Composition and release form
The drug Lozap is available in the form of small tablets for parenteral administration. They are white, slightly elongated and convex on both sides. They have a soluble thin film shell. Packaged in blisters of 10 pieces. One cardboard package contains 3, 6, 9 blisters and includes instructions for use.
The active substance is potassium losartran.
Auxiliary components: cellulose, povidone, talc, magnesium stearate, macrogol, dyes, mannitol, croscarmellose sodium.
Note!
Description of the drug Lozap Plus table. p/o No. 90 on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
pharmachologic effect
The drug belongs to the group of antihypertensive drugs. It is a specific angiotensin receptor agonist. After taking the medicine, there is a decrease in vascular resistance, a decrease in aldosterone and adrenaline levels in the bloodstream. In addition, the pressure in the pulmonary circulation is normalized, a pronounced diuretic effect occurs and the afterload on the body is reduced.
The drug prevents the development of hypertrophy of the muscular lining of the heart and improves people's susceptibility to physical activity.
While taking the drug, the angiotensin-containing enzyme is not blocked. Therefore, the level of bradykinin does not increase and the effect on the kinin system is prevented.
The pharmacological effect of the drug is the same for all patients, regardless of age and gender.
After one dose of medication, the hypotensive effect is observed after 6 hours and gradually decreases throughout the day. When a course is prescribed, pronounced results of therapy appear in patients after 3-4 weeks.
People suffering from liver cirrhosis should be careful when using antihypertensive drugs. The active ingredient occurs in their blood. Therefore, they need dose adjustment.
After oral administration, the tablets are quickly absorbed. The maximum content of the drug in the body is recorded after an hour. The drug is administered through the kidneys and intestines.
special instructions
It is necessary to prescribe with caution to the following categories of patients:
- with water-electrolyte imbalance (dehydration, hyponatremia, hypochloremic alkalosis, hypomagnesemia, hypokalemia), which can develop with intercurrent diarrhea or vomiting;
- with bilateral renal artery stenosis or stenosis of the artery of a single kidney; diabetes mellitus, hypercalcemia, hyperuricemia and/or gout; with a burdened allergic history and asthma; for systemic connective tissue diseases (including systemic lupus erythematosus); hypovolemia (including due to the use of diuretics in high doses); when administered concomitantly with NSAIDs, including COX-2 inhibitors.
Losartan. Renal dysfunction. There are reports that some patients who took the drug, due to inhibition of the function of the renin-angiotensin system, experienced changes in renal function, including renal failure; these changes may be reversible and disappear after cessation of therapy.
Other drugs that affect the renin-angiotensin system may cause increases in urea and creatinine in the blood of patients with bilateral renal artery stenosis and solitary renal artery stenosis.
Similar effects were noted when taking losartan; these changes in renal function may be reversible and disappear after discontinuation of therapy.
Hydrochlorothiazide. Arterial hypotension and water-electrolyte imbalance. As with all antihypertensive agents, symptomatic hypotension may occur in some patients. Patients should be monitored for clinical signs of fluid and electrolyte imbalance, such as dehydration, hyponatremia, hypochloremic alkalosis, hypomagnesemia, or hypokalemia, which may occur with intercurrent diarrhea or vomiting. In such patients, it is necessary to monitor the level of electrolytes in the blood plasma.
Metabolic and endocrine effects. Thiazide therapy may impair glucose tolerance. In some cases, dose adjustment of hypoglycemic agents, including insulin, may be required.
Thiazides may reduce urinary calcium excretion and cause occasional and mild increases in plasma calcium levels. Severe hypercalcemia may indicate latent hyperparathyroidism. It is necessary to stop taking the thiazide diuretic before testing the functions of the parathyroid glands.
Increased levels of cholesterol and TG in the blood may also be associated with therapy with thiazide diuretics.
In some patients, the use of thiazide diuretics can cause hyperuricemia and/or gout. Because losartan reduces uric acid levels, its combination with hydrochlorothiazide reduces the severity of diuretic-induced hyperuricemia.
Other effects. In patients using thiazide diuretics, hypersensitivity reactions may occur even in the absence of indications of allergies or a history of asthma. There are reports of exacerbation or progression of systemic lupus erythematosus when using thiazide diuretics.
The use of the drug may affect the speed of psychomotor reactions.
Lozap indication
The use of Lozap is relevant for the following conditions:
- High blood pressure.
- Chronic course of heart failure.
- Prevention of the development of severe vascular and cardiac diseases among patients with hypertension and left ventricular enlargement.
- Nephropathy and high blood pressure in people with diabetes.
- Contraindications
- Absolute contraindications for use are:
- Increase in potassium levels in the blood.
- Low pressure.
- Individual intolerance to the medicinal components included in the composition.
- The time of bearing a child.
- Breastfeeding.
- Symptoms of dehydration.
- Children under 18 years of age.
Side effects
As a rule, during the course of therapy, patients experience virtually no side effects. If they appear, they go away on their own and quickly, so there is no need to discontinue the drug. The following side effects are possible when taking Lozap:
- Dizziness, increased fatigue, headache, problems falling asleep. Migraines, anxiety, tremor, and depression are less common.
- Infection of the respiratory system. Signs of rhinitis, bronchitis and respiratory distress may appear.
- Dyspeptic symptoms, rarely gastritis, dry mouth, flatulence.
- Disturbance of the musculoskeletal system. Possible pain in the back and muscles, cramps.
- Signs of cardiac dysfunction are expressed in tachycardia, bradycardia, arrhythmia.
- Rarely, kidney problems, sexual dysfunction and infections of the urinary system appear.
- Allergic reactions, dry dermis, excessive sweating.
Overdose
There is no data on specific treatment for drug overdose. in case of overdose, therapy must be stopped and the patient must be under medical supervision. if the drug has been taken recently, it is necessary to induce vomiting and take measures aimed at eliminating dehydration, electrolyte disturbances, hepatic coma and hypotension. Treatment is symptomatic and supportive.
Losartan. Data on drug overdose in humans are limited. The most likely manifestations of an overdose are hypotension and tachycardia; bradycardia may result from parasympathetic (vagal) stimulation. In case of symptomatic arterial hypotension, maintenance therapy is indicated. Losartan and its active metabolite are not eliminated by hemodialysis.
Hydrochlorothiazide. The most commonly reported symptoms of overdose are due to electrolyte deficiency (hypokalemia, hypochloremia, hyponatremia) and dehydration due to excessive urination. When taking cardiac glycosides simultaneously, hypokalemia can cause an increase in the severity of arrhythmia. Hydrochlorothiazide is eliminated by hemodialysis, but the extent of elimination has not been established.
Instructions for use of Lozap
The medicine is intended for oral administration, regardless of the time of meal. It is recommended to take the tablets once a day.
For severe hypertension, patients are prescribed 50 mg. According to clinical indications, the dosage can be doubled.
According to the attached instructions, in case of cardiac insufficiency, patients are prescribed 12.5 mg once a day. Every week the dose of the drug is increased by 2 times until it reaches 50 mg per day.
In cases where patients are simultaneously taking diuretic drugs, the therapeutic dose of Lozap should be reduced to 25 mg.
Elderly people and those with kidney problems do not need to change the therapeutic dosage.
Lozap® AM
Pharmacological properties
Drug Lozap® AM
The results of two bioequivalence studies involving healthy volunteers showed that Lozap® AM in doses of 5 mg + 50 mg and 5 mg + 100 mg is bioequivalent to the combined use of corresponding doses of amlodipine camsylate and losartan potassium in the form of separate tablets.
Amlodipine
The bioequivalence of amlodipine besylate and amlodipine camsylate was assessed in a randomized, blinded, crossover study in healthy volunteers. The results obtained in the study showed that amlodipine camsylate 5 mg tablets are bioequivalent to amlodipine besylate 5 mg tablets.
Mechanism of action
Drug Lozap® AM
The drug Lozap® AM contains two active substances with a complementary mechanism of action to improve blood pressure (BP) control in patients with arterial hypertension (AH): losartan potassium, an angiotensin II receptor antagonist (ARA II), and amlodipine, a blocker " slow" calcium channels (SCMC).
Losartan blocks the vasoconstrictor effect of angiotensin II and the latter's stimulation of aldosterone release by selectively inhibiting the binding of angiotensin II to AT1 receptors in many tissues.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle, resulting in a decrease in peripheral vascular resistance and a decrease in blood pressure.
Losartan
Angiotensin II is a powerful vasoconstrictor, the main active hormone of the renin-angiotensin-aldosterone system (RAAS), as well as a decisive pathophysiological link in the development of hypertension.
Angiotensin II binds to AT1 receptors found in many tissues (vascular smooth muscle, adrenal glands, kidneys and heart) and performs several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates the proliferation of smooth muscle cells.
AT2 receptors are the second type of receptor to which angiotensin II binds, but its role in the regulation of cardiovascular function is unknown.
Losartan is a selective antagonist of AT1 - angiotensin II receptors, highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174) both in vitro and in vivo block all physiological effects of angiotensin II, regardless of its source or route of synthesis.
Unlike some peptide angiotensin II antagonists, losartan does not have agonist properties.
Losartan selectively binds to AT1 receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in regulating the function of the cardiovascular system. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for the destruction of bradykinin. Therefore, effects not directly related to AT1 receptor blockade, such as increased bradykinin-mediated effects or the development of edema (losartan 1.7%, placebo 1.9%), are not related to the action of losartan.
Amlodipine
Amlodipine is a dihydropyridine calcium antagonist (calcium ion antagonist or slow channel blocker) that inhibits the transmembrane entry of calcium ions into vascular smooth muscle cells and cardiomyocytes.
Experimental data suggest that amlodipine binds to both dihydropyridine and non-dihydropyridine binding sites on slow calcium channel receptors. The process of contraction of the myocardium and vascular smooth muscle depends on the transmembrane entry into the cell of extracellular calcium ions through specific ion channels. Amlodipine selectively inhibits transmembrane calcium entry, affecting vascular smooth muscle cells more than cardiomyocytes.
In vitro
a negative inotropic effect can be detected, however, in studies on intact animals using amlodipine in therapeutic doses, this effect was not detected. Amlodipine does not affect serum calcium levels. Within the physiological pH range, amlodipine is an ionized compound (pKa = 8.6), and its kinetic interaction with the calcium channel receptor is characterized by gradual association and dissociation with the receptor binding site, which leads to a gradual development of the effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle, which leads to a decrease in peripheral vascular resistance and a decrease in blood pressure.
Pharmacodynamics
Drug Lozap® AM
The drug Lozap®AM has been shown to effectively reduce blood pressure. Both losartan and amlodipine reduce blood pressure by reducing peripheral resistance. Blocking the entry of calcium into the cell and reducing the vasoconstrictive effect caused by the action of angiotensin II are complementary mechanisms.
Losartan
Losartan suppresses the increase in systolic and diastolic blood pressure during angiotensin II infusion. At the moment of reaching the maximum concentration (Cmax) of losartan in the blood plasma after taking losartan at a dose of 100 mg, the above effect of angiotensin II is suppressed by approximately 85%, and 24 hours after single and multiple doses - by 26-39%.
During the period of taking losartan, elimination of the negative feedback, which consists in the suppression of renin secretion by angiotensin II, leads to an increase in plasma renin activity (PRA). An increase in ARP leads to an increase in the concentration of angiotensin II in the blood plasma. With long-term (6-week) treatment of patients with hypertension with losartan at a dose of 100 mg/day, a 2-3-fold increase in the concentration of angiotensin II in the blood plasma was observed at the time the losartan Cmax was reached.
In some patients, an even greater increase in angiotensin II concentrations was observed, especially with a short duration of treatment (2 weeks). Despite this, during treatment, an antihypertensive effect and a decrease in plasma aldosterone concentrations appeared after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to the values observed before the start of losartan administration.
Since losartan is a specific antagonist of angiotensin II AT1 receptors, it does not inhibit ACE (kininase II), an enzyme that inactivates bradykinin. A study comparing the effects of losartan at doses of 20 mg and 100 mg with the effects of an ACE inhibitor on angiotensin I, angiotensin II and bradykinin showed that losartan blocked the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked responses to angiotensin I and increased the effects due to bradykinin without affecting the response to angiotensin II, demonstrating a pharmacodynamic difference between losartan and ACE inhibitors.
Plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing dose of the drug. Since losartan and its active metabolite are angiotensin II receptor antagonists, they both contribute to the antihypertensive effect.
In a study with a single dose of 100 mg of losartan, which included healthy volunteers (men), oral administration of the drug under high- and low-salt diets did not affect the glomerular filtration rate (GFR), effective renal plasma flow and filtration fraction. Losartan had a natriuretic effect that was more pronounced with a low-salt diet and did not appear to be associated with suppression of early sodium reabsorption in the proximal renal tubules.
Losartan also caused a transient increase in renal excretion of uric acid.
In patients with hypertension, proteinuria (at least 2 g/24 hours), without diabetes mellitus and taking losartan for 8 weeks at a dose of 50 mg with a gradual increase to 100 mg, a significant decrease in proteinuria (by 42%), fractional excretion of albumin was observed and immunoglobulins (IgG). In these patients, losartan stabilized GFR and reduced the filtration fraction.
In postmenopausal women with hypertension who took losartan at a dose of 50 mg for 4 weeks, there was no effect of therapy on the renal and systemic levels of prostaglandins.
Losartan does not affect autonomic reflexes and does not have a long-term effect on the concentration of norepinephrine in the blood plasma.
In patients with hypertension, losartan in doses up to 150 mg/day did not cause clinically significant changes in the concentration of fasting triglycerides, total cholesterol and high-density lipoprotein cholesterol. At the same doses, losartan had no effect on fasting blood glucose concentrations.
In general, losartan caused a decrease in serum uric acid concentrations (usually less than 0.4 mg/dL) that persisted during long-term treatment. In controlled clinical studies involving patients with hypertension, no cases of drug withdrawal due to an increase in creatinine concentration or serum potassium levels were recorded.
A 12-week parallel study, which included patients with left ventricular failure (NYHA functional class II-IV), most of whom were taking diuretics and/or cardiac glycosides, compared the effects of losartan at doses of 2.5, 10, 25 and 50 mg/day with placebo. At doses of 25 and 50 mg/day, the drug exhibited positive hemodynamic and neurohormonal effects, which persisted throughout the study.
Hemodynamic effects included an increase in cardiac index and a decrease in pulmonary capillary wedge pressure, as well as a decrease in total peripheral vascular resistance, mean systemic blood pressure, and heart rate (HR). The incidence of arterial hypotension in these patients depended on the dose of the drug.
Neurohormonal effects included decreased concentrations of aldosterone and norepinephrine in the blood.
Amlodipine
Hemodynamics
In patients with hypertension, after taking therapeutic doses, amlodipine causes vasodilation, which leads to a decrease in blood pressure in the supine and standing positions. This decrease in blood pressure is not accompanied by significant changes in heart rate or plasma catecholamine concentrations with long-term use. Although in studies evaluating hemodynamic parameters in patients with stable angina pectoris, a decrease in blood pressure and an increase in heart rate was observed with a single intravenous administration of amlodipine, in clinical studies, repeated oral administration of amlodipine did not lead to clinically significant changes in heart rate or blood pressure in normotensive patients with angina pectoris.
With long-term oral administration once a day, the antihypertensive effect persists for at least 24 hours. The concentration of amlodipine in the blood plasma correlates with the antihypertensive effect in both young and elderly patients. The magnitude of the decrease in blood pressure when taking amlodipine also correlates with the severity of the increase in blood pressure before treatment. Thus, patients with moderate hypertension (diastolic pressure 105-114 mm Hg) had an approximately 50% greater antihypertensive effect than patients with mild hypertension (diastolic pressure 90-104 mm Hg. ).
In patients with normal blood pressure, no clinically significant changes in blood pressure were observed (+1/-2 mmHg).
In patients with hypertension and normal renal function, taking amlodipine in therapeutic doses led to a decrease in renal vascular resistance, an increase in GFR and effective renal plasma flow without changing the filtration fraction or proteinuria.
As with other CBCMs, hemodynamic parameters of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine generally showed a slight increase in cardiac index without a significant change in the rate of increase in left ventricular cavity pressure at the beginning of the period. ejection (dP/dt) or left ventricular end-diastolic pressure or volume. In studies assessing hemodynamic parameters, amlodipine did not have a negative inotropic effect when used at therapeutic doses in healthy volunteers, even when used simultaneously with beta-blockers. However, similar results were observed in healthy volunteers or in patients with heart failure in the compensation stage when using drugs that have a pronounced negative inotropic effect.
Electrophysiological effects
Amlodipine did not affect sinoatrial node function or atrioventricular conduction in healthy volunteers. In patients with chronic stable angina, intravenous administration of 10 mg amlodipine did not have a significant effect on A-H and HV conduction and sinus node recovery time after cardiac stimulation.
Similar results were obtained in patients taking amlodipine and beta-blockers concomitantly.
In clinical studies in which patients with hypertension or angina pectoris took amlodipine concomitantly with beta-blockers, no adverse effects on electrocardiographic parameters were observed.
In clinical studies in patients with angina only, amlodipine therapy did not affect electrocardiographic intervals or cause greater atrioventricular block.
Interactions with drugs
Combining the drug with Fluconazole and Rifampicin leads to a decrease in the active substance.
Lozap increases the pharmacological activity of other antihypertensive drugs.
It is not recommended to take the medicine in parallel with non-steroidal anti-inflammatory drugs.
When interacting with potassium and potassium-sparing diuretics, it is important to monitor the level of the element in the blood to prevent the occurrence of hyperkalemia.
Patients with obvious symptoms of dehydration while taking diuretics may experience a rapid decrease in blood pressure when taking an antihypertensive drug.
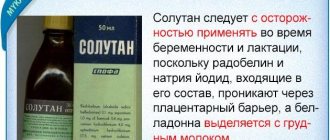
Use during pregnancy and breastfeeding
BRA II. The use of angiotensin II blockers during pregnancy is contraindicated. Patients planning pregnancy should switch to alternative antihypertensive therapy options with an established safety profile. If pregnancy is diagnosed during treatment, therapy with Lozap® plus should be stopped immediately and alternative treatment should be started.
It is known that treatment with ARBs during the second and third trimesters leads to fetotoxic effects (decreased renal function, oligohydramnios, delayed ossification of the skull), as well as toxicity to the newborn (renal failure, hypotension, hyperkalemia).
In the case of using the drug Lozap® plus in the second or third trimester of pregnancy, an ultrasound scan of the fetal kidneys and skull is recommended.
Children whose mothers took Lozap® plus during pregnancy should be carefully monitored for the development of arterial hypotension.
Due to the lack of information on the use of Lozap® plus during breastfeeding, the use of the drug during this period is contraindicated. During breastfeeding, preference is given to alternative treatment with drugs with a more studied safety profile.
Hydrochlorothiazide. Experience with the use of hydrochlorothiazide during pregnancy, especially during the first trimester, is limited. Animal studies are insufficient. Hydrochlorothiazide penetrates the placental barrier and is detected in the umbilical cord blood. Based on the pharmacological mechanism of action of hydrochlorothiazide, its use during pregnancy may impair fetoplacental blood flow and lead to fetal and neonatal disorders such as jaundice, electrolyte imbalance and thrombocytopenia.
Hydrochlorothiazide is excreted in breast milk. Thiazides can cause intense diuresis and may inhibit milk production. Therefore, the use of Lozap® plus during breastfeeding is contraindicated.