricular myocardial hypertrophy (LVH) is one of the most common and important factors influencing the prognosis and course of the disease [5]. An increase in the thickness of the posterior wall of the LV by just 1 mm increases the risk of developing myocardial infarction and stroke. In this regard, in recent years the criteria for assessing LVH have been tightened. One of the most important indicators characterizing LVH is the determination of the LV myocardial mass index (LVMI) according to echocardiography (Echo-CG). Currently, the criteria for LVH according to LVMI have been tightened for women from 110 to 95 g/m2, and for men - from 125 to 115 g/m2. Preventing the development of LVH or its regression in patients with hypertension significantly improves the prognosis of the disease, and therefore control of this indicator seems extremely important. Several RCTs (HOPE, SYSTEUR) revealed a significant correlation between the development of cardiovascular complications and regression or prevention of the development of LVH [13, 14]. When examining patients with hypertension and LVH, LV diastolic dysfunction is often recorded even before the onset of systolic dysfunction. Thus, according to M. Iriartek et al. (1995), in an echo-CG study of patients with hypertension using the Doppler method and determining E/A ≤0.8, disturbances were observed in 90% of patients with LVH, 25% of patients with hypertension without LVH, and only 8% of people without hypertension. Timely initiation and successful therapy allows the majority of these patients to prevent the subsequent development of severe LV systolic dysfunction with clinical manifestations of heart failure. The important role of diastolic dysfunction in patients with hypertension and LVH can be evidenced by the fact that 20 years ago the proposed echocardiographic classification of “hypertensive heart” implied the definition of grade I based on the presence of diastolic dysfunction, and grade II when combined with signs of LVH [15 ]. For grade III, clinical manifestations of chronic heart failure (CHF) were required with preserved ejection fraction (EF) >50%, and only grade IV was characterized by a decrease in LV systolic function with EF <50% along with dilatation of the heart chambers. In recent years, many studies have confirmed the frequent occurrence of diastolic dysfunction in patients with hypertension and LVH, which precedes the further development of systolic dysfunction [16].
In the multicenter RCT EDEN (The Effect of Losartan plus Hydrochlortiazide Combination on Therapy on Left Ventricular Diastolic Function in Patient with Hypertension), the use of a combination of losartan/hydrochlorothiazide significantly improved LV diastolic function in terms of parameters e and E/e with dynamic monitoring of echocardiography [17 ]. These data were confirmed by a significant (p<0.001) decrease in such an important marker of heart failure as brain natriuretic peptide (BNP) over 24 weeks. treatment. The same study demonstrated the possibility of a significant decrease in left atrial volume during treatment with a combination of these drugs, which helps explain the decrease in the incidence of atrial fibrillation (AF). In the LIFE study, in patients with hypertension and LVH in the group treated with losartan, compared with the group treated with atenolol, AF paroxysms were recorded 33% less often [5]. These studies largely predetermined the use of losartan as a component of upstream therapy in patients with hypertension and paroxysmal AF. A meta-analysis by A. Kirhlau et al. (2006), indicated a decrease in the number of new patients with AF during treatment with BRAS by 18% (CI = 0.70-0.97). But when analyzing patients specifically with hypertension, only losartan, according to the LIFE study, made it possible to significantly reduce the number of new cases of AF by 33% (CI = 0.54-0.81). Among the various ATI angiotensin II receptor blockers, losartan stands out for its unique ability to reduce uric acid levels. This effect is due to the action of losartan, and not its main metabolite EXP-3174, which plays a leading role in the hypotensive effect of the drug. The use of losartan leads to an increase in the excretion of uric acid in the urine and causes a decrease in its serum concentration in the blood. The LIFE study showed a highly significant dose-dependent reduction in uric acid levels with the use of losartan [5]. This led to the recommendation of the European Society of Rheumatology regarding the choice of losartan as the first drug in patients with gout and elevated blood pressure [18]. The possibility of reducing elevated uric acid levels in patients with hypertension with the use of other sartans or ACE inhibitors does not have such a strong evidence base, and although some studies indicate such a possibility, the uricosuric effect of losartan seems much stronger and more convincing. Prevention of strokes in patients with hypertension during antihypertensive therapy is one of the most important tasks of a general practitioner. In this matter, preventive treatment seems to us even more important than treatment of an event that has already occurred. We have already mentioned that there are not too many direct RCTs comparing different classes of drugs with similar designs and identical endpoints. So it makes sense to take a closer look at another meta-analysis from 2015, which compared the effects of different antihypertensive drugs on the risk of stroke in 227,754 patients across 17 studies. Meta-analysis revealed a significant reduction in the number of strokes by 17% (CI=0.79-0.89, p<0.01) with the use of calcium channel antagonists and a negative role of β-blockers when compared with other classes (CI=1.26- 1.61, p<0.01, average increase by 42%) [19]. ARBs occupy 2nd place in this ranking, although the risk of stroke is also reduced by 17%, but CI = 0.59-1.16, p = 0.03. When assessing the impact of all BRAS (ARBs and ACEIs) on this indicator, the results become significantly worse, and ACEIs studied separately show a tendency (albeit unreliable) towards an increase in the number of strokes. Moreover, if you look closely at the details, of the 6 studies on sartans included in the meta-analysis, only 2 of them (LIFE with losartan and SCOPE with candesartan) recorded a significant positive result with a reduction in the risk of stroke by 42%. The use of other drugs from this group gave very contradictory results. Of all the studies using ACE inhibitors, only the PROGRESS study with perindopril showed similar results [20]. Taking into account the fact that most often in practical work the risk of stroke is greatest in severely ill patients, and the combination of sartan with a calcium channel antagonist is rational, it makes sense to start with it, and if necessary, a diuretic can be added. If there is no effect or the target level is not achieved, you will need to look for other combinations. Despite the fact that all AT-I angiotensin II receptor blockers belong to the same group of medications, have many common effects and a high level of safety in their use, there are certain differences in their pharmacokinetics, which determines the peculiarities of their use and allows in a number of specific cases to implement the most justified choice even among these similar means. Based currently on the data of evidence-based medicine, we can note that if the use of any of the sartans in patients with hypertension can be useful (in this case, individual sensitivity and the absence of side effects are more important), then, for example, according to the indication of CHF, According to the instructions for use and the same evidence base, we can use only 3 of the 8 available sartans, namely losartan, valsartan and candesartan. For the other 5 sartans there are no indications for use in this pathology. This is due not only to the small number of multicenter RCTs. Thus, recently reported at the session of the American Society of Cardiology, the results of a prospective RCT with blinded end points SUPPORT in 1147 outpatients with hypertension and CHF showed that the addition of olmesartan, titrated to 40 mg/day, to basic therapy did not improve clinical outcomes compared with the control group , but worsened renal function in these patients [21]. The effect of losartan in CHF is largely determined by the dose of the drug. Thus, H. Svanström et al. based on results from the Danish Register 1998–2008. demonstrated: in patients over 45 years of age hospitalized for the first time due to CHF, a comparison of overall mortality when using losartan and candesartan showed that losartan at a dose of 12.5 and 50 mg, as well as candesartan at doses of 4,8,16 and 32 mg, did not led to a statistically significant reduction in mortality in more than 7500 patients [22]. A 100 mg dose of losartan caused a significant reduction in overall mortality (CI=0.49-1.00). This work makes it possible to correctly evaluate the results of the ELITE-II study, where the use of losartan, titrated at a dose of 12.5 to 50 mg/day in patients with CHF, did not surpass the use of the ACE inhibitor captopril, titrated to the maximum permitted dose of 150 mg/day. Secondary endpoints such as progression of CHF and the number of hospitalizations also did not significantly decrease. Despite fewer adverse effects in the losartan-treated group compared with those in the captopril-treated group, a reduction in all-cause mortality was not achieved [23]. Excellent tolerability and low incidence of side effects in treatment with sartans (in particular losartan), comparable to placebo, make this class of antihypertensive drugs the most attractive. High efficiency and a small number of side effects lead to the fact that patient adherence to treatment with these drugs is significantly higher compared to that with the use of other main classes of antihypertensive drugs. In practical work, the most common cause of increased blood pressure above target levels and the development of cardiovascular complications is irregular use or self-cessation of antihypertensive drugs. The main reasons for low adherence to therapy are the occurrence of side effects and insufficient effectiveness of the drugs. The low incidence of adverse events, even among BRAS, currently puts sartans at a leading position in the treatment of hypertension. The extremely rare development of dry cough, in contrast to ACE inhibitors, which is largely associated with the influence of substance P and, especially, introkinin A, gives sartans an advantage, which practitioners are mostly aware of. Another, less frequent, but more dangerous complication in the treatment of ACE inhibitors is the occurrence of angioedema, which in some cases is combined with laryngospasm and laryngeal edema and can be a life-threatening condition. In the monograph by B.A. Sidorenko and D.V. Preobrazhensky noted that in almost 60% of patients with this complication, the relationship between taking ACE inhibitors and angioedema is revealed only after several months, or patients continue taking ACE inhibitors after the symptoms disappear. The greatest risk is in patients with multivalent allergies or those who have previously experienced angioedema after using another ACE inhibitor [24]. In a large meta-analysis by A.Y. Gupta, N. Chapman and F. Dixson, the risk of angioedema with routine use of sartans is small and amounts to ≈ 0.03% of cases. However, the use of sartans in patients with hypertension, in whom angioedema was registered during previous ACE inhibitor therapy, increases the risk of its possible occurrence by 2–17 times [25]. According to this meta-analysis, it reaches 0.11% per year, but even in this category of patients it accounts for less than half of the cases that occur during treatment with ACE inhibitors. When comparing candesartan, telmisartan, valsartan and losartan, the latter is associated with the least number of cases and is significantly less likely to cause this complication. The frequent combination of hypertension as the most important risk factor for the development of cardiovascular complications and coronary artery disease determines the importance of metabolic neutrality or, preferably, the positive lipid-lowering effect of antihypertensive drugs. In the work of S.-M. Kyvelou, GP Vyssoulis, EA Karpanou showed the ability of sartans, along with a significant decrease in blood pressure, to improve lipid metabolism [26]. In 2438 patients with hypertension, observed for 6 months. and receiving monotherapy with sartans, a significant decrease in the level of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), apolipoprotein B and triglycerides (TG) was noted. At the same time, a significant increase in the level of high-density lipoprotein cholesterol (HDL-C) was also noted. In terms of its positive effect on increasing HDL-C levels, losartan showed itself to be a leader among other sartans. Another important niche for the practical use of losartan turned out to be Marfan syndrome. In experimental studies on animals, a decrease in the expansion of the aortic root was noted when using this drug. Conducted by M. Groenink, AW Den Hartog, R. Franken et al. A study in 145 adult patients with Marfan syndrome showed that the addition of losartan to standard beta blocker treatment reduced the dilation of the aortic root and arch, including in patients after surgical treatment [27]. In the work of RV Lacto, HC Dietz, LA Sleeper et al. the use of losartan at an average dose of 85 mg versus atenolol 151 mg showed comparable effectiveness of both drugs for the prevention of aortic root enlargement [28]. Thus, based on the scientific studies available to us and the latest meta-analyses, we tried to identify for practitioners those main niches where the use of ATI angiotensin II receptor blockers and, in particular, losartan may be most appropriate. I would like to draw attention to those cases where the combination of hypertension with certain risk factors, POM and cardiovascular complications has the most significant evidence base for the use of losartan and where our own clinical experience allows us to believe that this group of drugs will be the most effective and safe. In real clinical practice, high-quality generic drugs are increasingly used, but even among them we try to choose those that have their own evidence base. Thus, in the CORD study [29], the hypotensive effect and the effect on the prevention of cardiovascular complications of one of the best ACE inhibitors, ramipril, were compared with those of the generic losartan (Lozap, Zentiva, Czech Republic). The study showed that in the groups treated with ramipril 5 mg and Lozap 50 mg, as well as ramipril 10 mg and Lozap 100 mg, the hypotensive effect and the effect on the prevention of cardiovascular events were not statistically significantly different. At the same time, the number of adverse events in the group of patients taking Lozap was 8 times less common. The antihypertensive effectiveness of the drugs Lozap and Lozap plus was also assessed in an open, sequential, prospective, non-comparative Russian study by I.E. Chazovoy et al. [thirty]. The study showed that Lozap and Lozap plus provide a stable, uniform antihypertensive effect over 24 hours and have a positive corrective effect on the daily blood pressure profile, allowing most patients to achieve the target blood pressure level and increase treatment adherence. The use of Lozap and Lozap plus was characterized by high adherence to treatment. Up to 92% of patients continued taking the drug after the end of the study. High efficiency, as well as good tolerability and adherence to treatment with Lozap and Lozap plus allow most patients to achieve the target blood pressure level and prevent the development of POM and associated clinical diseases.
Side effects of Lozap and Losartan
Negative reaction of the body to taking Losartan:
- common side symptom: attacks of dizziness and drowsiness;
- lymphatic system: anemia;
- mental disorders: depression;
- central nervous system: drowsiness and apathy, headaches and dizziness, migraines;
- immune system: anaphylactic reaction;
- respiratory system: dry cough, shortness of breath;
- skin: itching and redness, urticaria;
- organs of the gastrointestinal tract: pain in the abdomen, nausea, less often vomiting, diarrhea;
- reproductive system: impotence, erectile disorders.
Possible side effects from using Lozap:
- blood and lymphatic system: anemia, less often - thrombocytopenia;
- immune system: Quincke's edema, allergies, extremely rarely - anaphylactic shock;
- psyche: depression;
- central nervous system: migraine, change in taste, insomnia, dizziness, drowsiness;
- vision and hearing: vertigo, ringing in the ears;
- heart: fainting, angina pectoris; extremely rare: circulatory disorders in the brain;
- vascular system: decreased blood pressure;
- respiratory system: shortness of breath;
- digestive system: nausea and vomiting, diarrhea, intestinal obstruction, pain in the stomach and abdomen;
- liver: hepatitis, pancreatitis;
- skin: itching, urticaria.
An overdose of Losartan and Lozap can manifest itself as dizziness and tachycardia, decreased blood pressure, fainting and collapse. In the case of a one-time use of a high dose of the drug with side effects, symptomatic therapy is carried out.
First aid is to lay the victim on his back and raise his legs. If necessary, introduce 0.9% sodium chloride solution. Medicines are prescribed to relieve side symptoms and normalize the patient's condition. Recommended measures are gastric lavage, taking sorbent. After stabilizing the patient’s condition, it is necessary to establish control over the main vital signs, and in case of deviations, carry out their medication adjustment.
Reviews from doctors
Andrey, 35 years old, therapist, Magnitogorsk: “We can say that these are 2 identical drugs with different names. They are equally effective in the treatment and prevention of vascular diseases, but have one common drawback - a positive result from their use is possible only in the case of long-term therapy; if the course of treatment is short or interrupted ahead of time, they will not help. Which remedy to choose, if they are identical, is a matter of individual patient preference.”
We recommend reading: What is the difference between Bisoprolol and Metoprolol?
Svetlana, 58 years old, cardiologist, Ulyanovsk: “There is no difference between the drugs. When choosing a medicine, you need to take into account the patient's possible intolerance to the auxiliary components. If there are no such contraindications, you can choose a drug based on its cost.”
Which is better Lozap or Losartan
According to experts, these are drugs that are equivalent in their principle of action, differing only in name, price and manufacturer. But they must be taken as prescribed by a doctor, so as not to aggravate the effectiveness of the parallel actions of auxiliary ingredients. The main concerns relate to diuretic supplements. On the advice of Myasnikov A.L. (cardiologist), when choosing antihypertensive drugs, it is necessary to be guided by the level of uric acid in the blood. With its increased content and the use of medications without diuretics, there is a risk of arthrosis.
Patient reviews
Marina, 48 years old, Kursk: “The doctor initially prescribed Lozap, but I decided to buy Losartan, because its price is slightly lower, and the pharmacist at the pharmacy said that it is no less effective than the first. But, as experience has shown, they are not exactly the same, because I didn’t get any particular effect from it, and after a few weeks an allergy began to appear. I had to switch to the more expensive Lozap, which I tolerated well, there were no allergies and no other adverse reactions.”
Kirill, 39 years old, Ivanovo: “At first I took Lozap, then in order to save money, since the course of treatment was going to be long, I switched to Losartan. I did not feel any difference from changing the drug. I decided that it wasn’t worth paying more if both remedies helped equally well and were well tolerated, and I didn’t have any side symptoms.”
Oksana, 51 years old, Kyiv: “My story is about how I decided that expensive means high quality, so instead of Losartan I bought Lozap. It helped, but it just started to cause nausea, dizziness, and a skin rash. When the doctor prescribed Losartan, which at first I didn’t really trust because of its low price, I didn’t have any side effects. And it even seemed that it was more effective than Lozap.”