Thiazide diuretics in the treatment of arterial hypertension
In June 2007, at the European Congress on Hypertension in Milan (Italy), new European guidelines for the treatment of arterial hypertension (HTN) were announced. Particular attention of cardiologists was directed to the place of certain classes of drugs in treatment regimens for hypertension.
6 rational combinations of antihypertensive drugs have been proposed [1]:
- thiazide diuretic + angiotensin-converting enzyme (ACE) inhibitor;
- thiazide diuretic + angiotensin receptor blocker;
- calcium antagonist + ACE inhibitor;
- calcium antagonist + angiotensin receptor blocker;
- calcium antagonist + thiazide diuretic;
- beta blocker + dihydropyridine calcium antagonist.
Based on the above, we can conclude that calcium antagonists (4 times) and thiazide diuretics (3 times) appear most often in combinations.
Thiazide diuretics have long been used as agents for the treatment of hypertension. In the 2007 European guidelines, the target groups for whom diuretics are preferred include elderly patients with systolic hypertension as well as heart failure [1].
However, the use of medium and high doses of thiazide diuretics is currently considered undesirable: for example, hydrochlorothiazide at a dose of 100 mg/day increases the risk of sudden death, and at doses of 50–100 mg/day does not prevent the development of coronary heart disease (CHD). In this regard, the recommended doses of thiazide diuretics are currently 12.5–25 mg/day, which do not always achieve an adequate diuretic and antihypertensive effect [2]. In addition, limiting the doses of thiazide diuretics is also associated with their negative effect on carbohydrate, fat and purine metabolism [3]. Therefore, in the 2007 European recommendations, gout was included as absolute contraindications to the use of thiazide diuretics, and metabolic syndrome and impaired glucose tolerance were included as relative contraindications. In addition, special emphasis is placed on the fact that high doses of diuretics cannot be prescribed to pregnant women due to the possibility of reducing circulating blood volume (CBV) and deteriorating blood supply to the fetus. However, we should not forget that diuretics can delay the development of chronic heart failure in patients with hypertension (Davis BR, 2006).
Thus, it is obvious that the scope of application of thiazide diuretics in the treatment of hypertension is quite limited. In this regard, the thiazide-like diuretic indapamide is of particular interest.
Indapamide has a dual effect, due to which it has a short-term and long-term antihypertensive effect. The short-term effect is associated with the effect of the drug on the proximal part of the distal tubules of the nephron and represents a natriuretic effect characteristic of representatives of the diuretic class as a whole. As for the long-term antihypertensive effect, it is unique to indapamide and occurs due to a direct vasodilating effect on the smooth muscle cells of the vascular wall [4].
The antihypertensive effect of indapamide retard 1.5 mg was compared with amlodipine (5 mg/day) and hydrochlorothiazide (25 mg/day) in a study of 605 patients with hypertension treated with the above drugs for 3 months. The number of patients responding to monotherapy was slightly higher in the indapamide-retard group (75.3%) compared with the amlodipine (66.9%) and hydrochlorothiazide (67.3%) groups. In the subgroup of patients with isolated systolic hypertension, a similar trend was observed: the number of respondents in the indapamide-retard group was 84.2%, while in the amlodipine group - 80%, hydrochlorothiazide - 71.4% [5].
The multicenter LIVE (Left ventricle hypertrophy: Indapamide Versus Enalapril) study examined the effect of indapamide and enalapril therapy on regression of left ventricular myocardial mass (LVMM). 505 patients (255 - indapamide group; 250 - enalapril group) with mild and moderate hypertension were prescribed indapamide retard 1.5 mg/day or enalapril at a dose of 20 mg once a day for 1 year. Therapy with indapamide led to a significant decrease in LVMM (p < 0.001); similar results were not obtained in the enalapril group. Indapamide also reduced the severity of left ventricular hypertrophy (LVH) to a greater extent than enalapril (p < 0.049) [6, 7].
Thiazide diuretics have been prescribed in combination with ACE inhibitors for a very long time: many pharmaceutical companies have even developed fixed combinations of these components. In a large number of studies, the combination of indapamide with perindopril also showed good results. However, there are not many studies on the effectiveness of combinations of indapamide with other classes of the drug.
In this regard, we found the work of Hashimoto J. et al interesting. [8], who added indapamide at a dose of 1 mg to 76 patients receiving ACE inhibitors, angiotensin receptor blockers, and calcium antagonists as monotherapy, but failed to achieve target blood pressure (BP) values with this treatment. During 4 weeks of combination therapy in these three groups, the dynamics of the level of 24-hour blood pressure monitoring, home blood pressure measurements, and random blood pressure measurements were assessed. In all groups, a significant decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) was noted. The decrease in SBP in the evening and pulse blood pressure was significantly more pronounced in the angiotensin receptor blocker + indapamide group compared to the calcium antagonist + indapamide group. Thus, the addition of indapamide to antihypertensive therapy led to an additional hypotensive effect that lasted 24 hours.
Until recently, only three classes of drugs were thought to have nephroprotective effects: ACE inhibitors, angiotensin receptor blockers, and calcium antagonists (mainly phenylalkylamines). The nephroprotective effect of thiazide-like diuretics was demonstrated in the NESTOR study [9]. In 570 patients with hypertension and type 2 diabetes mellitus, a comparative study of the effect of indapamide retard 1.5 mg and enalapril 10 mg on the severity of microalbuminuria (MAU) was carried out during one-year therapy. There was a decrease in MAU by 37% in the enalapril group and by 45% in the indapamide-retard group. Thus, the nephroprotective effect of indapamide retard 1.5 mg turned out to be comparable and even slightly higher than that of enalapril.
Another study examined the effect of indapamide retard at a dose of 1.5 mg prescribed for 3 months, compared with placebo, on 24-hour blood pressure monitoring, carbohydrate and lipid metabolism in patients with type 2 diabetes mellitus [10]. A significant decrease in average daily blood pressure was detected in the indapamide group compared to placebo. In addition, there was no effect of the therapy on electrolytes, creatinine, lipid spectrum, uric acid, liver transaminases, insulin levels, glycosylated hemoglobin and glucose tolerance test results.
Considering that diuretics have long established themselves as the drug of choice for the treatment of elderly patients, especially those with isolated systolic hypertension (ISAH). The multicenter X-CELLENT study included 1,758 patients with systolic-diastolic hypertension or ISAH, who were then randomized into 4 groups, which received monotherapy with indapamide retard 1.5 mg/day, amlodipine 5 mg/day, candesartan cilexetil 8 mg/day and placebo for 3 months. Compared to the placebo group, a significant decrease in blood pressure was noted in all groups. The advantage of indapamide in patients with ISAH was the virtually no effect of the drug on normal DBP values while reducing SBP; the remaining drugs reduced both SBP and DBP. In addition, in this group of patients, indapamide retard reduced average daily SBP to a greater extent than amlodipine. All three types of therapy were well tolerated [11].
As we indicated above, a dose of hydrochlorothiazide of 12.5–25 mg/day is considered metabolically neutral. In the work of A. A. Semenkin et al. A comparative study of the antihypertensive effectiveness and metabolic effects of indapamide retard (1.5 mg/day) and hydrochlorothiazide (25 mg/day) was conducted. Despite the comparable antihypertensive effect, in the group of patients receiving hydrochlorothiazide, after 3 months there was a significant increase in triglyceride levels by 15.3% (p < 0.05) and glucose by 12.2% (p < 0.05), and also a significant deterioration in endothelium-dependent vasodilation by 17% (p < 0.05) [12].
Of interest is the potential expansion of indications for the use of indapamide, in particular, its use in the treatment of chronic heart failure accompanied by edema syndrome. In one recent study in patients with persistent peripheral edema, indapamide 2 mg was added to furosemide (40–120 mg/day), which resulted in a significantly greater diuretic effect without a significant effect on plasma potassium and creatinine levels [13].
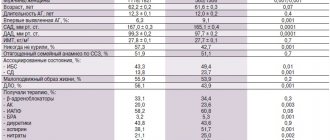
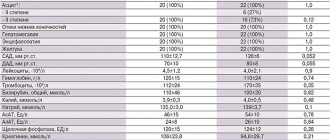
Thus, the original indapamide has more than convincingly proven its antihypertensive effectiveness and organoprotective properties during research. In an attempt to combine low cost with high quality of the drug to provide the majority of patients with hypertension with drugs of adequate action, modern generics of indapamide and, in particular, the drug “Ravel SR”, produced in a dose of 1.5 mg, are of particular interest. The drug has successfully proven itself after a trial in Slovenia in 2005–2006. study [4], which examined its antihypertensive efficacy and tolerability. The drug was prescribed to 1419 patients (58.1% women, mean age 61.9 ± 11.6 years), who showed a decrease in SBP by 14.1% and DBP by 11.1%. The development of adverse events while taking Ravel SR was noted in only 2.5% of patients (the most common were dry mouth and dizziness - 0.42% each, and 1 patient required correction of potassium levels due to the development of hypokalemia without discontinuation of the drug) .
The effectiveness and tolerability of Ravel SR was also studied in domestic studies. S. V. Nedogoda et al. [14] compared therapy with Ravel SR 1.5 mg/day and hydrochlorothiazide 25 mg in patients with hypertension and obesity. Patients of the 1st group received Ravel SR for 6 months, patients of the 2nd group were prescribed hydrochlorothiazide at a dose of 25 mg/day for the first 3 months, and then they were transferred to Ravel SR (3 months). The results of the study showed that while taking Ravel SR, achieving target blood pressure values occurred 15% more often than with hydrochlorothiazide. It was noted that only on therapy with Ravel SR there was an improvement in vascular elasticity (as assessed by pulse wave velocity) and a decrease in myocardial hypertrophy, as well as an improvement in carbohydrate and lipid metabolism.
Also of interest are the results of the BOLERO program (Basic treatment and antihypertensive effect: the drug “Ravel SR” in patients with arterial hypertension), aimed at studying the antihypertensive effectiveness of the slow-release form of the drug and its effect on quality of life. It was shown that the use of indapamide retard for 2 months led to a decrease in SBP and DBP in men by 18%, and in women by 15%. During treatment, cardiovascular risk decreased to the same extent in men and women, and the improvement in quality of life was more noticeable in the group of women [15].
The emergence of each new high-quality and safe generic drug is a step towards ensuring that Russian patients demonstrate higher adherence to hypertension treatment. Currently, patients with hypertension in the Russian Federation who have a target blood pressure level do not exceed 5–15% of the population, while in Western Europe there are more than 30% of such patients. The drug "Ravel SR" (indapamide retard) 1.5 mg as an antihypertensive drug with a mild diuretic effect has every opportunity to expand the boundaries of the use of diuretics outlined by modern recommendations for the treatment of hypertension.
For questions regarding literature, please contact the editor.
D. A. Napalkov , Candidate of Medical Sciences MMA named after. I. M. Sechenova , Moscow
Thiazide diuretics[edit | edit code]
Hydrochlorothiazide
(dichlorothiazide, hypothiazide, nephrix); chemical structure of 6-chloro-7-sulfamoyl-3,4-dihydro-2H-1,2,4-benzothiadiazine-1,1-dioxide. Like Diacarb, the drug contains a sulfonamide group.
Pharmacokinetics
. This thiazide diuretic is well absorbed from the intestine. It appears in the blood within 10 minutes. The maximum concentration after a single dose is 45-60 minutes, the duration of action is 4-6 hours. The half-life is 5.6-14.8 hours, depending on the dose. It is excreted by the kidneys by secretion in the proximal tubules similar to uric acid and, as a result of competition, inhibits its release from the body.
Cyclomethiazide
(cyclopenthiazide, Navidrex); chemical structure of 2-cyclopentylmethyl-6-chloro-7-sulfamoyl-3,4-dihydro-1,2,4-benzothi-adiazine-1,1-dioxide. As the name implies, cyclomethiazide is close in structure to hydrochlorothiazide, differing only in that one of the hydrogen atoms at the C3 position is replaced by a methylcyclopentyl radical.
Pharmacokinetics
. Well absorbed in the alimentary canal. The diuretic effect of this thiazide diuretic occurs after 2-4 hours, maximum after 3-6 hours and lasts 10-12 hours. It is excreted by the kidneys by secretion in the tubules.
Pharmacodynamics of thiazides
. The diuretic effect of thiazide diuretics is carried out, in contrast to diacarb, due to not only partial binding of carbonic anhydrase, but also inhibition of the activity of Na+,K-ATPase, succinate dehydrogenase, and enzymes for the oxidation of non-esterified fatty acids. The supply of energy to the sodium pump is disrupted and Na+ reabsorption is reduced, which contributes to an increase in natriuresis and diuresis. At the same time, the release of potassium, chlorides, hydrogen carbonates, magnesium ions, and phosphates increases. Thiazides in normal doses do not significantly disturb the acid-base balance. With prolonged administration, the drugs delay the excretion of calcium ions.
Cyclomethiazide is much more active than hydrochlorothiazide, is slowly eliminated by the kidneys and therefore has a longer effect.
Thiazide diuretics have an antihypertensive effect. The mechanism of action is that they reduce blood volume. The sodium and water content in the vascular wall also decreases, which leads to its thinning and an increase in the lumen of the vessels. The sensitivity of vascular adrenergic receptors to catecholamines decreases, which also contributes to vasodilation. With prolonged administration, thiazides reduce the excretion of uric acid.
In diabetes insipidus, thiazide diuretics exhibit a paradoxical effect - they significantly reduce diuresis. The mechanism of this action has not been precisely established; it is assumed that there is a decrease in thirst, an increase in the filtration capacity of the kidneys, and the sensitivity of vasopressin receptors to vasopressin in diabetes insipidus.
Side effects:
Thiazide diuretics cause hypokalemia with long-term use, so potassium intake should be increased; Secreted by the kidneys, according to the principle of competition, thiazides reduce the secretion of other substances, in particular uric acid. Therefore, taking thiazides by patients with gout leads to an exacerbation of the disease. In large doses, thiazides can cause hypochloremic alkalosis. In elderly people, thiazides provoke latent diabetes mellitus, causing hyperglycemia. Hypercholesterolemia and hypertriacyl-glycerolemia are also noted.
Newspaper "News of Medicine and Pharmacy" 21 (301) 2009
Currently, we can talk about three generations of thiazide and thiazide-like diuretics: the first generation, typical representatives of which are hydrochlorothiazide and chlorthalidone; second generation, represented by xipamide; the third generation, which is represented by the regular and retard forms of indapamide.
Thiazide and thiazide-like diuretics act at the level of the distal convoluted tubules of the nephron. The greatest diuretic effect is achieved when relatively low doses of thiazide diuretics are prescribed.
The diuretic and antihypertensive effect of thiazide diuretics is significantly weakened in patients with renal failure (serum creatinine level more than 2.0 mg/dL; glomerular filtration rate less than 30 ml/min). For this reason, thiazide and thiazide-like diuretics are not recommended for the treatment of hypertension in patients with impaired renal function.
Thiazide diuretics (unlike loop and potassium-sparing diuretics) reduce the excretion of calcium ions in the urine. The calcium-sparing effect of thiazide and thiazide-like diuretics makes them especially useful in the treatment of arterial hypertension in patients with concomitant osteoporosis. According to some observations, bone fractures are much less likely to occur in patients with hypertension treated with thiazide diuretics compared to patients receiving other antihypertensive drugs.
Small doses of hydrochlorothiazide and thiazide-like diuretics do not affect carbohydrate, lipid and purine metabolism; in addition, a decrease in calcium excretion during long-term use of these drugs is a positive aspect in the treatment of women suffering from postmenopausal hypertension.
Along with the natriuretic effect, all thiazide diuretics increase the excretion of potassium and magnesium ions and at the same time reduce the excretion of uric acid. Therefore, thiazide diuretics are contraindicated in patients with hypokalemia (potassium level less than 3.5 mmol/l), gout and hyperuricemia (uric acid more than 8.5 mg/dl in men and more than 6.6 mg/dl in women).
Experience with the use of diuretics in long-term therapy of hypertension
In hypertension, the hemodynamic effects of hydrochlorothiazide and chlorthalidone, as well as indapamide, have been most well studied.
There are two phases in changes in hemodynamics in patients with hypertension during treatment with thiazide diuretics.
In the first 4–6 weeks of diuretic therapy, blood pressure decreases mainly due to a decrease in the volume of extracellular fluid by 10–15%. Cardiac output decreases at this time, as hypovolemia leads to a decrease in venous return to the heart. Total peripheral vascular resistance (TPVR) does not change or slightly increases. Body weight decreases at the beginning of diuretic therapy by approximately 1–1.5 kg. Plasma renin activity increases.
The mechanisms of the antihypertensive action of thiazide diuretics are not fully understood. Two different mechanisms of action are hypothesized:
1) antihypertensive effect, directly or indirectly associated with depletion of sodium (chloride) reserves; 2) antihypertensive effect associated with direct or indirect vascular effects of diuretics, independent of natriuresis.
Indapamide, unlike other thiazide and thiazide-like diuretics, has a direct vasodilator effect. When prescribing the drug at a dose of 2.5 mg/day, the total peripheral vascular resistance decreases by 10–18%. Vasodilating effect
indapamide is caused by blockade of calcium channels, stimulation of the synthesis of prostacyclin and prostaglandin E2, which have vasodilating properties and activation of potassium channels.
Thiazide and thiazide-like diuretics are first-line drugs for long-term treatment of patients with uncomplicated hypertension and patients with isolated systolic hypertension. Their location has been determined through numerous placebo-controlled studies.
Numerous controlled studies have shown that these diuretics not only effectively lower blood pressure, but also significantly reduce the risk of stroke in patients with hypertension by an average of 34–51% and congestive heart failure by 42–73%, as well as mortality from cardiovascular causes. by 22–24%.
In elderly patients, diuretics and β-blockers are equally effective in preventing the development of cerebrovascular complications. Diuretics prevent the development of coronary artery disease and reduce mortality from cardiovascular complications in elderly patients with hypertension. This gives grounds to consider diuretics as first-line drugs for the initial treatment of hypertension in elderly patients.
Before prescribing diuretics, it is necessary to determine the content of potassium, uric acid, glucose and creatinine in the blood. If hypokalemia, hyperuricemia, hyperglycemia and azotemia are detected, thiazide diuretics should not be used.
It is recommended to start diuretic therapy with low doses of drugs. The initial dose of hydrochlorothiazide is 12.5-25 mg, chlorthalidone - 12.5-25 mg, indapamide - 1.25-2.5 mg.
If there is no sufficient antihypertensive effect after 2–4 weeks of therapy, the initial doses of diuretics are increased. High doses of thiazide and thiazide-like diuretics should not be used unnecessarily - more than 50 mg of hydrochlorothiazide, more than 25 mg of chlorthalidone and more than 2.5 mg of indapamide per day.
For long-term treatment of patients with hypertension, preference should be given to low doses of diuretics in combination with other antihypertensive drugs. Combinations with β-blockers, ACE inhibitors or AII receptor blockers are recommended.
Use of indapamide in the treatment of patients with hypertension
Among the third generation thiazide diuretics, indapamide stands out first, which in its chemical structure is a chlorobenzamide derivative containing a methylindolinyl group.
At a dose of 2.5 mg/day, which is recommended for the treatment of hypertension, indapamide acts primarily as an arterial vasodilator. The daily volume of urine does not change significantly when treated with indapamide at a dose of 2.5 mg/day, but increases by 20% when the drug is prescribed at a dose of 5 mg/day. Therefore, according to the main mechanism of action, indapamide is a peripheral vasodilator, which, when administered in high doses, can have a diuretic effect.
Indapamide differs from other thiazide and thiazide-like diuretics in that it has minimal effects on potassium and uric acid levels.
When treated with indapamide, the plasma concentration of glucose practically does not change and the sensitivity of peripheral tissues to the action of insulin is not impaired, therefore it is the safest diuretic for the treatment of arterial hypertension in patients with diabetes mellitus.
Unlike other thiazide and thiazide-like diuretics, indapamide has a minimal effect on the levels of total cholesterol and triglycerides and slightly increases the level of high-density lipoprotein cholesterol in the blood (by an average of 5.5 ± 10.9%). The ability of indapamide to increase plasma levels of anti-atherogenic high-density lipoprotein cholesterol is unique among all diuretic drugs.
All these effects distinguish indapamide from other thiazide and thiazide-like diuretics and give reason to consider it the first representative of the third generation of this subclass of diuretics.
The retard form of indapamide, indapamide SR (sustained-release), provides controlled slow release and uniform delivery of the drug into the blood over 24 hours. Thanks to a special technology for retarding a small amount of the drug, a long-term antihypertensive effect is achieved. The T/P (trough-peak ratio) for indapamide retard 1.5 mg is 89% for systolic blood pressure (SBP) and 85% for diastolic blood pressure (DBP), indicating the stability of the antihypertensive effect over a 24-hour dosing interval . In addition, studies using a 32-hour period of ambulatory blood pressure monitoring (ABPM) showed that the T/P index 32 hours after the last dose of indapamide SR was 52% for SBP and 54% for DBP (according to the FDA criterion, T index /P of a single dose antihypertensive drug should be at least 50%).
Due to its improved pharmacokinetic profile, indapamide SR is better tolerated than the conventional dosage form of indapamide. The effectiveness and safety of the drug at a dose of 1.5 mg were studied in several large clinical studies - CTs, which showed the entire therapeutic spectrum of the drug, including the effect on target organs of hypertension in a subgroup of elderly patients.
Contraindications to the use of thiazide diuretics
Contraindications for long-term use of thiazide and thiazide-like diuretics in patients with hypertension are hypokalemia, gout, asymptomatic hyperuricemia, decompensated liver cirrhosis, intolerance to sulfonamide derivatives (diuretics, hypoglycemic and antibacterial drugs). In high doses, thiazide diuretics are contraindicated in diabetes mellitus, especially type 1. Diuretics should be prescribed with great caution to patients with ventricular arrhythmias or receiving cardiac glycosides or lithium salts.
***
Thus, at present, thiazide and thiazide-like diuretics are effective, safe and the most accessible antihypertensive drugs that can be used to treat patients with hypertension, both as monotherapy and in combination with other drugs.
Prepared by Evgeniya Priymak