Causes of polyhydramnios
In most cases, the exact cause of the condition is difficult to identify. Polyhydramnios during pregnancy can be caused by several factors.
Maternal reasons:
- heart disease, kidney disease;
- diabetes. The disease causes fetal hyperglycemia and, as a result, polyuria (fetal urine is the main source of amniotic fluid);
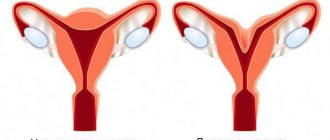
- multiple pregnancy;
- inflammatory diseases of the pelvic organs;
- hemolytic anemia.
Causes of polyhydramnios due to fetal pathologies:
- inability to swallow amniotic fluid due to gastrointestinal malformations (esophageal and duodenal atresia);
- malformations of the central nervous system (hydrocephalus, anencephaly, meningocele);
- tracheoesophageal fistula;
- diaphragmatic hernia, for example, Bochdalek's hernia, in which the pleuro-peritoneal membranes are not developed and the stomach prolapses into the chest cavity. Because of this defect, the fetus is not able to swallow a sufficient amount of amniotic fluid;
- fetal kidney disorders leading to increased urine production, such as in antenatal Bartter's syndrome;
- chromosomal abnormalities such as Down syndrome and Edwards syndrome;
- skeletal dysplasia (dwarfism);
- sacrococcal teratoma.
Amniotic fluid
The development of the baby in the mother's belly occurs in the amnion, which is also known as the amniotic sac. It contains liquid - amniotic fluid. Their quantity and quality are of great importance. Functions of water:
- nutrition
The amniotic fluid contains the nutrients the embryo needs. At the beginning of development, the baby absorbs them through the skin.
- temperature support
Amniotic fluid provides a constant temperature around the fetus at 37˚ C.
- pressure support
Water is also needed to prevent the umbilical cord and fetus from being choked. This is done by maintaining a constant level of pressure in the bubble.
- protection against mechanical damage
Amniotic fluid protects against damage to the baby, which can occur, for example, when a pregnant woman is hit in the stomach. Water also protects the unborn child from noise.
- immunoglobulin protection
The waters that surround the fetus contain antibodies. They are needed to protect against infections. The amniotic sac also protects the waters from contamination by various agents.
- freedom of space for the fetus
The fetus can move in the amniotic fluid.
Symptoms of polyhydramnios
Clinical signs:
- abdominal enlargement;
- uterine size advances gestational age;
- shiny skin with stretch marks;
- dyspnea;
- swelling.
Symptoms are more pronounced in acute polyhydramnios: the abdomen quickly enlarges, a nagging pain appears in the lower abdomen and perineum, and shortness of breath increases. Chronic polyhydramnios during pregnancy is not so pronounced, since amniotic fluid accumulates gradually. A pregnant woman may feel well, so hydramnios is often diagnosed during a routine ultrasound. Mobility, abnormal position, and weak heart rhythm (dull heartbeat) of the fetus are noted. Ultrasound helps to identify extensive hypoechoic zones and assess the volume of amniotic fluid. Polyhydramnios during late pregnancy is manifested by a discrepancy between the size of the uterus and the gestational age.
Also, to make a diagnosis, the content of prolactin in the amniotic fluid is determined. With polyhydramnios, its content is reduced (relative to the norm for a certain period of pregnancy).
Treatment and prognosis
Therefore, it is important to identify this disease as early as possible and apply timely measures. Treatment depends on the cause of polyhydramnios: for infection, it can be antibacterial drugs, and for extragenital pathology, treatment of the underlying disease. In any case, a pregnant woman with polyhydramnios should receive increased attention, because she is at risk of developing complications. She is required to undergo additional ultrasound diagnostics; a CTG (cardiotocography) is performed on the baby to monitor his heartbeat and movements. Even with such a diagnosis, you can give birth to a completely healthy child if you follow the doctor’s recommendations and are attentive to your health.
Consequences of polyhydramnios
The prognosis for the fetus is unfavorable. Perinatal mortality is about 50%. The main causes of death are prematurity and developmental defects. The consequences of polyhydramnios for a child are intrauterine hypoxia, umbilical cord strangulation, development of neonatal pneumopathy, malnutrition (underweight), hyperglycemia.
Polyhydramnios significantly increases the risk of complications during childbirth:
- incorrect presentation of the fetus;
- premature contractions;
- premature rupture of membranes;
- umbilical cord prolapse;
- placental abruption.
The risks are usually proportional to the volume of accumulated amniotic fluid. The consequences of polyhydramnios for a woman are hypertension, respiratory failure, postpartum hemorrhage.
Diagnostics
Polyhydramnios is suspected upon examination based on the indicators described above. Be sure to tell your doctor about all the symptoms that bother you. To confirm polyhydramnios, ultrasound diagnostics are done. The amniotic fluid index is calculated. This is the gold standard for diagnosing the pathology in question. The data of this index is measured every day.
Other diagnostic methods:
- vaginal smear to determine microflora
- blood sugar test to look for possible diabetes
- clinical blood and urine tests
- PCR for torch infections
- blood test for antibela in case of negative rhesus in a pregnant woman
- Dopplerometry (monitoring the baby’s condition)
- cardiotocography
When treating a patient in a specialized medical institution, every day they measure her abdominal circumference, listen to the fetal heartbeat and look at its position.
How is polyhydramnios treated?
Treatment of polyhydramnios is carried out when there is a threat of premature birth or acute respiratory failure in a pregnant woman. To eliminate polyhydramnios, multiple amniocentesis is used - a puncture in the amniotic membrane and collection of amniotic fluid. If the condition is caused by fetal polyuria, the pregnant woman is prescribed a short course of indomethacin. If diabetes mellitus is detected in the mother, hypoglycemic therapy is selected to correct blood glucose levels. If an inflammatory disease is suspected, antibacterial drugs are prescribed. If the cause of the pathology has not been established, normalization of the uteroplacental blood flow is carried out. Antiplatelet agents, vitamins, and antispasmodics are usually prescribed. Read more about the treatment of hydramnios on our website Dobrobut.com.
Related services: Consultation with a gynecologist during pregnancy
What are the risks of polyhydramnios for a woman?
In addition to the purely external defects that this disease (stretch marks) can lead to, there are a number of consequences that can seriously complicate the life of the expectant mother:
- Threat of miscarriage or premature birth. Since there is a lot of water, they put pressure on the internal os of the cervix, the membranes are inflamed and swollen, and a slight load can trigger the process of childbirth or spontaneous miscarriage.
- Malposition. With a sudden release of a large amount of amniotic fluid, the fetus may change its position to oblique or transverse, in which natural childbirth is impossible.
- Bleeding during childbirth and the postpartum period.
- Weakness of labor due to overstretching of the uterine walls.
- With premature rupture of amniotic fluid, umbilical cord loops may fall out.
All this leads to special tactics during childbirth. If this is a premature birth, then this is a special management of the process and the creation of conditions for a premature baby. And, for example, if the fetus is not positioned correctly or if the umbilical cord loops fall out, a caesarean section is definitely necessary.
Pathogenesis
The main role in the development of polyhydramnios is played by the placenta and fetal membranes. With this pathology, involutive changes in the placenta and amnion are detected. In the fetal membranes, the number of microvilli and their increased branching increases, which is accompanied by an increase in the thickness of the embryonic membrane. With this pathology, on the one hand, the secreting activity of the amnion , and on the other hand, destructive changes occur in it, which lead to tissue necrosis. Necrosis affects the development of the fetus and causes various developmental pathologies. The chorion veins also undergo changes - they narrow, and sometimes they are completely overgrown in the chorion villi. With polyhydramnios, fluid transport inward increases through the membranes and through expanded intercellular channels in the epithelium. And due to the thickening of the membranes, the reabsorption of water is partially blocked, which helps to increase their quantity.
List of sources
- Sidorenko V.N., Bugrov V.Yu., Kletsky S.K., Sakharov I.V. A modern view on the etiopathogenesis of oligohydramnios and polyhydramnios and ways to solve them for polyhydramnios of an infectious nature/Medical news. - 2022. - No. 4. — P. 53-57.
- Ishchenko A.I., Demenina N.K. // Women's health. - 2014. - No. 6. - pp. 26-28.
- Kulavsky E.V. Features of the course of pregnancy and childbirth with polyhydramnios. Abstract for the academic degree of Candidate of Medical Sciences. Ufa 2004, 26 p.
- Zubkova M.V. Clinical and genetic characteristics of oligohydramnios and polyhydramnios: Abstract of thesis. dis. ...cand. honey. Sci. - M., 2007. - 21 p.
- Pustotina O.A., Bubnova N.I., Ezhova L.S. Clinical and morphological characteristics of the fetoplacental complex in polyhydramnios and oligohydramnios of infectious origin / Obstetrics and Gynecology. - 2007. - No. 3. — P.42-46.
Polyhydramnios during pregnancy: what is dangerous, causes, signs, consequences, treatment
Polyhydramnios is a type of pregnancy pathology. With polyhydramnios, there is an increase in the amount of amniotic fluid. An increase in the volume of amniotic fluid may be associated with diseases, medications, lifestyle, the influence of external factors and other reasons. According to statistics, it occurs in approximately one woman out of 100 pregnant women. Polyhydramnios can develop over several weeks or progress rapidly (over several hours). Treatment tactics and prognosis depend on the nature of the pathology, its form and type.
Women with a history of polyhydramnios require special monitoring during subsequent pregnancies. Despite the fact that the course of different pregnancies in the same woman is different, an increase in the risk of developing pathology in the future cannot be ruled out.
In ICD-10, polyhydramnios is designated by code O40. In the scientific literature, the pathology is called hydramnios or polyhydramnios.
Polyhydramnios during pregnancy causes serious concern among doctors. A woman with suspected polyhydramnios needs a detailed diagnosis. The results of the examination allow us to determine the form and nature of the pathology, as well as choose the safest and most effective method of treatment.
With polyhydramnios during pregnancy, a woman's volume of amniotic fluid (amniotic fluid) increases. Normally, the amount gradually increases with increasing gestational age.
The amniotic fluid index (AFI) is an indicator that determines the amount of amniotic fluid at different stages of pregnancy. It is calculated using ultrasound. To determine the index during the study, the uterine space is divided into 4 parts. The vertical dimension of a large water-containing pocket located between the fetus and the uterine wall is measured. Normally, this parameter should be within the range of 2-8 cm, and with polyhydramnios it exceeds 8 cm. The amniotic fluid index is measured in mm³ or cm³. For example, in the middle of the second trimester, the IAF is 70-200 mm³. By the beginning of the third trimester it is 90-250 mm³, and after 37 weeks it begins to gradually decrease. By the 40th week of pregnancy, the AFI should not exceed 220-240 mm³.
With polyhydramnios during pregnancy, the volume of amniotic fluid exceeds one and a half liters, and sometimes reaches 5 liters or more. Doctors calculate the volume of amniotic fluid using a formula; this requires knowing the gestational age, fetal body weight, and AFI.
Chronic polyhydramnios
Chronic polyhydramnios is a gradual increase in the volume of amniotic fluid. For some time it does not show any signs. The woman may not be aware of the problem. Most often, pathology is detected during the next ultrasound or during a routine visit to the gynecologist and measuring the volume of the abdomen.
Chronic polyhydramnios occurs in women more often than the acute form of the pathology. This nature of the course is more amenable to correction and less likely to cause irreversible consequences. For chronic polyhydramnios, a woman may be prescribed outpatient treatment or inpatient therapy. An expectant mother with chronic polyhydramnios requires more careful monitoring before birth. The delivery technique is selected in accordance with the course of the pathology, the state of health of the mother and fetus, as well as related factors. In most cases, women with chronic polyhydramnios give birth naturally if there are no other obstacles to this.
Acute polyhydramnios
Acute polyhydramnios is a rapid increase in the volume of amniotic fluid. Usually accompanied by pronounced symptoms and a rapid deterioration in the woman’s well-being, as well as suffering of the fetus. The acute form of polyhydramnios is detected more often when a woman urgently seeks medical help - complaints of rapidly developing swelling, high blood pressure, headache and heaviness in the lower abdomen or perineum.
Acute polyhydramnios is less common than the chronic form of the pathology. If an acute form is detected, a woman requires urgent hospitalization. It is important to make a correct diagnosis and begin therapy immediately, since the outcome of the pregnancy depends on this. In difficult cases, when the volume of amniotic fluid reaches critical parameters within a few hours, the woman may require early delivery. Cesarean section is often performed for acute polyhydramnios. With a good response to therapy, prolongation of pregnancy and natural childbirth are possible.
Forms of polyhydramnios during pregnancy
Polyhydramnios during pregnancy can vary greatly from woman to woman. Therefore, you should not rely on the experience of treatment and the course of pregnancy with polyhydramnios from friends and acquaintances. In addition to the nature of polyhydramnios (acute or chronic), the form is of significant importance.
Mild polyhydramnios
Mild polyhydramnios is the initial stage of an increase in the volume of amniotic fluid. With mild polyhydramnios, the woman is prescribed treatment, and the question of the need for emergency delivery is postponed. With mild polyhydramnios, the best pregnancy outcome will be if the chronic form is diagnosed. This means that the volume of amniotic fluid increases gradually and does not exceed one and a half liters. The acute form of moderate polyhydramnios requires urgent treatment, as a result of which the increase in water volume will be stopped or continued.
With mild polyhydramnios during pregnancy, the volume of amniotic fluid fluctuates up to 1500 cm³. Signs of moderate polyhydramnios are usually blurred or absent altogether. The expectant mother may be bothered by slight swelling of the body and heaviness in the lower back or lower abdomen.
Moderate polyhydramnios
Moderate polyhydramnios is a pregnancy pathology in which the amount of amniotic fluid exceeds 3 liters. Typically, moderate polyhydramnios manifests itself with characteristic signs and forces a woman to tell her doctor about her discomfort (increased blood pressure, a feeling of fullness in the perineum, swelling, headaches). Chronic moderate polyhydramnios has more favorable prospects than the acute form of moderate polyhydramnios. In chronic cases, complaints increase gradually, and in acute cases, symptoms appear suddenly, their intensity increases rapidly.
Moderate polyhydramnios requires monitoring of the woman. Usually the expectant mother is hospitalized and undergoes supportive therapy for several days. The further tactics of doctors depend on the results. Often in obstetrics there were cases when, with moderate polyhydramnios, a woman’s well-being remained stable, the increase in water volume was insignificant, and the pregnancy ended in natural birth.
Severe polyhydramnios
Severe polyhydramnios is a serious pathology of pregnancy, in which the volume of amniotic fluid reaches critical levels. The water level in severe forms of polyhydramnios ranges from 3-5 liters. Such meanings cannot remain unnoticed. With severe polyhydramnios, the expectant mother has complaints of high blood pressure, pain in the abdomen and perineum, a large belly, a sudden appearance of stretch marks on the skin, and general swelling of the body.
Severe polyhydramnios during pregnancy requires immediate medical attention. Usually the woman is hospitalized and prescribed drug therapy. If the fetus is suffering or there is a rapid increase in the volume of amniotic fluid, early delivery is indicated, regardless of the gestational age.
Polyhydramnios in the 1st trimester, in the 2nd trimester, in the 3rd trimester
Polyhydramnios during pregnancy does not appear in the first trimester. Usually the pathology develops in the later stages, but it can also occur in the middle of the gestational period.
Moderate and mild polyhydramnios are not as dangerous as severe polyhydramnios. The pathology is especially dangerous in the later stages and in the presence of concomitant diseases, for example, placental insufficiency. With polyhydramnios in late and mid-pregnancy, it is important to assess the condition of the fetus and the health indicators of the pregnant woman. Based on the obtained parameters, the doctor can make the right decision. When prescribing drug therapy, recommendations for lifestyle and nutrition correction, as well as surgical intervention, it is important to assess the expected benefits for the child and the risks for the mother. The longer the gestational age when polyhydramnios is detected, the more favorable the outcome. This pattern is due to the fact that with polyhydramnios, pregnant women always have a high risk of premature birth (in some cases forced). As you know, the longer the gestational age, the higher the chance of giving birth to a child without complications.
Causes of polyhydramnios during pregnancy
Polyhydramnios during pregnancy can be caused by a number of factors. Diseases of internal organs, unhealthy ecology, genital tract infections, and negative external factors can provoke an increase in the volume of amniotic fluid.
Causes of polyhydramnios in pregnant women:
- Rh conflict (occurs when the mother’s blood group is negative and the father’s is “positive”; the risk of conflict increases with each subsequent pregnancy);
- diabetes mellitus in pregnant women (lack of the hormone insulin causes carbohydrate imbalance);
- arterial hypertension (can develop directly during pregnancy or be diagnosed earlier; in the second case, the woman requires prevention of polyhydramnios);
- inflammatory processes of the urinary and reproductive systems;
- some pathologies of the formation and development of the embryo (this is why it is so important to undergo examinations and screenings in a timely manner).
How does polyhydramnios manifest itself in pregnant women?
The intensity of the signs of polyhydramnios directly depends on its nature and form. Chronic polyhydramnios develops gradually, may not appear for a long time and may appear unexpectedly. Acute polyhydramnios can develop within a few hours, is accompanied by severe symptoms and forces a woman to urgently consult a doctor.
General signs of polyhydramnios in pregnant women:
- deterioration in general health, weakness and malaise;
- shortness of breath, feeling of heaviness in the chest;
- swelling of the body, especially the lower extremities and fingers;
- increase in abdominal volume;
- rapid weight gain;
- formation of stretch marks on the hips, abdomen and chest;
- changes in blood pressure, the formation of hypertension;
- tachycardia and interruptions in heart function, the occurrence of extrasystoles;
- anxiety, feeling of fear, panic attacks;
- a feeling of heaviness in the lower back and front of the abdomen;
- discomfort and feeling of fullness in the perineum.
Diagnosis of polyhydramnios
A doctor can suspect polyhydramnios based on the woman’s signs and complaints. In addition, to make a diagnosis, it is necessary to perform a number of studies, the results of which will not only help make the correct diagnosis, but will also determine the form of polyhydramnios:
- measuring the volume of the abdomen and the height of the uterine fundus;
- body weight measurement;
- Ultrasound.
To determine the cause of polyhydramnios in a pregnant woman, it is recommended:
- taking anamnesis;
- blood test for antibodies (indicated for negative Rhesus in the patient);
- load glucose test;
- serological examination, tests for infections;
- tests to detect other clinical diseases (for example, anemia, blood pathologies, diseases of the endocrine system).
If there are indications, additional instrumental, laboratory or hardware manipulations are prescribed.
Treatment of polyhydramnios
Women with polyhydramnios first of all wonder what to do about this problem, whether the pathology is dangerous for the child and whether it can be cured. Doctors do not give a definite answer to these questions, because much depends on the nature of polyhydramnios, the form and causes of the pathology.
Severe and acute polyhydramnios almost always requires early delivery. A caesarean section is usually performed. The prognosis depends on the period at which the pathology was discovered. With severe polyhydramnios, the fetus usually suffers. Oxygen starvation develops, and irreversible processes occur in the nervous system and brain. Timely intervention by doctors and adequate labor management tactics are the best solution.
Moderate and mild chronic polyhydramnios has a more favorable prognosis. The woman is prescribed conservative therapy, in accordance with the causes of the pathology (etiotropic and symptomatic treatment). Antibiotics, immunoglobulins, insulin injections, diuretics, antihypertensives and other medications may be used. The doctor selects the regimen individually. There is no single treatment algorithm for polyhydramnios that is suitable for all pregnant women. Despite the fact that with moderate and mild polyhydramnios without a pronounced increase in water volume, the prognosis is better, the woman still remains at risk of premature birth and complications. Therefore, it is important to strictly follow your doctor’s recommendations.
Reducing the amount of fluid consumed does not affect the course of polyhydramnios. Drinking has nothing to do with amniotic fluid volume. But a doctor can prescribe a diet; a healthy diet especially helps patients with obesity, diabetes, and arterial hypertension.
To improve the condition of the fetus with polyhydramnios, the expectant mother is recommended to take vasodilating agents, antispasmodics, vitamins and minerals. Auxiliary products are relevant if there is no suffering to the fetus and there is no threat to its life.
Why is polyhydramnios dangerous?
The main threat of polyhydramnios is that the pathology has an irreversible effect on the fetus. With prolonged suffering, irreversible changes develop in the functioning of the brain and vital organs.
In addition, polyhydramnios can lead to:
- incorrect position of the fetus, breech presentation;
- anomalies of labor;
- premature placental abruption;
- violation of the integrity of the uterus;
- bleeding;
- oxygen starvation of the embryo;
- delays in fetal development;
- premature birth or late miscarriage;
- loss of individual parts (umbilical cord, arms, legs) during the discharge of amniotic fluid;
- intrauterine infection.
Danger to mother
Polyhydramnios during pregnancy is dangerous for a woman due to complications during childbirth. Often labor begins prematurely. During the outflow of amniotic fluid in the 3rd trimester, loss of parts of the fetus may occur, which is fraught with injury and oxygen starvation. In addition, women with an overly distended uterus may experience bleeding in the first hours after childbirth. After pregnancy with polyhydramnios, the uterus contracts worse, which requires the use of appropriate medications.
Danger to child
Polyhydramnios is dangerous for a child because it can lead to death. Women with rapid development of pathology have a high risk of stillbirth. Therefore, it is so important to detect the problem in a timely manner and take appropriate measures. With polyhydramnios, oxygen starvation develops, the brain and other important organs suffer. A child with polyhydramnios is usually born prematurely and requires intensive care.
In case of moderate polyhydramnios or a chronic course of a mild form of pathology, pregnancy can be maintained until natural delivery. Despite the high risks, there are many cases where women with moderate polyhydramnios in the later stages gave birth to a full-term child naturally.
Features of childbirth with polyhydramnios
If the pathology is mild and there is no fetal suffering, pregnancy continues successfully until labor begins spontaneously. Women with mild to moderate polyhydramnios give birth naturally unless there are other contraindications. It is impossible to predict in advance the consequences of natural childbirth with polyhydramnios. But it is important to know that a woman in labor with such a diagnosis requires constant supervision by medical personnel, from the very beginning of labor and at least 2-3 days after birth.
In case of severe pathology, the woman is given birth ahead of schedule. A caesarean section is usually performed. The condition of the fetus will directly depend on the form and cause of polyhydramnios, as well as how quickly the problem was discovered and measures were taken to eliminate it.
After childbirth, a woman with polyhydramnios is at risk of uterine bleeding, so the use of drugs to contract the uterus is recommended, and natural breastfeeding is encouraged.
Prevention of polyhydramnios during pregnancy
Polyhydramnios occurs in approximately 1% of women. However, such a low risk is not a reason to refuse prophylaxis. There is no specific scheme to prevent the development of polyhydramnios. To avoid problems, doctors give the following recommendations:
- take a responsible approach to pregnancy planning, exclude infections and diseases;
- determine in advance the Rh factor and the likelihood of a conflict, and if necessary, use the method of administering immunoglobulin before 30 weeks of pregnancy, as well as in the first 72 hours after birth;
- lead a healthy lifestyle and eat a varied diet;
- avoid stress, anxiety, lack of sleep, have healthy physical activity;
- undergo all examinations, ultrasounds and screenings in a timely manner;
- consult a doctor unscheduled if you have any complaints, do not self-medicate.
Prevention
Prevention of this pregnancy pathology includes:
- Advance preparation for pregnancy (be examined for sexually transmitted diseases and chronic gynecological diseases, and, if necessary, treated before pregnancy).
- Identification of women at risk (recurrently pregnant women who had a history of increased water, Rh-negative blood, diabetes mellitus, chronic infections, inflammatory gynecological diseases, twins in a previous pregnancy, fetal deformities in previous pregnancies).
- Thorough examination (endocrinological, bacteriological, immunological, genetic).
- Collecting a genealogical history (finding out cases of polyhydramnios in the mother, sisters and in previous pregnancies).
- Medical genetic counseling.
- Regular visits to the gynecologist and examination throughout pregnancy for early detection of fetal malformations.
- Timely treatment of pregnancy complications.
Medicines
Photo: yaprelest.ru
For polyhydramnios, the following groups of medications can be prescribed:
- anti-inflammatory drugs - prescribed in the presence of an inflammatory process in a woman’s body. The mechanism of action of the drugs is aimed at suppressing the activity of inflammatory mediators, which can be produced under the influence of various exo- and endogenous damaging factors;
- antibacterial agents - used to treat infectious diseases of bacterial etiology. The choice of a specific drug is made depending on the sensitivity of the pathogen that was the source of the development of the infectious disease. Of course, only those antibacterial agents that do not have a teratogenic effect should be prescribed;
- medicines that help improve microcirculation. Representatives of this group of drugs normalize capillary permeability and also improve metabolic processes in the walls of blood vessels;
- vitamin and mineral complexes, the purpose of which helps to saturate a woman’s body with all the necessary vitamins and minerals, thereby enhancing the body’s protective properties.
Diet
In the second trimester, there is a risk of developing gestational diabetes , which is associated with polyhydramnios. Therefore, a mandatory condition is to limit simple carbohydrates - candies, waffles, sweet pastries, halva, cookies, condensed milk, etc. There is no point in restricting fluid intake, since it does not affect the amount of amniotic fluid.
The consumption of table salt should be limited, which will reduce water retention in the body, therefore internal swelling, swelling of the anterior abdominal wall and legs will be significantly reduced. They recommend a diet excluding canned food, salty, spicy foods, sausages and smoked meats, and extractive dishes. The diet should include protein (meat, fish, cottage cheese), fruits, berries, vegetables, vegetable juices, as well as complex carbohydrates in the form of whole grain bread, whole cereals, bran bread, and legumes.
Complications
Everyone who has been diagnosed with this pathology is interested in the dangers of polyhydramnios for pregnant women. An acute form of pathology, as already noted, can provoke termination of pregnancy. Until the 28th week of gestation, termination is carried out for medical reasons. With polyhydramnios, labor may occur prematurely because the uterus is greatly distended. Complications may include prenatal rupture of water, bleeding in the first two hours after birth and in the afterbirth period.
Polyhydramnios often causes placental abruption to occur too early. In such cases, doctors may resort to abdominal delivery. During the release of amniotic fluid, small parts of the baby or umbilical cord loops may fall out, then surgery will be urgently needed.
With polyhydramnios, the fetus is often too active, which can cause it to become entangled in the umbilical cord or become incorrectly positioned. This may also be the reason for the inability to give birth naturally. There is also a risk of suffocation for the baby. Polyhydramnios causes disruption of blood flow in the uterus and placenta, therefore intrauterine hypoxia (lack of oxygen) is possible, and developmental delays in the child are also likely. With polyhydramnios, pregnant women may develop gestosis, uncontrollable vomiting and a persistent increase in blood pressure.