The use of angiotensin receptor blockers in the treatment of arterial hypertension
What is the advantage of angiotensin receptor blockers over other classes of antihypertensive drugs, in particular over ACE inhibitors? What is the comparative effectiveness of various angiotensin receptor blockers?
Based on a representative sample (1993), it can be stated that the prevalence of arterial hypertension (AH) in Russia is 39.2% among men and 41.1% among women. At the same time, only 58.9% of women and 37.1% of men know about the presence of the disease; 46.7% and 21.6% receive treatment (including effective treatment - 17.5% and 5.7%), respectively (first report experts of the Scientific Society for the Study of Arterial Hypertension, the All-Russian Scientific Society of Cardiologists, the Interdepartmental Council on Cardiovascular Diseases, 2000). The management of patients with hypertension is currently regulated by the recommendations of experts from the World Health Organization (WHO) and the International Society of Arterial Hypertension (ISH) (WHO-SOG recommendations, 1999) and the National Guidelines for the diagnosis and treatment of arterial hypertension developed on this basis (All-Russian Scientific Society of Cardiology, Arterial Hypertension Section, 2001). According to these recommendations, the goal of hypertension treatment is to reduce the overall risk of cardiovascular morbidity and mortality, which involves reducing blood pressure to the target level (less than 140/90 mm Hg), as well as correcting all identified risk factors (for example, adequate treatment of hypercholesterolemia , diabetes mellitus). Since course treatment of hypertension is ineffective (in most cases, hypertension cannot be cured), the patient must receive individually selected antihypertensive therapy constantly.
For long-term treatment of hypertension, β-blockers, diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, calcium antagonists, and α-blockers are currently used. As is known, in the pathogenesis of arterial hypertension, angiotensin II plays a crucial role, causing vasoconstriction, stimulation of aldosterone synthesis and its release, sodium reabsorption in the kidneys, cardiac muscle growth, proliferation of smooth muscle cells of blood vessels, increased peripheral noradrenergic activity and a number of other effects. Therefore, the most promising in the drug correction of hypertension are currently considered to be angiotensin-converting enzyme (ACE) inhibitors, which prevent the transition of angiotensin I to angiotensin II, and angiotensin receptor blockers. Widely used ACE inhibitors, although highly effective, have a number of side effects (including cough, angioedema) due to their effect on the metabolism of bradykinin and substance P [4].
Angiotensin receptor blockers have a number of advantages over ACE inhibitors - they more specifically and effectively suppress the cardiovascular effects of activation of the renin-angiotensin system. Currently, this “youngest” group of antihypertensive drugs (the first of them is losartan, synthesized in 1988) is represented by a number of drugs that differ slightly from each other in their mechanism of action and pharmacokinetic properties.
Based on their chemical structure, they distinguish between biphenyl tetrazole derivatives (losartan, irbesartan, candesartan), non-biphenyl non-tetrazole compounds (eprosartan, telmisartan) and non-heterocyclic compounds (valsartan); depending on the presence of the active metabolite - prodrugs (losartan, candesartan) and active medicinal substances (valsartan, irbesartan, telmisartan, eprosartan); depending on the type of antagonism with angiotensin II - competitive antagonists (losartan, eprosartan) and non-competitive (valsartan, irbesartan, candesartan, telmisartan). The main characteristics of various angiotensin receptor blockers are given in table. 1.
The hypotensive effect of angiotensin receptor blockers is primarily associated with the suppression of the vasoconstrictor effect of angiotensin II, realized through receptors in the walls of blood vessels. In addition, blockade of angiotensin II receptors leads to a decrease in the secretion of aldosterone, a decrease in the reabsorption of sodium and water in the proximal segment of the renal tubules.
Stimulation of type 2 angiotensin receptors may play a certain role in the hypotensive effect when the level of angiotensin II is elevated (due to blockade of type 1 receptors). It is assumed that stimulation of angiotensin II type II receptors can lead to vasodilation and suppression of proliferative processes.
At the same time, electrophysiological studies in animals have shown that angiotensin II, by activating presynaptic angiotensin receptors of noradrenergic neurons of the sympathetic nervous system, increases the release of norepinephrine. When studying the effect of various angiotensin receptor antagonists (valsartan, irbesartan, losartan, eprosartan) on the sympathetic release stimulated in decerebrate normotensive rats by spinal cord irritation, an inhibitory effect was noted only for eprosartan [6]. Thus, in clinical practice, eprosartan (teveten) is the only drug in its group that can block both presynaptic receptors and angiotensin receptors in blood vessels in therapeutic doses.
Angiotensin receptor blockers, used in therapeutic doses, on average reduce systolic blood pressure by 10-20 mmHg. Art. and diastolic - by 10-15 mm Hg. Art., as shown in a large number of studies. The maximum reduction in blood pressure is achieved in most patients after 3-4 weeks of treatment.
As an example, here are several clinical studies on the effectiveness of eprosartan. An 8-week, double-blind, placebo-controlled, randomized, clinical (243 patients with mild to moderate hypertension) study of eprosartan (teveten at a dose of 600 mg once daily) showed that the drug lowered blood pressure significantly more effectively than placebo [3 ]: in the eprosartan group, systolic blood pressure decreased by 6 mmHg. Art., diastolic - by 7.5 mm Hg. Art.; the difference compared to the results in the placebo group was statistically significant. Therapy was considered effective if diastolic pressure in the sitting position decreased to 90 mmHg. Art. or the decrease in diastolic blood pressure from the initial level was 10 mm Hg. Art. and more. In the eprosartan group, therapy was effective in 42% of patients, in the placebo group - in 21%.
The relationship between the dose of eprosartan and the level of blood pressure reduction was assessed in a multicenter, double-blind, parallel, placebo-controlled study that included 364 patients with a baseline diastolic blood pressure of 95-114 mm Hg. Art. The effectiveness of eprosartan therapy was assessed at doses of 400, 600, 800, 1200 mg once a day compared with placebo; the duration of treatment was 8 weeks. According to the results obtained, the optimal initial dose of the drug was 600 mg per day [10].
In a 13-week, double-blind, placebo-controlled, parallel-group study [4], 243 patients received eprosartan at a daily dose of 400–800 mg once or twice daily. The dose of the drug was adjusted during the first 9 weeks until the optimal hypotensive effect was achieved, after which drug therapy at an effective dose continued for another 4 weeks. The hypotensive effect of eprosartan was once again confirmed (diastolic blood pressure decreased in the treatment group by an average of 9 mm Hg versus 4 mm Hg in the placebo group), and the therapeutic effect was the same when taking the drug once or twice a day. Therapy with eprosartan (once daily) was effective in 46.8% of cases.
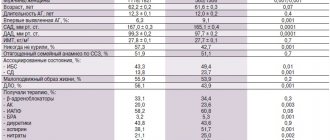
A number of studies have shown that angiotensin receptor blockers are at least as effective as ACE inhibitors (Table 2). For example, in a 26-week, double-blind, clinical (528 patients aged 21-78 years with mild to moderate hypertension) study [2], therapy with eprosartan at a dose of 400-600 mg per day was more effective than treatment with enalapril in dose 5-20 mg per day. There were more patients in whom antihypertensive therapy was found to be effective in the eprosartan group (81.7%) compared to the enalapril group (73.4%). When analyzing the results obtained, it turned out that in the subgroup of elderly patients, the frequency of cases of “response to treatment” was the same as in young patients [1]. Similar results were obtained in another study devoted to a comparative assessment of the hypotensive effects of eprosartan and enalapril in mild to moderate arterial hypertension [7].
The comparative effectiveness of eprosartan (400-800 mg per day in two divided doses) and enalapril (10-40 mg per day in one dose) in severe arterial hypertension was studied in a 10-week double-blind study involving 118 patients (78% of them in over 65 years of age) [8]. The dose was titrated every two weeks; If necessary, hydrochlorothiazide (hypothiazide 25 mg per day) was added to therapy. Therapy with eprosartan led to a more significant reduction in systolic and diastolic blood pressure compared with enalapril; additional prescription of diuretics was required in both groups in almost the same number of patients (39% of patients in the eprosartan group, 37% in the enalapril group). Thus, compared with enalapril, eprosartan is more effective in reducing elevated systolic blood pressure in severe arterial hypertension.
A number of studies have assessed the effectiveness of various angiotensin receptor blockers. For example, an 8-week study [5] included 567 patients with mild to moderate hypertension (Table 3). Therapy with irbesartan at a dose of 300 mg per day was slightly more effective than treatment with losartan at a dose of 100 mg per day; the proportion of patients who responded to treatment was 52% and 42%, respectively. In a 4-week, double-blind, randomized, clinical trial involving 60 patients, eprosartan (600 mg once daily) was found to be more effective than losartan (50 mg once daily). Patients in whom therapy was considered effective were 73% in the eprosartan group and 53% in the losartan group [9].
The most important requirement for modern antihypertensive drugs is a high duration of exposure, allowing control of blood pressure for 24 hours. To assess the severity and duration of the antihypertensive effect of long-acting drugs, the US Food and Drug Administration (FDA) proposed in 1988-1990 . use the “trough:peak” (T/P) coefficient, that is, the ratio between the smallest decrease in systolic or diastolic pressure at the end of the interdose interval and its maximum decrease at the height of the drug’s effect. Antihypertensive therapy seems optimal, in which there are no significant fluctuations in blood pressure during the day, that is, this coefficient should tend to unity, or 100%. According to FDA recommendations, the final:peak ratio should be at least 50%; this means that modern antihypertensive drugs should provide a reduction in blood pressure 24 hours after administration by at least 50% of the reduction in values during the period of maximum hypotensive effect. This allows for effective blood pressure control between doses of the drug; low fluctuations in blood pressure help reduce damage to the vascular wall, and consequently, the frequency of cardiovascular complications of arterial hypertension decreases.
The T/P ratio values for various angiotensin receptor blockers are presented in table. 4.
Using ambulatory blood pressure monitoring, it has been shown that a single dose of angiotensin receptor blockers provides control of blood pressure levels throughout the day, including in the morning, when the risk of developing vascular accidents (myocardial infarction and stroke) is especially high; Only losartan in some cases has to be used twice a day. The highest values of the T/P ratio (i.e., the longest duration of effective antihypertensive action) were found when using eprosartan, irbesartan and candesartan.
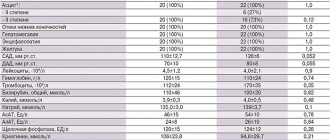
The high effectiveness of angiotensin receptor blockers is combined with good tolerability. According to data obtained from placebo-controlled clinical trials, the frequency of side effects during therapy with drugs of this group does not differ from this indicator in the placebo group. In particular, the incidence of side effects during therapy with losartan is 15.3% versus 15.5% in the placebo group, and during therapy with valsartan - 15.7% versus 14.5%; the frequency of side effects during therapy with eprosartan is given in table. 5. It is very important that drugs in this group, unlike ACE inhibitors, do not cause or worsen cough. Thus, angiotensin receptor blockers are quite safe; Contraindications to their use are only pregnancy, hyperkalemia and bilateral renal artery stenosis.
According to the National Guidelines for the Diagnosis and Treatment of Arterial Hypertension (2001), the absolute indication for the use of angiotensin receptor blockers is intolerance to ACE inhibitors (cough when using them), and the relative indication is congestive heart failure. The last recommendation is due to the fact that, as shown by Pitt B. et al. (1997), losartan can increase life expectancy in patients with chronic heart failure.
It should be noted, however, that inhibition of both the sympathoadrenal and angiotensin-aldosterone systems by eprosartan leads to a significant decrease in systolic blood pressure, therefore the use of this drug is promising for isolated systolic hypertension, arterial hypertension after a stroke, obesity, stress-induced, metabolic, alcoholic hypertension ( Kobalava Zh. D., Moiseev V. S., 2000).
Literature
- Argenziano L., Trimarco B. Effect of eprosartan and enalapril in the treatment of elderly hypertensive patients: subgroup analysis of a 26-week, double-blind, multicentre study. Eprosartan Multinational Study Group. Curr Med Res Opin 1999; 15(1):9-14.
- Gavras I., Gavras H. Effects of eprosartan versus enalapril in hypertensive patients on the renin-angiotensin-aldosterone system and safety parameters: results from a 26-week, double-blind, multicentre study. Eprosartan Multinational Study Group. Curr Med Res Opin 1999; 15(1):15-24.
- Gradman A.H., Gray J., Maggiacomo F., Punzi H., White WB Assessment of once-daily eprosartan, an angiotensin II antagonist, in patients with systemic hypertension. Eprosartan Study Group. Clin Ther, 1999; 21(3):442-453.
- Hedner T., Himmelmann A., for the Eprosartan Multinational Study Group. The efficacy and tolerance of once and twice daily doses of eprosartan in essential hypertension. J Hypertens, 1999; 17:129-136.
- Kassler-Taub K., Littlejohn T., Elliot W. et al., for the Irbesartan Study Investigators. Comparative efficacy of two angiotensin II receptor antagonists, irbesartan and losartan, in mild to moderate hypertension. Am J Hypertens. 1998; 11:445-53.
- Ohlstein EH, Brooks DP, Feuerstein GZ, Ruffolo RR Inhibition of sympathetic outflow by the angiotensin II receptor antagonist, eprosartan, but not by losartan, valsartan or irbesartan: relationship to differences in prejunctional angiotensin II receptor blockade. Pharmacology, 1997; 55(5):244-51.
- Oparil S. Eprosartan versus enalapril in hypertensive patients with angiotensin-converting enzyme inhibitor cough. Curr Ther Res, 1999; 60(1):1-14.
- Ponticelli C., for the Eprosartan Study Group. Comparison of the efficacy of eprosartan and enalapril in patients with severe hypertension. Am J Hypertens, 1997; 10:128A.
- Puig JG, Mateos F., Buno A., Ortega R., Rodriguez F., Dal-Re. R. Effect of eprosartan and losartan on uric acid metabolism in patients with essential hypertension. J Hypertens, 1999; 17(7):1033-1039.
- Weber M. Clinical efficacy of eprosartan. Pharmacotherapy. 1999; 19(4, part 2):95–101.
- Zanchetti A., Omboni S., Di Biago C. Candesartan cilexetil and enalapril are of equivalent efficacy in patients with mild to moderate hypertension. J Hum Hypertens 1997; 11 (suppl 2):57-9.
RAAS blockers and COVID-19
The renin-angiotensin-aldosterone system (RAAS) is an elegant cascade of vasoactive peptides that orchestrates key physiological processes in the human body. The severe acute respiratory syndrome coronaviruses SARS-CoV-1 and SARS-CoV-2 caused the severe acute respiratory syndrome epidemic in 2002–2004 and the current coronavirus disease (COVID-19) pandemic. These viruses interact with the RAAS through angiotensin-converting enzyme 2 (ACE2), a protein whose physiological function is to inhibit the activation of the RAAS, but which also serves as a receptor for both types of SARS viruses. This association between the SARS viruses and ACE2 has been implicated as a potential contributor to infectivity, and there have been concerns regarding the use of RAAS inhibitors that alter ACE2 activity and the impact of differences in ACE2 expression on viral virulence in the current COVID-19 pandemic. Indeed, some media and health systems have recently called for the withdrawal of ACE inhibitors and angiotensin receptor antagonists (ARAs) both prophylactically and in the context of suspected COVID-19.
Given the widespread use of ACE inhibitors and ARBs worldwide, there is an urgent need for recommendations on the use of these drugs in the treatment of patients with COVID-19. Here we emphasize that the data collected from human samples are very scarce and cannot be used to confirm or refute the hypotheses and concerns expressed. In particular, we discuss the uncertain effects of RAAS blockers on ACE2 levels and activity in humans and propose the alternative hypothesis that changes in ACE2 may be beneficial rather than harmful in patients with lung lesions. We also express clear concerns regarding the discontinuation of RAAS inhibitors, as we believe that this may be dangerous for some high-risk patients with known or suspected COVID-19.
Early reports highlighted the potentially high incidence of hypertension among patients with COVID-19 compared with the general population. In the largest case series from China collected during the pandemic, hypertension was the most common comorbidity in 1099 patients, accounting for approximately 15% of the sample, but these values appear to be lower than the incidence of hypertension in patients with other viral infections and lower than the incidence of hypertension in the Chinese population.
According to reports, comorbidities, including hypertension, were much more common in patients with severe COVID-19 requiring transfer to intensive care units and ventilators, or in patients who died, compared with patients with milder disease. Concerns have been raised that therapy for concomitant pathologies, including the use of RAAS inhibitors, could contribute to the outcome of the underlying disease. However, these outcomes were also observed to be closely associated with older age, which is currently considered the most significant predictor of COVID-19-associated death. Unfortunately, reports to date have not paid enough attention to age or other important factors that may act as potential predictors of risk. For other infectious diseases, comorbidities such as hypertension are key prognostic factors, which is likely to be true for COVID-19.
It is important to note that, despite the conclusions about the use of RAAS inhibitors, these studies lack specific data. According to population-based studies, the proportion of the total number of hypertension patients in China receiving antihypertensive therapy is only 30 to 40%. Only 25–30% of patients undergoing treatment receive RAAS inhibitors as basic therapy or as part of combination therapy. The data presented allow us to estimate that only a small proportion of patients with COVID-19 received therapy with RAAS inhibitors, at least in China. It is necessary to obtain information on the relationship between RAAS inhibitor therapy and the corresponding outcomes of the underlying disease, with strict consideration of the indications for therapy and the severity of concomitant disease in patients with COVID-19.
The tissue-specific and systemic components of the RAAS constitute a complex intertwined network of activating and inhibitory peptides (Fig. 1). ACE2 is a critical inhibitory protein responsible for the breakdown of angiotensin II to angiotensin-(1–7), which thereby reduces its effects on vasoconstriction, sodium retention, and fibrosis. Although angiotensin II is the main substrate of ACE2, this enzyme can also convert angiotensin I to angiotensin-(1–9) and participate in the hydrolysis of other peptides. Human studies showed extensive expression of ACE2 in tissue samples obtained from 15 organs, including the heart and kidneys, as well as in the main target cells of SARS-CoV-2 (with manifest signs of damage) - the alveolar epithelium of the lungs. Of particular interest is the low level of soluble forms of ACE2 in the systemic circulation, together with the relatively low functional role of ACE2 in lung tissue under normal conditions. However, there are clinical conditions that promote activation of this link.
Figure 1 | Interaction between SARS-CoV-2 and the renin-angiotensin-aldosterone system
The process of penetration of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) into type II pneumocytes after binding to its functional receptor angiotensin-converting enzyme 2 (ACE2) is shown. After endocytosis of the viral particle, the expression of ACE2 on the surface of the cell membrane is suppressed, leading to the uncontrolled accumulation of angiotensin II. Local activation of the renin-angiotensin-aldosterone system may mediate lung tissue damage during viral infection. ACE is angiotensin-converting enzyme, ARA is an angiotensin receptor antagonist.
It can be expected that ACE inhibitors and ARBs have different effects on ACE2 levels, since their effects on angiotensin II (the main substrate of ACE2) are different. Despite the significant structural homology between ACE and ACE2, their active centers are different. As a result, ACE inhibitors do not directly affect ACE2 activity. Experimental animal models have revealed confounding effects of ACE inhibitors on tissue ACE2 levels and activity. Similar conflicting results in animal model studies have been observed regarding the effect of ARBs on ACE2. Some studies found increased expression of ACE2 messenger RNA or increased concentrations of ACE2 itself, while others found no effect.
In contrast to work in animal models, there are few human studies of the effects of RAAS inhibitors on ACE2 expression. One study described that intravenous administration of ACE inhibitors to patients with coronary insufficiency had no effect on the production of angiotensin-(1–7), which calls into question the effect of ACE inhibitors on ACE2-mediated metabolism of angiotensin II in general. Similarly, in another study among hypertensive patients, angiotensin-(1–7) levels remained unchanged after administration of the ACE inhibitor captopril. However, if captopril monotherapy was continued for 6 months, angiotensin-(1–7) levels increased. In addition, several studies have examined plasma ACE2 activity or urinary ACE2 concentrations in patients on long-term RAAS inhibitor therapy. In cross-sectional studies of patients with heart failure, atrial fibrillation, aortic stenosis and coronary insufficiency taking ACE inhibitors or ARBs, plasma ACE2 activity did not differ from patients with the same diseases not receiving therapy. In a longitudinal cohort study of Japanese patients with hypertension, urinary ACE2 levels in patients receiving long-term treatment with the ARB olmesartan were higher than in untreated controls, but this effect was not observed with the ACE inhibitor enalapril or other ARBs (losartan, candesartan, valsartan, and telmisartan). Previous ACE inhibitor therapy was associated with an increase in ACE2 messenger RNA levels in intestinal tissue, but no association was found between ARB therapy and ACE2 RNA levels; the effect of RAAS inhibitors on ACE2 expression in lung tissue is unknown.
These conflicting data highlight the complexity of RAAS responses to modulators and support the assumption that the conclusions of preclinical studies in model organisms cannot be unambiguously transferred to human physiology. This suggests that the effect of RAAS inhibitors on ACE2 may take different forms depending on the specific drug of the class. It is important to note that plasma ACE2 levels may not be indicative of the full-length membrane-bound form, in part because the process of ACE2 dissociation from the membrane is separately regulated by an endogenous inhibitor. In addition to the degree of expression, the significance of the role of ACE2 may vary depending on the specific tissue or clinical condition. Unfortunately, there is no data on the effect of ACE inhibitors, ARBs and other RAAS inhibitors on the expression of ACE2 in lung tissue. Moreover, even if RAAS inhibitors affect the level and/or activity of ACE2 in target tissues, there is no clinical evidence that this affects the binding and entry of SARS-CoV-2 peplomers into the cell. Further study of the mutual influence of SARS-CoV-2 and the RAAS in humans is necessary.
SARS-CoV-2 not only uses ACE2 to enter the cell, it also inhibits its further expression, which leads to the cessation of its organ-protective effect. It is currently suggested, although without any evidence, that the continuous action of angiotensin II may partially influence the extent of organ damage in COVID-19. Immediately after the reception and attachment of the virus peplomer, the process of a consistent decrease in the concentration of ACE2 on the membrane surface begins. Long-term persistent viral infection and virion replication also contribute to a decrease in ACE2 expression, at least in in vitro cell cultures. Inhibition of ACE2 activity in the lungs causes primary infiltration of neutrophils in response to bacterial endotoxins and can lead to excessive accumulation of angiotensin II released from inhibition and local activation of the RAAS. Indeed, in mouse models, exposure to SARS-CoV-1 peplomers caused acute lung injury that was limited by blockade of the RAAS. In experiments with other mouse models, the authors concluded that ACE2 dysregulation may contribute to secondary acute lung injury following primary infection by virulent strains of influenza virus and human respiratory syncytial virus. A small study correlated elevated plasma angiotensin II levels with total viral load and severity of lung injury in patients with COVID-19. Restoring the level of ACE2 through the administration of a recombinant ACE2 drug made it possible to reverse destructive processes in lung tissue in preclinical models of other acute viral infections, and in phase 2 trials in people with acute respiratory distress syndrome, it was possible to safely reduce the level of angiotensin II.
Dysregulation of ACE2 in COVID-19 could theoretically lead to a decrease in its cardioprotective effect due to myocardial involvement and abnormal pulmonary hemodynamics. Levels of markers of myocardial damage increased during the development of COVID-19 and continued to increase as the disease worsened and before death. Many viruses are cardiotropic, and many viremias are accompanied by subclinical viral myocarditis. The role of ACE2 in the myocardial response to injury and its recovery is well known. Thus, in one study on animals with a knockout of the ACE2 gene, they developed extremely unfavorable processes of left ventricular remodeling in response to acute injury due to the accumulation of angiotensin II. In autopsies of patients who died from SARS, the presence of viral RNA was detected in 35% of cardiac images, which in turn was associated with reduced ACE2 expression. Administration of recombinant ACE2 normalized angiotensin II levels in isolated human hearts affected by dilated cardiomyopathy. These hypotheses formed the basis for testing a recombinant ACE2 drug to restore the balance of the RAAS and potentially prevent organ damage. In addition, paired studies of losartan for the treatment of COVID-19 are currently being conducted in RAAS blocker-naïve patients who have been hospitalized and in patients without a history of hospitalization.
Despite these theoretical controversies regarding the effect of pharmacological regulation of ACE2 on SARS-CoV-2 infectivity, there are clear health risks when discontinuing RAAS blocker therapy in patients who are otherwise in a stable condition. COVID-19 is especially severe in patients with concomitant cardiovascular pathologies, which leads to active myocardial damage, myocardial stress, and cardiomyopathy. RAAS blockers have shown clinical efficacy in protecting the heart and kidneys; their withdrawal may lead to clinical decompensation in patients at high risk.
Although data on heart failure are infrequent in epidemiological reports from China, the incidence of heart failure among critically ill patients in the United States may be high (>40%). Clinical trials of quinapril for the treatment of heart failure demonstrated severe progressive deterioration in patients with chronic symptomatic heart failure. In the TRED-HF study, among patients with asymptomatic heart failure and restored left ventricular ejection fraction, rapid relapse of dilated cardiomyopathy was demonstrated immediately after cessation of therapy (including therapy with RAAS blockers). Moreover, RAAS blockers are the mainstay of therapy after myocardial infarction: continued therapy for several days or weeks after the event has been shown to reduce early mortality. Myocardial infarction associated with COVID-19 may be more dangerous among clinically unstable patients when RAAS blockers are discontinued.
Discontinuation of RAAS blockers prescribed for the control of hypertension may carry fewer risks than their discontinuation for conditions for which they are recommended by many clinical guidelines as a basic therapy, but in this case it may be associated with other difficulties. Discontinuation of RAAS blockers to switch to other antihypertensive therapy in stable outpatients should be done carefully to avoid rebound effects. Moreover, selecting an equivalent dose of other antihypertensive therapy can be problematic in practice and depend on the individual characteristics of each patient. Even small and short-term jumps in blood pressure after a change in therapeutic tactics are associated with excess cardiovascular risk. This may be especially important in patients with COVID-19, an infection that causes activation of the RAAS, in countries where adequate blood pressure control has not been achieved in the population (for example, China).
The effects of discontinuing RAAS blockers or switching to other treatment regimens in patients with chronic kidney disease (CKD) remain uncertain. Although the incidence of CKD in hospitalized patients with COVID-19 is low (1–3%) in China, the incidence of CKD may be higher in other countries and in critically ill patients. Many patients experience varying degrees of acute renal failure during the course of their illness. For these high-risk groups, it is recommended that individual therapeutic decisions regarding RAAS blockers be made based on hemodynamic status, renal function, and clinical stability.
Based on the available data, we believe that despite theoretical concerns and uncertainty regarding the effects of RAAS blockers on ACE2 and the potential impact of these drugs on the course of COVID-19, RAAS blocker therapy should be continued in patients who are stable, at risk of infection, or already ill. COVID-19 (see footnote). This position is now supported by many professional associations (Table S2). Although additional data may influence treatment decisions for high-risk COVID-19 patients, clinicians should be aware of the undesirable consequences of premature discontinuation of proven therapy due to hypothetical concerns based on incomplete experimental data.
- ACE2, an enzyme that physiologically inhibits the activation of the RAAS, is a functional receptor for SARS-CoV-2, the virus responsible for the COVID-19 pandemic
- Some preclinical studies have shown that RAAS blockers may increase ACE2 expression. This has raised concerns about the safety of their use in patients with COVID-19
- There is insufficient data to determine whether these observations can be translated to human physiology, and there is no work examining the effects of RAAS blockers on COVID-19
- Clinical trials are being conducted on the safety and effectiveness of RAAS modulators, including recombinant human ACE2 and the ARA losartan, in the treatment of COVID-19
- Abrupt discontinuation of RAAS blockers in high-risk patients, including those with heart failure or a history of myocardial infarction, may lead to clinical instability and adverse health effects
- Until further data are available, we believe that RAAS blockers should continue to be used in stable patients who may be infected with or already have COVID-19
ANTIHYPERTENSIVE DRUGS AND PHARMACEUTICAL GROUPS FOR INTERACTION
Preferansky Nikolai Georgievich
Head of the Department of Medical and Pharmaceutical Information Systems, NP MIAC RAMS, Prof., Doctor of Pharmacy.
Part IV SARTANS
II.
Angiotensin receptor blockers type I (BAT1)
Depending on the mechanism of binding to angiotensin receptors type I, they are distinguished into reversible competitive (Valsartan, Losartan, Eprosartan) and irreversible non-competitive (Irbesartan, Candesartan) types of action. Reversible drugs have a half-life: Valsartan T½ = 6 hours, Losartan T½ = 2 hours, Eprosartan T½ = 5–9 hours and have a short-term effect. These drugs are bound by a strong covalent bond. Irbesartan T½ = 11–15 hours, Candesartan T½ = 9–13 hours, Telmisartan T½ = 24 hours. They are taken once a day, because they have a long-lasting effect.
Selective non-peptide blockers of type I angiotensin receptors are classified according to their chemical structure into 3 groups:
1. Biphenyl tetrazole derivatives
(biphenyltetrazole derivatives) -
Losartan
(Blocktran, Brozaar, Vasotensin, Zisacor, Cozaar, Lozap, Lorista, Presartan, Renicard);
Valsartan
(Vals, Valsafors, Valsakor, Diovan);
Irbesartan
(Aprovel);
Candesartan
(Atacand).
2. Biphenyl non-tetrazole compounds
(biphenylcarboxylic acid derivatives) -
Telmisartan
(Mikardis, Praytor);
(imidazolecarboxylic acid derivatives) Olmesartan medoxomil
(Cardosal 10, Cardosal 20, Cardosal 40).
3. Non-biphenyl non-tetrazole compounds
(a derivative of tenylimidazole acrylic acid) -
Eprosartan
(Naviten, Teveten).
Table Angiotensin receptor blockers AT1 with other groups
| Interacting group | Result of interaction | Interaction mechanism |
| Alpha blockers | Increased hypotensive effect | Potentiation of antihypertensive effect |
| Antiarrhythmic drug - Propafenone | Life-threatening for patients with ventricular tachyarrhythmias or pulmonary embolism | |
| Indirect anticoagulants | Risk of bleeding | Threat to the life of patients |
| beta blockers | Increased hypotensive effect | Synergy, increased efficiency |
| Herbal diuretics | Increased risk of a sharp decrease in blood pressure | Potentiation |
| Potassium-sparing diuretics | Increased risk of hyperkalemia | Decreased renal excretion of potassium |
| Combined diuretics | Increased risk of a sharp decrease in blood pressure | Potentiation |
| MiME - potassium supplements | Increased risk of hyperkalemia | Synergism regarding blood calcium levels |
| Normothymic drugs (antimanic) | Increased lithium concentration and toxicity | Reducing renal excretion of lithium by inhibiting its secretion |
| Osmotic diuretics | Increased risk of a sharp decrease in blood pressure | Potentiation |
| Loop diuretics | Increased risk of a sharp decrease in blood pressure | Potentiation |
| Various diuretics | Increased risk of a sharp decrease in blood pressure | Potentiation |
| Saluretics, carbonic anhydrase inhibitors | Increased risk of a sharp decrease in blood pressure | Potentiation |
| Sleeping pills | Increased hypotensive effect | Synergism of antihypertensive action due to central sedative action at the level of vasomotor centers |
| Means for inhalation anesthesia | A significant decrease in blood pressure is possible. If possible, discontinuation of ACE inhibitors during upcoming anesthesia | Synergism of antihypertensive action due to blockade of sympathetic ganglia and dilation of blood vessels of the skin and muscles, increasing the tone of the vagus nerve |
| Fluoroquinolones | Sharp decrease in blood pressure | Increased efficiency |
IIa. Interaction of the most studied drugs from the BAT1 group with other groups or active substances
| Drugs that reduce the activity of the RAAS | Interacting groups or active substances | Result of interaction |
| Valsartan | Alcohol | Increased hypotensive effect |
| Warfarin | Prolongation of prothrombin time by 12% | |
| Diuretics | Increased hypotensive effect | |
| NSAIDs | Reduced hypotensive effect | |
| Irbesartan | Diuretics | Increased hypotensive effect |
| Lithium preparations | Increased concentration of lithium in the blood | |
| Losartan | Alcohol | Increased hypotensive effect |
| Hydrochlorothiazide | Synergism, enhanced hypotensive effect. Rational combination | |
| Indomethacin | Weakening the hypotensive effect | |
| Potassium-sparing diuretics, potassium-containing drugs | Hyperkalemia, monitoring serum potassium concentration | |
| Sympathomimetics | Weakening the hypotensive effect | |
| Estrogens | Weakening the hypotensive effect |
IIb.
Interaction of angiotensin receptor blockers AT 1 with active substances
| Active substance | Result of interaction | Interaction mechanism |
| Amiodarone | A sharp decrease in blood pressure | Should not be administered to patients due to inhibition of cytochrome P-450 isoenzymes |
| Ketoconazole | A sharp decrease in blood pressure | Inhibition of cytochrome P-450 isoenzymes |
| Omeprazole | A sharp decrease in blood pressure | Inhibition of cytochrome P-450 isoenzymes |
| Fluconazole | A sharp decrease in blood pressure | Inhibition of cytochrome P-450 isoenzymes |
| Cimetidine | A sharp decrease in blood pressure | Inhibition of cytochrome P-450 isoenzymes |
| Cyclosporine A | With simultaneous use of cyclosporine with angiotensin II receptor antagonists, severe hyperkalemia may develop. |
“Blood pressure pill”: how it works
There is probably no other group of drugs that contains so many drugs. In addition, most of the drugs have a good dozen analogues, which wreaks havoc among antihypertensive drugs, beyond the control of the common mind. But the mind of a good cardiologist and professional pharmacist can comprehend not such a medicinal mess.
"A lot" does not mean "good"
The variety of antihypertensive drugs is largely due to the fact that today, along with modern ones, the drugs that were used to treat our grandmothers continue to be used. Fortunately, they are used quite rarely, but, nevertheless, they bring confusion to the treatment of hypertension. In addition, it should be borne in mind that in Russian pharmacies you can still easily buy any antihypertensive drug without a doctor’s prescription. This means that self-medication of hypertension, which cannot be called anything other than “self-torture,” continues to flourish and bear bitter fruits.
But is there really a big difference in how and with what to reduce the pressure: the main thing is that the tonometer shows the norm or numbers close to it? Of course there is, and here's why.
The fact is that many antihypertensive drugs lead to a sharp decrease in blood pressure. This does not have the best effect on the patient’s well-being, but there are much more serious consequences. If you constantly take these medications, the elasticity of the vascular wall, which regularly tenses and relaxes, decreases. As a result, heart and vascular diseases develop (or rapidly progress) - the most dangerous complications of hypertension.
Drugs that have a sharp vasodilating effect include adelfan and clonidine, beloved by many generations of hypertensive patients. Cheap bendazole and its combination with papaverine, metamizole and phenobarbital (andipal) have a less powerful effect on blood vessels. These drugs reduce cardiac output and, with long-term use, worsen ECG readings.
But herbal antihypertensive drugs, for example raunatin, should not be taken seriously at all: a more effective and safe alternative has long been found for drugs whose age has already exceeded the sixth decade.
Six groups
I have not listed all the antihypertensive drugs that continue to be produced and used, despite serious disadvantages and side effects. There are so many of them that I am afraid to completely confuse the reader. It is much easier to name those drugs that are recognized throughout the world as the drugs of choice for the treatment of hypertension. They belong to six pharmacological groups:
- Diuretics or diuretics (hydrochlorothiazide, indapamide).
- Beta blockers (atenolol, betaxolol, metoprolol, bisoprolol, nebivolol, etc.).
- Calcium channel blockers (verapamil, amlodipine, nifedipine, felodipine, etc.).
- ACE inhibitors (captopril, enalapril, lisinopril, ramipril, fosinopril, etc.).
- Angiotensin II receptor blockers (losartan, valsartan, candesartan, irbesartan, telmisartan, etc.).
- Alpha adrenergic blockers (doxazosin, urapidil, etc.).
The mechanism of action of each of these groups is different and quite complex:
- Diuretics
(diuretics) increase the excretion of salts and water from the body. As a result, the sodium content in the vessel wall is reduced, which prevents vasoconstriction and increased blood pressure. - Beta blockers
work by blocking so-called β1-adrenergic receptors located in the heart. This leads to a decrease in the frequency and strength of heart contractions and a decrease in blood pressure. - The action of calcium channel blockers
is based on the ability to block the passage of calcium ions into the cell, which reduces vascular tone, expands their lumen and improves blood circulation in them. - ACE inhibitors
block the angiotensin-converting enzyme, which converts angiotensin I to angiotensin II, which has a powerful vasoconstrictor effect. - Angiotensin II receptor blockers
act on the same mechanism as ACE inhibitors, but at a later stage. - Alpha blockers
lower blood pressure, reducing vasospasm.
By the way, there is practically no difference in efficiency between them. Among a number of drugs, nifedipine and captopril stand out, which can be taken as first aid to quickly reduce blood pressure. In addition, diuretics, calcium channel blockers and ACE inhibitors definitely reduce the risk of developing cardiovascular accidents, the likelihood of which increases significantly with hypertension.
Angiotensin receptor antagonists
Most doctors will recommend trying an ACE inhibitor first to treat hypertension; if that doesn't work, then they may recommend angiotensin receptor blockers (ARBs).
This group of drugs is better tolerated, they do not cause coughing - which is the most important condition for increasing a person’s adherence to therapy.
Recent discoveries have expanded the use of angiotensin receptor antagonists; they are now not only recommended as initial or adjunctive antihypertensive therapy, but they also show benefits in the treatment of heart failure (HF), diabetic kidney disease, especially among patients with ACE inhibitor intolerance and diabetes.
New indications have emerged, such as chronic heart failure after myocardial infarction, atrial fibrillation and metabolic syndrome. They can be used both in monotherapy and in combination with other antihypertensive drugs.
To date, 9 groups are known. They all have names that end in "sartan". They differ in their ability to reduce blood pressure, duration of action and the presence of additional indications.
The benefits of ARBs do not end there; titrating the dose is easy and simple; you do not have to select as carefully from the group as, for example, calcium antagonists or beta blockers .
Keep in mind that sartans will not have an immediate, sustained hypotensive effect. They work gently, the effect increases gradually, appears at 2–4 weeks and intensifies by the 6–8th week of therapy.
How do angiotensin receptor antagonists work?
The renin-angiotensin-aldosterone system (RAAS) is a coordinated hormonal cascade that controls cardiovascular, renal, and adrenal function by regulating body fluid and electrolyte balance and blood pressure. It is the main active element in the RAAS.
The renin-angiotensin-aldosterone system can be controlled by 4 groups: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), aldosterone antagonists and direct renin inhibitors. Each group only partially suppresses the work of the RAAS. They all act approximately the same way, suppressing the release of the hormone, but they do it in different ways.
ACE inhibitors block the enzyme that promotes its formation, ARBs block receptors , through which its action is realized.
What it does in the body:
- leads to generalized vasoconstriction;
- which increases peripheral resistance;
- increase the load on the heart;
- increases aldosterone, sodium in the blood, resulting in cell growth in the arteries and heart (hypertrophy);
- promotes the release of catecholamines from the adrenal glands, causing hyperactivity of the sympathetic nervous system.
Its inactivation , with the help of ARBs, promotes regression (elimination and reversal) of pathological processes. People with a high renin-sodium profile have a greater risk of myocardial infarction than people with a normal or low profile.
Adverse events from this group include headache, dizziness, hyperkalemia, respiratory infections, angioedema and fatigue. ARBs should not be combined with ACE inhibitors because such combinations increase the risk of hypotension, hyperkalemia, and renal failure.
Losartan
The medicine undergoes transformation in the liver, so the activity of Losartan depends on its condition. The initial dose is 50 mg, the maximum is 150 mg, taken 1-2 times a day.
The effect of Losartan is volume dependent. The maximum reduction in blood pressure should be expected at 4-6 weeks. The medicine has the widest indications: hypertension, heart failure, stroke prevention in cardiac hypertrophy and kidney protection in diabetes (DM).
Pros:
- Treats hypertension, but has a weaker effect on blood pressure than other representatives
- Protects kidneys from diabetes damage
- Reduces the risk of stroke in hypertension better than atenolol
- Eliminates cardiac hypertrophy
- Affects uric acid levels, which other ARBs do not, recommended for gout and hypertension
- Dilates blood vessels
- Excreted approximately 40% in urine and 60% in feces
- Combines well with diuretics
- Has an antiplatelet effect by blocking thromboxane A2 receptors
- Inexpensive
Minuses:
- Cannot be combined with rifampicin, fluconazole
- Increases potassium in the blood
- Has a short period of action, so you need to drink several times a day
- To increase efficiency, you need to constantly increase the amount
- May cause dizziness.
Analogues:
- Losaran (Vertex, Russia) 1000 mg No. 90 – 400 rub.
- Bloktran (Pharm standard, Russia) 50 mg No. 30 - 320 rub.
- Cozaar (Merck) 100 mg No. 28 - 160 rub.
- Lozap (Sanofi) 100 mg No. 90 – 531 rub.
- Losartan (Teva) 50 mg No. 30- 150 rub.
- Lorista (KRKA) 100 mg No. 90- 404 rub.
Losartan has been shown to be highly effective in studies in reducing the risk of death from heart attack or stroke by approximately 13% compared with atenolol, especially in patients with diabetes.
Candesartan cilexetil
Candesartan is a prodrug and therefore requires activation in the liver.
Initial dose - 4-8 mg, average 24 mg, maximum - 32 mg, taken 1-2 times a day. An excellent drug, practically devoid of drawbacks, deserves the attention of hypertensive patients, and is suitable for long-term lifelong use.
Pros:
- Dilates blood vessels
- Protects kidney tissue from damage from high blood pressure and diabetes
- Indicated for the treatment of heart failure
- Significantly reduces the risk of stroke, better than other ARBs
- Well tolerated
- It does not interact with other medications, so it does not interfere with their work.
Minuses:
- May cause dizziness
Analogues:
- Atakand (Astra Zeneca) England - 977 rub.
- Hyposard Polfa 16 mg No. 28- 301 rub.
- Cantab Nobel Türkiye 8 mg No. 28- 250 rub.
- Kandesar Sunn India 8 mg No. 10- 42 rub.
- Kasark (candesartan + hydrochlorothiazide) Evertogen India – 250 rub.
Olmesartan medoxomil
Also a prodrug, it needs to be converted by the liver. Initial amount 20 mg, maximum 40 mg, dose 1 time.
It is in second place in Europe in popularity, sold under the name “Benicar”. Shows the greatest effectiveness among sartans in controlling high blood pressure.
Pros:
- Treats hypertension, for best effect a dose of 40 mg is needed
- Starts working quickly in 1-2 hours
- Good when combined with diuretics
- Recommended for children from 6 years old
- Excreted in feces (60%) and urine (40%)
- Duration of action up to 24 hours
- The maximum antihypertensive effect occurs at week 8, blood pressure results begin at week 2
- Food does not affect absorption
- Well tolerated, the number of side effects was comparable to placebo.
Minuses:
- Hard
- Has a number of heart restrictions
- Recommended only for the treatment of hypertension
- Not possible for congestive heart failure
Analogues:
Cardosal Berlin Chemie (Germany) 10 mg No. 28 - 468 rub.
Azilsartan medoxomil
After activation in the liver, azilsartan is converted into the active form. The initial dose is 40-80 mg, maximum 80 mg. Reception 1 time.
pros:
- Binds more strongly to receptors than other ARBs
- Has a powerful and long-lasting antihypertensive effect
- Increases tissue sensitivity to insulin and affects the mass of adipose tissue, promising for patients with hypertension with metabolic disorders
- Combines well with diuretics
- 2 weeks are enough for stable stabilization of blood pressure
- Reduces anxiety levels
- Lowers sugar levels
- Has nephroprotective properties.
Minuses:
- May cause dizziness, diarrhea
- Recommended from 18 years of age
- Not suitable for severe liver dysfunction
- There are no analogues, dear.
Analogues:
- Edarbi Takeda (Japan) 20 mg No. 28 - 377 rub., 80 mg No. 28 - 830 rub.
- Edarby Clo Takeda (Japan) - Azilsartan 40 mg + chlorthalidone 25 mg No. 98 pcs - 1840 rub.
According to clinical studies, azilsartan in a minimum dose (40 mg) reduces blood pressure better than taking the maximum dose of valsartan and olmesartan.
Eprosartan
They are not a prodrug, so they can be used for liver pathologies. Initial dose - 600 mg, maximum - 800 mg, taken 1 - 2 times a day.
Tops the popularity rating in Europe, recommended only for the treatment of hypertension. Excellent protection against primary and recurrent stroke.
Pros:
- Treats hypertension
- Dilates blood vessels
- Has a mild diuretic effect
- Open 24 hours
- Maximum effect after 2 weeks
- Does not affect heart rate
- Mainly excreted through the intestines (90%)
Minuses:
- Sometimes causes headaches and indigestion
- There are no analogues, only the brand is on sale, expensive
Analogues:
Teveten (Abbot, Netherlands) 600 mg No. 14– 1299 rub.
Patients who took telmisartan, eprosartan, and irbesartan were less likely to refuse to continue treatment than patients who were on losartan.
Irbesartan
It is not a prodrug, it works immediately, without the help of the liver. Irbesartan has one of the highest bioavailability. The initial dose is 150 mg, the maximum is 300, taken 1 time. It differs from analogues in its powerful nephroprotective effect.
Pros:
- Ideal for hypertension and kidney damage due to diabetes
- Shows antiplatelet effect
- Valid for 24 hours
- Exceeds the effectiveness of valsartan
- In lowering diastolic blood pressure it was inferior to olmesartan
- Reduces the incidence of congestive heart failure
- Combines well with diuretics
- Recommended for hypertension and obesity
- Protects kidneys from damage
- Well tolerated
Minuses:
- Possible dizziness
- Increases potassium levels in the blood.
Analogues:
- Aprovel (Sanofi Aventis, France) 150 mg No. 14 - 200 rubles, 300 mg No. 28 - 706 rubles.
- Irbesartan Atoll, Russia 300 mg No. 28 - 559 rub.
- Irbesartan (Canon, Russia) 150 mg No. 28- 391 rub.
Telmisartan
Telmisartan is record to date for an ARB. Provides a hypotensive effect for up to 48 hours.
Sartan of the second generation, is one of the active metabolites of losartan, superior to it in all respects.
The initial dose is 40 mg, the maximum is 80 mg. Reception 1 time. Telmisartan is the drug of choice in patients with obesity and hypertension, especially resistant to therapy.
Pros:
- Not a prodrug, acts immediately
- Duration 48 hours
- Has a rapid onset of action within 30 minutes
- Increases tissue sensitivity to insulin and enhances glucose utilization in muscles and tissues
- In therapeutic dosages it acts as a hypoglycemic agent
- Has a beneficial effect on carbohydrate and fat metabolism
- Suitable for elderly patients
- Has antiplatelet activity.
- Reduces the risk of heart attack and stroke in diabetics.
Minuses:
- Coadministration of telmisartan with digoxin increases plasma digoxin levels, which may lead to toxicity.
Analogues:
- Mikardis (Boehringer Ingelheim) Germany 40 mg No. 14 – 335 rub.
- Telzap Sanofi, France 40 mg No. 90- 703 rub.
- Telmista (KRKA, Slovenia) 40 mg No. 84 – 724 rub.
- Elmisartan SZ (Northern Star, Russia) 40 mg No. 30 - 216 rub.
- Telsartan (Doctor Reddis, India) 40 mg No. 30 - 230 rub.
- Tanidol (Gedeon Richter, Hungary) 40 mg No. 30 – 196 rub..
Valsartan
Valsartan and losartan were first on the market. It is not a prodrug.
The initial dose is 20-40 mg or 160 mg, the average is 254 mg, the maximum is 160 mg. Once a day.
In Europe it is in third place in popularity.
Pros:
- Treats hypertension
- Starts working in 2 hours
- Indicated for chronic heart failure and after a heart attack
- Mortality from cardiovascular diseases decreases with cardiac weakness or after myocardial infarction
- Reduces the risk of blood clots
- Has a vasodilating effect
- Has many analogues on the market
- Does not affect glycemic levels, does not change lipid profile and triglyceride levels.
Minuses:
- Not recommended for severe liver and kidney damage
Analogues:
- Valz (Balkanfarma Bulgaria) 40 mg No. 30 - 124 rub.
- Valsacor (KRKA, Slovenia) 80 mg No. 90 — 682 rub.
- Diovan (Novartis, Switzerland) 80 mg No. 28 – RUB 1,570.
- Valsartan (Atoll, Russia) 80 mg No. 30- 183 rub.
- Exforge Novartis, Switzerland - this is (valsartan / amlodipine) combined - 1228 rubles.
A number of studies have shown that valsartan for hypertension is comparable to amlodipine in the long term.
News: A new effective combination drug for the treatment of heart failure has recently been tested. It contains sartan (valsartan) and a new class of drugs - neprilysin inhibitors (sacubitril).
It's called "Uperio" (sacubitril + valsartan). Uperio showed good results in chronic HF with hypertension.
Fimasartan
Another new ARB inhibitor developed by a Korean company. Obtained by converting the losartan molecule, it is 10 times superior to it and valsartan.
Used only as an antihypertensive agent. The initial dose is 60 mg, the maximum is 120 mg. Take once a day.
Pros:
- Treats hypertension
- Can be used for heart failure
- Acts quickly and for a long time
- Shows antihypertensive effect within 24 hours
- Dilates blood vessels
- It is excreted only in feces.
Minuses:
- The market is represented by one representative, dear.
Analogues:
Kanarb (Boryung, Korea) 6 mg No. 30 - 907 rub., 120 mg No. 30 - 1348 rub.
Key points
Sartans (BRA) are a unique group. If a sick person tolerates it well, his blood pressure has stabilized and remains stable for 24 hours, and he has diabetes and increased weight, then there is no need to look for the best remedy among other groups of drugs. You can stay on it for life, if necessary, just increase the dose and add a diuretic.
After a few years of taking it, we will see positive changes: the size of the heart and the thickness of blood vessels will return to normal, kidney function will be restored, sugar and cholesterol levels will stabilize. In the long term, they will reduce the risk of heart attack and stroke.
They will also prevent a recurrent heart attack, slow the progression of renal failure, and reduce the risk of diabetes in patients at risk.
In addition, angiotensin receptor antagonists are well tolerated and should be considered as first-line agents for the prevention and management of risk factors for CVD and other diseases.
The addition of sartans to ACE inhibitors or aldosterone antagonists is unlikely to be advisable and should be avoided due to the risk of hyperkalemia.
If a person taking an ACE inhibitor or sartan still has symptoms, perhaps adding a calcium antagonist (amlodipine) or a beta blocker (nebivolol) or trying angiotensin/neprilysin (Uperio).
In the Russian ranking according to doctors' recommendations, losartan is in the lead, with valsartan in second place. This is explained by its affordable price and good knowledge. Despite the fact that other representatives of the group are more powerful, have a longer effect, and are used less frequently.
The choice of ARB can be considered ideal if it is recommended taking into account the individual characteristics of the body, tolerance and existing pathology.
How to choose a worthy drug so that it brings maximum benefit for various conditions:
- Hypertension - any sartan can be used. Olmesartan, eprosartan and telmisartan have proven themselves well.
- Prevention of cardiac pathology - telmisartan is better, losartan is also possible
- Heart failure (shortness of breath) - losartan, valsartan, candesartan
- Immediately after a heart attack - valsartan is better, telmisartan is allowed
- Stroke - losartan or telmisartan, candisartan, eprosartan.
- Atrial fibrillation - telmisartan, in second place is candesartan, valsartan and losartan
- Diabetes – telmisartan, valsartan. In second place are losartan, irbisartan and candisartan. Undesirable – olmesartan
- Metabolic syndrome (obesity) – telmisartan, in the background – valsartan
- Gout – losartan, undesirable – candesartan
- For sexual weakness , give preference to valsartan, losartan, irbesartan.
- Cognitive impairment – Candesartan, Irbesartan, Losartan, Valsartan, Eprosartan, Telmisartan.
Only the right approach to choosing a medicine will improve the quality of life, prolong it and reduce the risk of fatal cases.
Rating
The latest 2013 European recommendations for the treatment of arterial hypertension (ESH/ESC Guidelines for the management of arterial hypertension) declare that “... since metabolic syndrome is often regarded as a “prediabetic” condition, preference is given to blockers of the renin-angiotensin system and calcium antagonists, t . To.
they have the potential to improve, or at least not worsen, insulin sensitivity, while beta blockers (except beta blockers with vasodilating properties) and diuretics should be considered as adjunctive agents, preferably used in low doses." The recommendations in the section “Drugs of choice in certain situations” also indicate that angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), and calcium antagonists are the drugs of choice for metabolic syndrome [1].
It is known that ARBs (sartans) suppress the activity of the renin-angiotensin-aldosterone system more completely than ACEIs and do not affect the bradykinin system. In terms of antihypertensive effectiveness, ACEIs and ARBs are equivalent, but the latter have a better tolerability profile, since they do not cause cough or angioedema. ARBs provide higher adherence to therapy among patients with hypertension due to a better tolerability profile and the absence of “escape” of the hypotensive effect.
ARBs have pronounced cardio- and nephroprotective effects: they prevent left ventricular hypertrophy, increase the duration of sinus rhythm retention in paroxysmal atrial fibrillation, reduce the degree of microalbuminuria and proteinuria, and slow the progression of heart and renal failure. With long-term use, ARBs reduce carotid intima-media thickness and the volume of large atherosclerotic plaques (MORE study with telmisartan).
A significant reduction in the risk of developing diabetes mellitus during ARB therapy was also found in the LIVE, VALUE, CHARM, and ALPIN studies.
In the LIFE study, the reduction in the relative risk of developing new cases of diabetes mellitus while taking losartan was 25%, in SCOPE with eprosartan therapy - 20%, and in CHARM with candesartan therapy - 22%. A meta-analysis also showed that ARB therapy is associated with a reduction in the development of new cases of diabetes mellitus [2].
At the same time, a significant reduction in the incidence of cardiovascular complications was noted in the treatment of ARBs in hypertensive patients with diabetes mellitus (LIFE, IDNT, RENAAL).
An important advantage of ARB therapy in light of the metabolic syndrome epidemic is that the number of AT1 receptors and their sensitivity to angiotensin II increases dramatically in obesity, hyperinsulinemia, and dyslipidemia.
An important mechanism of action of ARBs is the modulation of the activity of PPARγ receptors responsible for glucose homeostasis, lipid metabolism and blood pressure regulation. This effect not only reduces blood pressure, but also normalizes levels of glucose, insulin and triglycerides. Moreover, the results of a number of studies indicate a decrease in tissue insulin resistance due to stimulation of nuclear PPARγ receptors in cells of adipose, muscle tissue, and hepatocytes, and this effect is comparable to the effect of oral hypoglycemic drugs.
Thus, there is a compelling case for widespread use of the ARB class in metabolic syndrome. At the same time, the practicing physician faces the problem of differentiated selection of a specific drug for a specific patient. In this regard, it is advisable to consider the clinical and pharmacological characteristics of ARB representatives. Moreover, significant intraclass differences between them find new confirmation [3]. Thus, in a clinical study, two drugs of the ARB group (telmisartan and losartan) were compared, during which it was found that telmisartan, unlike losartan, reduces the concentration of free blood glucose, unbound insulin and HbA1c, thereby identifying the main intraclass differences between the drugs in potential improvement metabolic disorders in patients with metabolic syndrome [4].
Losartan
Over the past decade, numerous and convincing data have emerged on the close relationship between increased uric acid levels and an increased risk of cardiovascular complications in hypertension, metabolic syndrome, and type 2 diabetes. At the same time, a connection has been proven between impaired uric acid metabolism and endothelial dysfunction [5]. According to the PIUMA Study, the presence of hyperuricemia increases the risk of cardiovascular complications by 1.73, and the risk of mortality by 1.96.
The prevalence of hyperuricemia with a combination of arterial hypertension and metabolic syndrome is 37.8%, and in its absence – 22% [6]. However, the duration of the disease does not affect the frequency of hyperuricemia. The study authors showed that patients with uric acid levels above 300 μmol/L have more pronounced metabolic risk factors, which are directly dependent on the degree of increase in uric acid. Losartan blocks the two main transport systems of distal tubular epithelial cells involved in the reabsorption of urates (urate/lactate and urate/chloride) and protects the structures of the renal tubulointerstitium from the damaging effects of urates. When using losartan, the excretory pool of uric acid increases only due to inhibition of urate reabsorption without increasing filtration, which fundamentally distinguishes it from classical uricosuric drugs, the use of which increases urate filtration and increases the risk of developing nephrolithiasis. It has been shown that losartan itself, and not its active metabolite E-3174, has uricosuric activity [7]. Consequently, this activity is due to the characteristics of the molecule, and not to blockade of the AT1 receptor, which is fundamentally important when analyzing the class-specific effects of this group of antihypertensive drugs. The LIFE trial, which assessed the effect of losartan and atenolol on cardiovascular events and mortality among high-risk hypertensive patients with left ventricular hypertrophy, also examined the association of baseline uric acid levels with other risk factors and disease prognosis, and was the first large-scale study to demonstrate that a decrease in uric acid levels during losartan therapy is associated with a positive effect on the incidence of complications in the treatment of arterial hypertension.
Valsartan
The NAVIGATOR study showed that in patients with impaired glucose tolerance and risk factors, treatment with valsartan leads to a relative reduction of 14% and an absolute reduction of 3.8% in the incidence of new cases of diabetes mellitus [8].
A distinctive feature of valsartan is its positive effect on sexual function in men and women [9, 10]. This is due to its ability to have a direct vasodilating effect, improve endothelial function and microcirculation, reduce the volume of connective tissue in the corpora cavernosa, increase testosterone levels in men and indirectly, through metabolites of angiotensin II (angiotensin IV), influence the dopaminergic system involved in the regulation of sexual behavior.
Candesartan
The metabolic effects of long-term antihypertensive therapy with candesartan were studied in the ALPINE study [11]. When compared with hydrochlorothiazide, the candesartan group showed a decrease in insulin levels, blood glucose, triglycerides and an increase in HDL. In the hydrochlorothiazide group, compared with the candesartan group, there was also an increase in the ratios of high- and low-density lipoprotein cholesterol and apolipoprotein B/apolipoprotein AI, which indicates a deterioration in the lipid profile. Against the background of these changes, diabetes mellitus was diagnosed in 4.1% of patients in the hydrochlorothiazide group and only in 0.5% of patients in the candesartan group, and metabolic syndrome was diagnosed in 18 patients in the hydrochlorothiazide group and only in 5 patients in the candesartan group. A distinctive feature of the drug is the presence of an evidence base for effective use in chronic heart failure, including in the subgroup of patients with impaired carbohydrate metabolism.
Irbesartan
The nephroprotective effect and the ability of the drug to reduce albuminuria have been proven in large studies (IRMA, IDNT). But an important feature of irbesartan is its ability to ensure that 70% of patients achieve target blood pressure in metabolic syndrome. At the same time, all of them showed a decrease in waist circumference and a decrease in the initially elevated levels of insulin, glucose and blood lipids. Moreover, it should be noted that it is most pronounced when arterial hypertension and metabolic syndrome are combined [12]. Similar results were obtained in another study [13]. In addition, recent studies have shown that irbesartan and telmisartan act as partial agonists of peroxisome proliferator-activated receptor γ (PPARγ) at concentrations achieved by oral administration and doses recommended as a treatment for hypertension, making their use possible for sensitization. to insulin [14].
Telmisartan
Telmisartan exhibits maximum activity against PPARs compared to other ARBs and has maximum lipophilicity. PPARγ play a key role in the metabolism and energy metabolism of adipose tissue - creating lipid reserves in white adipose tissue and increasing energy expenditure in brown fat. PPARγ is also involved in adipocyte differentiation and regulation of glucose metabolism by improving insulin sensitivity, being a link between lipid and carbohydrate metabolism. The use of telmisartan may prevent the development of atherosclerosis by reducing visceral fat, suppressing vascular inflammation and increasing adiponectin levels, especially in patients with metabolic syndrome.
A recently published meta-analysis of 10 randomized trials involving 546 patients with metabolic syndrome showed that telmisartan significantly reduced fasting glucose, hyperinsulinemia, glycated hemoglobin, increased insulin sensitivity and adiponectin levels [15].
It is important to note that telmisartan also has the same positive effect on all of these indicators, as well as lipids and resistin, during therapy with rosiglitazone [16]. In addition, only telmisartan in combination with rosuvastatin reduces insulin resistance and C-reactive protein levels, in contrast to the combination of this statin with irbesartan and olmesartan [17].
Thus, analysis of the evidence base for the use of ARBs in metabolic syndrome, the features of their clinical pharmacology and experience in practical use make it possible to offer the practitioner a simple algorithm for their differentiated use in this condition (see figure).