What is type 1 diabetes and why is it dangerous?
The content of the article
Juvenile type 1 diabetes (T1DM) is a disease associated with metabolic disorders, namely a deficiency of the hormone insulin and increased concentrations of glucose in the blood. It is an autoimmune disease in which the immune system mistakenly destroys the body's own cells, making it difficult to treat. The disease affects both adults and children. A baby can become insulin dependent after suffering a virus or infection. If we compare statistics on type 1 and type 2 diabetes, type 1 diabetes occurs in approximately one in 10 cases.
Type 1 diabetes is dangerous due to severe complications - it gradually destroys the entire vascular system. For example, T1DM significantly increases the risk of developing cardiovascular diseases: people suffering from hyperglycemia are more likely to suffer strokes and heart attacks. The life expectancy of a woman suffering from type 1 diabetes is 15 years less than that of a healthy woman of the same age. Men with hyperglycemia live on average to 50-60 years and die 15-20 years earlier than their peers.
Diabetics must follow a diet and daily routine throughout their lives, take insulin and monitor their blood sugar levels. If you follow all the recommendations of the endocrinologist, and it is this doctor who treats type 1 and type 2 diabetes mellitus, you can avoid dangerous complications and live a normal life.
Treatment
Treatment of diabetes is all about managing the disease throughout your life. Type 1 diabetes involves constant administration of the missing hormone to the patient - insulin. In addition, adherence to diet, proper distribution of physical activity and self-discipline play an important role in treatment.
Drug treatment: insulin therapy
People with type 1 diabetes need insulin injections every day to control blood sugar levels and get the energy the body needs. The doctor, together with the patient, selects the most effective type and regimen of drug administration.
Entering a fixed dose of insulin
When choosing this regimen, the patient injects himself with a fixed dose of insulin throughout the day. In this case, you need to carefully monitor the amount of carbohydrates consumed and take into account physical activity so as not to cause a state of hyper- or hypoglycemia.
How does an insulin pump work?
“Modern pumps consist of several blocks. The first is glucose monitoring (a sensor (needle) is implanted under the skin, which measures blood sugar levels hundreds of times over a long period of time. The second is a bottle of insulin (short-acting) that enters the human blood. It is necessary to constantly change insulin dosage regimens in depending on physical activity and the amount of planned calorie consumption.”
Morgunov Leonid Yulievich
expert
Head of the endocrinology department of the State Budgetary Institution "City Clinical Hospital named after A.K. Eramishantsev, Moscow Department of Health, endocrinologist
Basal-bolus regimen
This scheme simulates the production of insulin by the pancreas. Following this, the patient injects himself with long-acting basal insulin to maintain blood sugar levels in the absence of food. Before meals, to eliminate sugar surges, a bolus of short-acting insulin is also administered.
Its dose depends on the blood sugar level and the amount of carbohydrates in the dishes consumed. This is a more flexible scheme in terms of power mode. The main thing is to correctly measure how much insulin you need.
Important!
Your attending physician and specialists from the School of Diabetes will teach you how to dose insulin depending on the calorie content of food and physical activity. Check her address at your local clinic. Muscovites can find him out at this link. It is advisable to take classes at such a school annually. You will have to carefully analyze everything you eat, calculate how many units of insulin you need to inject for this, and monitor how the body reacts to the injection.
How to administer insulin
There is no need to be afraid of insulin therapy. For convenient administration of insulin, easy-to-use devices have long been developed: an insulin pump and a “penfill” - a syringe pen with insulin.
Insulin pump
The insulin pump (Fig. 2) independently administers the required amount of insulin throughout the day, imitating the work of the pancreas. In this case, short-acting insulin is used; the insulin bolus program before meals can be adjusted depending on dietary habits.
Figure 2. Insulin pump. Photo: Romaset / Depositphotos
Pump insulin therapy has a number of contraindications, including the presence of a mental illness that can lead to improper use of the device, decreased vision (if this interferes with interaction with the interface), acute somatic (non-mental) diseases or exacerbations of chronic diseases, psycho-emotional stress.
In addition, the use of a pump is not recommended for newly diagnosed type 1 diabetes mellitus, but this is a temporary limitation due to the fact that the patient must first learn to count insulin, and only then proceed to pump therapy.
Pump - there are difficulties
“In 25% of patients, the insulin pump “does not work” because you constantly need to think about how to calculate and how much insulin to administer, use different modes, do not forget about all this, etc. It is generally not recommended for blind patients, because It will be difficult for them to understand this device. Despite the constant improvement of equipment and good reviews about the insulin pump, there are a lot of technical difficulties: the needle gets clogged, the device breaks down, insulin does not flow, etc., which can lead to serious complications.”
Morgunov Leonid Yulievich
expert
Head of the endocrinology department of the State Budgetary Institution "City Clinical Hospital named after A.K. Eramishantsev, Moscow Department of Health, endocrinologist
Penfill
Penfill (Fig. 3) is a syringe pen for administering insulin. The pen allows you to change the insulin dose using a selector.
Figure 3. Penfill. Photo: DGLimages/Depositphotos
Important!
The dose of insulin administered should correspond as closely as possible to the amount of carbohydrates consumed. When using a pen, never inject excess insulin “just in case”! A drop in blood glucose levels (hypoglycemia) occurs very quickly and you may lose consciousness.
Sugar control
Since the dose of insulin depends on the level of sugar in the blood, it must be constantly measured using a glucometer (Fig. 4).
Figure 4. Glucometer for measuring blood sugar. Photo: spukkato / freepik.com
Ask your doctor what your goal sugar level should be and how often you should check it. Staying as close to your target as possible will help you prevent or delay diabetes-related complications.
Diabetes while traveling
Before traveling, visit your doctor for advice about your itinerary, planned physical activity, and possible changes in insulin dosage and regimen.
Bring with you the necessary amount of insulin or prescriptions to purchase it. Check to see if your drug is available where you are going. Stock up on test strips for your glucose meter: changing your diet can lead to fluctuations in glycemia. It is better to take with you 2 times more medications than you usually need.
Get a medical bracelet that indicates you have diabetes. Get travel insurance in case you miss your flight or need medical attention. Order a special meal on board or take food on the go.
Your continuous glucose meter and insulin pump may turn off during airport X-ray screening. Ask customs officials for a manual inspection.
Diet
Dietary restrictions for patients with type 1 diabetes are relevant if the dose of insulin administered is fixed. This primarily concerns carbohydrates. Their excess or deficiency can provoke surges in blood glucose.
If the dose of insulin is calculated every time before meals, you will not have to limit yourself in food. You just need to take into account how a particular product affects blood sugar levels by calculating its glycemic index (GI), and how much “short” insulin is needed to control carbohydrate metabolism after a particular food.
However, the diet for type 1 diabetes should be balanced and based on the principles of healthy eating. Pay special attention to the ratio of carbohydrates, fats and proteins: the amount of insulin you need directly depends on this.
For diabetes, doctors advise reducing consumption:
- salted, smoked, pickled dishes,
- foods high in starch and fat,
- confectionery products, sauces and semi-finished products.
Drink less fruit juices, sugary drinks and fast food - these are also harmful for a healthy person.
Physiotherapy
If you regularly engage in sports or fitness, alternating strength training with cardio exercise, remember the existence of a “carbohydrate window”. Due to inexperience, you can end up in a situation of life-threatening hypoglycemia. Therefore, be sure to inform your trainer about your diagnosis and do not practice alone at first. Avoid injecting insulin before exercise to avoid causing your blood sugar to drop. Calculate with your doctor how much you need to reduce your usual insulin dose on training days.
Important!
Patients with diabetes, like healthy people, benefit from feasible physical activity - walking, jogging, children - outdoor games. In the early stages of using insulin, avoid prolonged active swimming, mountain climbing, fast or strenuous cycling: an acute drop in blood sugar (due to the administration of too much insulin for such an intense activity) with weakness to the point of fainting can lead to injury and pose a threat to life.
How does type 1 diabetes develop?
What is the trigger for the development of type 1 diabetes, like all autoimmune diseases, there is still no exact answer. But the main cause of the disease is known - a lack of insulin occurs due to the death of cells in the islets of Langerhans. The islets of Langerhans are areas on the tail of the pancreas that produce endocrine cells that participate in various life processes.
The role of endocrine cells is extensive, to be convinced of this, it is enough to consider a few examples:
- Alpha cells produce glycogen, which stores energy in the liver. This polysaccharide is the main form of glucose storage: glycogen reserves in the liver in a healthy person can reach 6% of the total body weight. Glycogen from the liver is available to all organs and can quickly replenish glucose deficiency in the body.
- Beta cells produce insulin, which converts glucose from the blood into energy. If the number of beta cells is insufficient or their work is poor, there is not enough insulin, so glucose remains unchanged in the blood.
- Delta cells are responsible for the production of somatostatin, which is involved in the functioning of the glands. Somatostatin limits the secretion of somatotropin - growth hormone.
- PP cells stimulate the production of gastric juice, without which complete digestion of food is impossible.
- Epsilon cells secrete a secretion that stimulates appetite.
The islets of Langerhans are equipped with capillaries, innervated by the vagus and peripheral nerves, and have a mosaic structure. The islets that produce certain cells are interconnected. Beta cells that produce insulin inhibit the production of glucogen. Alpha cells suppress the production of beta cells. Both islets reduce the amount of somatostatin produced.
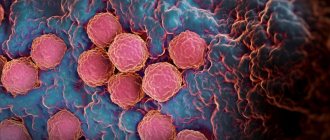
Failure of immune mechanisms leads to the body's immune cells attacking the cells of the islets of Langerhans. Due to the fact that 80% of the surface of the islets is occupied by beta cells, they are the ones that are destroyed the most.
Dead cells cannot be restored; the remaining cells produce too little insulin. It is not enough to process the glucose entering the body. All that remains is to take insulin artificially in the form of injections. Diabetes mellitus becomes a lifelong death sentence; it cannot be cured and leads to the development of concomitant diseases.
Causes of type 1 diabetes mellitus
The development of type 1 diabetes is provoked by the following diseases:
- Severe viral infections
(rubella, chickenpox, cytomegalovirus, hepatitis, mumps). In response to infection, the body produces antibodies that, simultaneously with the virus cells, destroy beta cells, which are in many ways similar to the infection cells. In 25% of cases, after suffering from rubella, a person is diagnosed with diabetes mellitus. - Autoimmune diseases of the thyroid gland and adrenal glands
that produce hormones: autoimmune thyroiditis, chronic adrenal insufficiency. - Hormonal diseases
: Itsenko-Cushing syndrome, diffuse toxic goiter, pheochromocytoma. - Long-term use of a number of medications
. Antibiotics, tablets against rheumatism, dietary supplements with selenium are dangerous - they all provoke hyperglycemia - increased levels of glucose in the blood. - Pregnancy
. Hormones produced by the placenta increase blood sugar levels. The pancreas is under increased stress and cannot cope with the production of insulin. This is how gestational diabetes develops. This disease requires observation and may disappear without a trace after childbirth. - Stress.
When a person is very nervous, a large amount of adrenaline and glucocorticosteroids are released into the blood, which destroy beta cells. In patients with a genetic predisposition, it is after stress that a diagnosis of type 1 diabetes is made.
Causes of type 1 diabetes in children and adolescents
Many parents are mistaken in thinking that diabetics got sick because they ate a lot of chocolate and sugar. If you limit your child’s sweets, he can be protected from diathesis rather than from diabetes. Children get diabetes at an early age not because of poor diet. This is evidenced by the findings of scientists studying this problem.
The authoritative scientist Andreas Beyerlein from the Munich Helmholtz Center conducted a study, upon completion of which the following conclusions were made:
- A severe viral infection suffered at the age of 0-3 years leads to the development of type 1 diabetes mellitus in 84%, and the pathology is more often diagnosed when the child reaches the age of 8.
- Acute acute respiratory viral infection suffered by infants under 3 months causes diabetes in 97% of cases.
- In children with a hereditary predisposition to hyperglycemia, the risk of developing the disease increases depending on nutritional factors (nutrition): artificial feeding, early consumption of cow's milk, high birth weight (above 4.5 kg).
There are two peak ages for detecting diabetes in children - 5-8 years and adolescence (13-16 years). Unlike adults, childhood diabetes develops very quickly and rapidly. The disease manifests itself as an acute form of ketoacidosis (poisoning by ketone bodies formed in the liver) or diabetic coma.
As for heredity, the likelihood of transmitting T1DM is low. If the father has type 1 diabetes, the risk of transmission to children is 10%. If the mother, then the risks are reduced to 10%, and in late births (after 25 years) to 1%.
Identical twins have different risks of getting the disease. If one child is sick, the disease occurs in the second no more than 30-50%.
Signs and symptoms of diabetes in adults
Listed here are the classic symptoms of diabetes mellitus (DM). Read carefully and listen to your body.
- Constant fatigue.
Constant fatigue reduces a person’s activity and performance, worsening his well-being. If you don’t feel alert even after sleep, you should think about it. - Persistent hunger.
How to distinguish hunger caused by some disease from ordinary hunger not associated with disease? Find out more about this. - Numbness and pain in the legs.
One of the main and most common complications of diabetes is diabetic polyneuropathy. Therefore, when loss of sensation or numbness in the limbs occurs, it is important to understand that this may be a symptom of diabetes. - Intense thirst.
A symptom that cannot be ignored. With the development of diabetes mellitus, a person, experiencing thirst, drinks from 2 to 6 liters (10-30 glasses) of liquid per day. - Frequent urination.
In diabetes, urine volume can reach 10 liters per day. If you notice frequent and excessive urination, this is a reason to consult a doctor for diagnosis. - Blurred vision.
Symptoms of visual impairment in diabetes mellitus may include: gradual deterioration of vision, spots, threads or other shadows “floating” in the field of vision, etc. Find out more about this. - Unexplained weight loss.
If you notice that within a few months you have inexplicably begun to lose weight without a special program, then such weight loss is a reason to consult a doctor, because this may be a symptom of diabetes. - Long-term healing of wounds.
There may be several reasons, and one of them is manifestations of diabetes mellitus. If you begin to notice wounds, scratches, or ulcers that take a long time to heal, do not ignore it.
Complications of type 1 diabetes
In addition to diabetes itself, its complications are no less dangerous. Even with a slight deviation from the norm (5.5 mmol/liter on an empty stomach), the blood thickens and becomes viscous. Vessels lose their elasticity, and deposits in the form of blood clots (atherosclerosis) form on their walls. The internal lumen of arteries and vessels narrows, organs do not receive sufficient nutrition, and the removal of toxins from cells is slowed down. For this reason, places of necrosis and suppuration appear on the human body. Gangrene, inflammation, rash occurs, and blood supply to the extremities deteriorates.
High blood sugar disrupts the functioning of all organs:
- Kidneys
. The purpose of the paired organs is to filter the blood from harmful substances and toxins. When the sugar level is more than 10 mmol/liter, the kidneys stop doing their job efficiently and pass sugar into the urine. A sweet environment becomes an excellent base for the development of pathogenic microflora. Therefore, hyperglycemia is usually accompanied by inflammatory diseases of the genitourinary system - cystitis (inflammation of the bladder) and nephritis (inflammation of the kidneys). - The cardiovascular system.
Atherosclerotic plaques, formed due to increased blood viscosity, line the walls of blood vessels and reduce their capacity. The cardiac muscle myocardium ceases to receive adequate nutrition. This is how a heart attack occurs - necrosis of the heart muscle. If a sick person does not suffer from diabetes, he will feel discomfort and a burning sensation in the chest during a heart attack. A diabetic suffers from decreased sensitivity of the heart muscle and may die unexpectedly. The same goes for blood vessels. They become brittle, increasing the risk of stroke. - Eyes
. Diabetes damages small vessels and capillaries. If a blood clot blocks a large vessel of the eye, partial death of the retina occurs, and detachment or glaucoma develops. These pathologies are incurable and lead to blindness. - Nervous system.
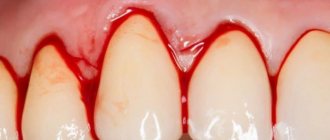
Poor nutrition, associated with serious restrictions in type 1 diabetes, leads to the death of nerve endings. A person stops reacting to external stimuli, he does not notice the cold and freezes his skin, does not feel the heat and burns his hands. - Teeth and gums.
Diabetes is accompanied by diseases of the oral cavity. The gums soften, tooth mobility increases, gingivitis (inflammation of the gums) or periodontitis (inflammation of the inner surface of the gums) develops, which leads to tooth loss. The effect of insulin-dependent diabetes on the teeth of children and adolescents is especially noticeable - they rarely have a beautiful smile: even their front teeth deteriorate. - Gastrointestinal tract
. In diabetes, beta cells are destroyed, and along with them the PP cells responsible for the production of gastric juice. Patients with diabetes often complain of gastritis (inflammation of the stomach lining), diarrhea (diarrhea due to poor digestion of food), and the formation of gallstones. - Problems with bones and joints
. Frequent urination leads to the leaching of calcium, resulting in damage to the joints and skeletal system, and an increased risk of fractures. - Leather
_ Increased blood sugar leads to the loss of protective functions of the skin. Small capillaries become clogged with sugar crystals, causing itching. Dehydration makes the skin wrinkled and very dry. In some cases, patients develop vitiligo - the breakdown of skin cells that produce pigment. In this case, the body becomes covered with white spots. - Female reproductive system
. A sweet environment creates favorable soil for the development of opportunistic microflora. In type 1 diabetes, frequent relapses of thrush are typical. Women have poor vaginal lubrication, which makes sexual intercourse difficult. Hyperglycemia negatively affects fetal development in the first 6 weeks of pregnancy. Diabetes also leads to premature menopause. Early menopause occurs at 42-43 years.
Lectures DM1
The main chronic complications of type 1 diabetes, the mechanism of their development, clinical manifestations, measures to prevent the development of chronic complications, early diagnosis.
Fig.1
IN WHICH ORGANS DO COMPLICATIONS OF DIABETES DEVELOP?
Diabetes mellitus, if poorly controlled, can lead to adverse consequences: due to increased levels of glucose in the blood, diabetes-specific complications in the eyes, kidneys, and legs gradually arise and progress very quickly. And the “insidiousness” of diabetes is that these complications appear 10-15 years after the onset of the disease, develop unnoticed and at first do not affect your well-being. Unfortunately, it can be very difficult to cope with complications that have already manifested themselves. Therefore, diabetes must be well controlled from the very beginning of the disease. If some initial manifestations of complications have appeared, then improved control will help prevent them from developing. Small vessels in the eyes and kidneys are affected - this is called microangiopathy. The walls of small vessels, being in constant contact with the blood flowing inside the vessels, are very sensitive to increased glucose levels. Under its influence, irreversible changes gradually occur in the vascular wall, as a result of which the blood supply, and therefore the nutrition of the entire organ, deteriorates. This, in turn, leads to disruption of its operation.
EYE DAMAGE. DIABETIC RETINOPATHY
Fig.2
In the eyes, against the background of constantly elevated blood glucose levels, the retina is affected. The retina lines the inside of the eyeball.
The basis of the retina is a plexus of small vessels; it also contains nerve endings that provide vision function. A complication of diabetes caused by changes in the blood vessels of the retina is called diabetic retinopathy (the word comes from the Latin name for the retina - retina, which means “network”).
The meaning of the frequently used term “fundus” should also be explained. This is the name for the part of the inner lining of the eye that is visible during a special examination performed by an ophthalmologist, i.e. retina. So, the cause of diabetic retinopathy is long-term decompensation of diabetes. In diabetic retinopathy, retinal vessels become more fragile, permeable, and lose elasticity, which leads to the development of microaneurysms - protrusions on the vessels, and then to hemorrhages. Diabetic retinopathy develops gradually, and even quite pronounced stages may be imperceptible to a person. In other words, if a diabetic patient does not complain of decreased vision, this does not mean that he does not have retinopathy! With further development of the process, new formation of retinal vessels may occur, followed by massive hemorrhages (this is called proliferative retinopathy). In this case, a significant decrease in visual acuity may occur. The presence and severity of this complication of diabetes can only be determined by an ophthalmologist (ophthalmologist) by examining the fundus of the eye with a dilated pupil. To dilate the pupil, special drops are instilled into the eyes, after which vision temporarily becomes blurry and unclear. This procedure is necessary, since sometimes in diabetic retinopathy the main changes are located on the periphery of the retina, while in the central zone, which is visible without dilating the pupil, they are not yet present. An ophthalmologist examines the fundus using a special device.
If there is a noticeable deterioration in vision, you can choose glasses from an ophthalmologist. However, it is not possible to improve vision affected by retinopathy with glasses. The same changes that can be corrected by choosing glasses are not associated with retinopathy, although they sometimes cause unreasonably strong anxiety for the patient, since he attributes them to complications of diabetes.
Every person with diabetes should visit an ophthalmologist at least once a year.
If retinopathy is present, the frequency of examinations should increase (how often is decided by the ophthalmologist), since at some point treatment may be necessary. Immediate examination should be carried out if there is a sudden deterioration in vision.
PREVENTION AND TREATMENT OF DIABETIC RETINOPATHY
The basis for the prevention of retinopathy, as well as all complications of diabetes, is maintaining good diabetes compensation, i.e. maintaining blood glucose levels as close to normal as possible. Regular eye examinations are extremely important, as discussed above.
It should also be noted that the condition of the fundus of the eye is negatively affected by disorders such as high blood pressure, blood cholesterol, and smoking. To preserve vision, it is important that these indicators are monitored and maintained within normal limits. The level of total cholesterol (it must be determined at least once a year) should be below 5.2 mmol/l (according to the latest data, below 4.5 mmol/l); Blood pressure levels will be discussed in the section on kidney damage.
You should not rely on unproven methods of treatment - advertisements for some “magic” plants, etc. appear from time to time. Currently, there are no effective medications for the treatment and prevention of diabetic eye damage.
A reliable method of treating diabetic retinopathy, recognized and successfully used throughout the world, is laser coagulation of the retina. Timely and correctly performed laser coagulation allows you to preserve vision even in the later stages of diabetic retinopathy. However, treatment is most effective in the early stages of retinopathy.
Laser photocoagulation is an outpatient procedure that is performed in one or more sessions and is completely safe. Its meaning is to use a laser beam to influence the altered retina, which helps prevent further progression of the process. It should be understood that this type of treatment only stops the further development of diabetic retinopathy, but if there is already a significant decrease in vision, there is no return to completely good vision. This is why it is so important to carry out laser coagulation in the early stages, when vision has not yet been reduced.
A prerequisite for a lasting positive effect from laser photocoagulation is good compensation of diabetes; in its absence, the progression of retinopathy will continue.
In severe proliferative diabetic retinopathy in the case of severe hemorrhages in the vitreous body (hemorrhages are an obstacle to light and also threaten retinal detachment), the use of surgical treatment methods is necessary. A so-called vitrectomy is performed - removal of the vitreous body. To avoid acute situations (massive hemorrhages, retinal detachment), which can lead to irreparable consequences, you need to avoid heavy physical activity. Heavy lifting is dangerous, as is severe straining, which can occur with constipation or a persistent cough.
CATARACT
Fig.3
In diabetes mellitus, along with retinal damage, clouding of the lens, which is called cataracts, often occurs. This disease is also common among people who do not have diabetes, especially in older age groups.
If the clouding of the lens is severe, the penetration of light rays to the retina is difficult and vision deteriorates significantly, up to its complete loss. The treatment of cataracts is now well established; a radical method is surgery to remove the clouded lens. Vision is restored after such an operation, although it requires correction with glasses or by replacing the removed lens with an artificial one. It is important for a diabetic patient to know that any operations, including lens removal, proceed successfully only against the background of good compensation for diabetes. This condition is also put forward by ophthalmological surgeons.
KIDNEY DAMAGE. DIABETIC NEPHROPATHY
Fig.4
Against the background of long-term decompensation of diabetes in the kidneys, small vessels are affected, which are the main part of the renal glomerulus (kidney tissue consists of many such glomeruli). The vessels of the renal glomerulus provide the function of the kidneys, which act as a filter in the human body. The kidneys excrete unnecessary substances in the urine, filtering them from the blood; necessary substances are retained, sending them back into the blood.
When, due to an increased level of glucose in the blood, the vessels of the renal glomeruli change, the normal functioning of the renal filter is disrupted and protein, which is a necessary substance and does not normally enter the urine, begins to penetrate there.
A complication of diabetes caused by damage to blood vessels in the kidneys is called diabetic nephropathy. In the early stages, its development cannot be felt in any way.
Every diabetic patient must undergo a urine test at least once a year to determine the protein in it.
This can be a regular, so-called general urine test, which is done in any clinic. However, diabetic nephropathy can be detected at earlier stages, which is very important for therapeutic and preventive measures. This is a urine test for microalbuminuria, i.e. micro amounts of albumin protein. Daily urine is collected: the norm is the excretion of up to 30 mg of protein per day, micro albuminuria - from 30 to 300 mg, proteinuria - more than 300 mg. By the way, the appearance of protein in the urine does not always indicate diabetic nephropathy. This may also be a manifestation of the inflammatory process in the kidneys, for example, an exacerbation of chronic pyelonephritis. At the same time, there will be other changes in the urine.
INCREASED BLOOD PRESSURE
Fig.5
Elevated blood pressure levels are not always accompanied by some unpleasant sensations. The danger of increased blood pressure is that it itself causes serious harm to the kidneys, i.e. a kind of vicious circle develops: high blood glucose levels → kidney damage → increased blood pressure → kidney damage → increased blood pressure.
Therefore, elevated blood pressure levels, regardless of the causes, must be reduced. The maximum permissible level is currently considered to be 140 mmHg. Art. - for the upper indicator (systolic blood pressure) and 85 mm Hg. Art. - for lower (diastolic blood pressure). If at least one of these two indicators is often above the specified limits, treatment is necessary.
PREVENTION AND TREATMENT OF DIABETIC NEPHROPATHY
As with diabetic retinopathy, prevention and treatment of diabetic nephropathy primarily includes compensation for diabetes mellitus, i.e. maintaining blood glucose levels as close to normal as possible. If a persistent increase in blood pressure is registered, the doctor will prescribe appropriate treatment. There are now a lot of medications for the treatment of arterial hypertension, and effective treatment can be selected for every diabetic patient. It is important for the patient to understand that these medications must be taken constantly, i.e. not only with high blood pressure, but also with blood pressure that has dropped to normal, so that it does not increase! In this case, an obligatory component of treatment will be independent monitoring of blood pressure at home, in particular to assess the effectiveness of the drugs used, therefore all people with arterial hypertension need to have a device for measuring blood pressure (tonometer) at home and be able to use it.
It is necessary to measure blood pressure daily in the morning and evening, recording the data obtained in a self-monitoring diary for discussion with a doctor and selection of treatment. Recently, even in the presence of microalbuminuria (even without an increase in blood pressure), drugs are prescribed that, in principle, are intended to lower blood pressure (the so-called ACE inhibitors), but in this case are used to protect the kidney from further damage.
An important factor in the treatment of hypertension is limiting table salt to 3-5 g per day (it should be remembered that 1 teaspoon contains 5 g of salt). This involves excluding foods rich in salt from the diet (pickled cucumbers and tomatoes, sauerkraut, pickled mushrooms, herring, mineral water high in sodium, etc.). All canned foods tend to contain a lot of salt. Food should be prepared from natural products without adding salt. Don't be afraid to limit your salt! A healthy body requires only 0.5 g of salt per day, and we often eat up to 10-15 g.
If diabetic nephropathy reaches advanced stages, the doctor may recommend a special diet with limited protein (this mainly applies to animal products - meat, fish, eggs, cheese, cottage cheese, etc.). If renal failure develops (an indicator of this will be an increase in the level of creatinine in a biochemical blood test, it also needs to be determined for all patients with diabetes at least once a year), hemodialysis (artificial kidney) or a kidney transplant is used.
LEGS IMPAIRMENT
Fig.6
Why are the legs one of the most vulnerable parts of the body with diabetes? The fact is that the legs are affected by a number of external factors: walking, body weight, shoes. In diabetes mellitus, these factors can include damage to nerves, blood vessels, and impaired ability to heal wounds.
Young people with type 1 diabetes primarily experience nerve damage called diabetic polyneuropathy, which is associated with long-term high blood glucose levels. At a more mature age, damage to large vessels is also possible, which is a manifestation of atherosclerosis and is often associated with an increase in such indicators as cholesterol levels in the blood. However, elevated blood glucose levels aggravate the severity of the atherosclerotic process.
Manifestations of diabetic neuropathy include various types of pain in the legs, a burning sensation, “crawling sensations,” tingling, and numbness. These symptoms can be very painful, but there is another danger that is not always noticeable to a diabetic patient. Neuropathy is characterized by a decrease in the sensitivity of the legs: the ability to perceive the effects of high and low temperatures, pain (for example, a prick with a sharp object), etc., is lost. This poses a great danger because it increases the risk and makes minor injuries invisible, for example, when foreign objects get into shoes, wearing incorrectly selected shoes, when treating nails, calluses.
Decreased sensitivity combined with foot deformities common in diabetes leads to improper distribution of pressure when walking. This leads to trauma to the tissues of the foot, up to the formation of ulcers in areas of greatest stress. The so-called diabetic foot syndrome occurs. Areas of trauma can become inflamed and infection develops. The inflammatory process in conditions of reduced sensitivity occurs without pain, which can lead to underestimation of the danger. Self-healing does not occur if diabetes compensation is unsatisfactory, and in severe advanced cases the process can progress, leading to the development of purulent inflammation - phlegmon.
In the worst case scenario and in the absence of treatment, tissue necrosis - gangrene - can occur. A sign of damage to large arteries and impaired blood supply at severe stages is pain in the legs when walking. They occur in the lower legs even after walking for a short time, and the person must stop and wait until the pain goes away before continuing on. This pattern is called “intermittent claudication.” Coldness of the feet may also be a concern.
PREVENTION AND TREATMENT OF LEG LESIONS
Since diabetic feet are at such great risk, every diabetic patient should be familiar with measures to prevent the complications described above. First of all, this is a good compensation for diabetes; it cannot be replaced by any other preventive and therapeutic purposes, including medications! In addition, you need to stop smoking and monitor your blood pressure and cholesterol levels.
It is advisable to undergo a medical examination of your feet at least once a year (with determination of various types of sensitivity and pulsation in the arteries of the feet)
Examination of the feet is best done in a specialized office “Diabetic foot” - there are more and more such offices in our country in recent years. In addition, every diabetic patient should be familiar with a set of preventive measures to reduce the risk of leg damage. Preventive measures can be presented in the form of “prohibiting” and “permitting” rules, which we present below.
FOOT CARE RULES
Fig.7
This cannot be done if you have diabetes!
First of all, you should not use any sharp objects when caring for your feet: scissors, callus knives, razor blades. The use of such objects is one of the most common causes of injury, especially in conditions of reduced sensitivity and poor vision! In the absence of these “risk factors”, using scissors is possible, but you should not cut your nails too short and cut the corners too deep. This can lead to the formation of a so-called ingrown nail - the cause of pain, inflammation and long-term treatment, including surgery. Wearing tight shoes also contributes to ingrown toenails.
If your feet are cold, you cannot warm them with heating pads (including electric ones), steam heating radiators, or electric heating devices. Temperature sensitivity in a diabetic patient is often reduced, so it is easy to get burned.
For the same reason, you should not take hot foot baths. The water temperature should not be higher than 37 °C (it is better to measure it with a water thermometer, as for bathing children). In addition, foot baths should not be long - this loosens the skin and makes it more vulnerable.
It is not recommended to walk without shoes, as there is a high risk of injury with simultaneous penetration of infection into the area of injury. You must wear bathing slippers on the beach and when swimming. You should also protect your feet from sunburn.
It is necessary to avoid uncomfortable (narrow, chafing, pressing) shoes and not to wear high-heeled shoes. High heels contribute to poor circulation in the foot and the formation of areas of increased pressure on its plantar surface. You need to be careful with new shoes: wear them for no more than 1 hour for the first time, and also never use any breaking-in methods, such as putting them on a wet sock. An additional risk of injury is created by shoes that open and therefore do not protect the toes and heel. Sandals or sandals with a strap that goes between the toes can injure the delicate skin in this area. It is unacceptable to wear shoes on bare feet due to the high likelihood of abrasions.
If you have calluses on your feet, you should not try to get rid of them with callus fluids, ointments or patches, as they all contain substances that corrode the skin. Calluses usually form as a result of wearing ill-fitting shoes that put pressure on the foot in certain places.
You should pay attention to the elastic bands of your socks. If they are too tight and leave indentations on the skin of the shins, it impedes blood circulation.
This is how you need to take care of your feet if you have diabetes!
Every day, a diabetic patient should carefully examine his feet, especially the plantar surface, heel area and interdigital spaces. Older people and overweight people may experience considerable difficulty with this. They may be advised to use a mirror placed on the floor during the examination, or ask relatives to do this, especially if their vision is impaired. Daily inspection allows you to promptly detect wounds, cracks, and abrasions.
It is necessary to wash your feet daily. After washing your feet, wipe them dry with a soft towel, especially in the spaces between the toes. High humidity in these areas contributes to the development of diaper rash and fungal diseases. For the same reason, when using a moisturizer for excessively dry skin, you should not apply it between your fingers.
Nails should be treated regularly (at least once a week) using a file. This will not only avoid injury, but also form the correct horizontal edge of the nail, leaving its corners untouched.
The most suitable remedy for removing calluses and areas of excessive keratinization (thickening and dryness) of the skin is pumice. It is better to buy a special pumice stone for foot care at the pharmacy. You should use it while washing your feet and do not try to get all problem areas in complete order in one go.
If your feet are cold, you need to warm them up with warm socks of the appropriate size and without tight elastic bands. It is necessary to ensure that the socks do not bunch up in the shoes.
You should make it a rule to check the inside surface of your shoes before putting them on: whether any foreign objects have gotten inside, whether the insole is curled up, or whether sharp nails are showing through. Let us remind you once again that this is necessary due to the fact that the sensitivity of the feet can be reduced, which the person with diabetes is not aware of.
Your feet are protected when you wear the right shoes. If necessary, advice on choosing shoes can be obtained from the Diabetic Foot office.
FIRST AID FOR FOOT INJURIES
Even minor injuries to the feet should be shown to a doctor, but a person should be able to provide first aid to himself. If, when examining your feet, a wound, abrasion or crack is discovered, you need to wash it with a disinfectant solution. You can use a 1% solution of dioxidin, 0.01% solution of miramistin or 0.02% solution of furatsilin. The washed wound should be covered with a sterile bandage or bactericidal patch. You cannot use a regular adhesive plaster!
All of the above products must be in your home first aid kit, and also taken with you on trips. Do not use alcohol solutions (alcohol solution of iodine, brilliant green - brilliant green), as well as a concentrated, dark solution of potassium permanganate (potassium permanganate). They can cause burns and also stain the skin, preventing signs of developing inflammation from being seen. It is also undesirable to use oil dressings (with fat-based ointments), which create an environment for the development of infection and impede the drainage of secretions from the wound. There is no point in treating wounds with insulin; it has no healing effect. If signs of inflammation appear in the area of damage (redness, swelling, purulent discharge), immediate medical attention is needed. The best option would be to contact the Diabetic Foot office. Surgical debridement and antibiotics may be required. In such a situation, it is important to provide complete rest to the leg. The doctor may prescribe bed rest; if ambulation is necessary, use crutches to avoid putting stress on the leg.
CHECK-UPS FOR DIABETES
To summarize this section, I would like to emphasize once again that diabetes complications are preventable. To do this, first of all, regular monitoring of your condition by a diabetic patient is necessary. Let us repeat once again which indicators, in addition to blood glucose levels, need to be regularly monitored, as well as which specialists should be visited.
Glycated hemoglobin (HbA1c) - once every 6 months, if necessary, once every 3 months.
Level of cholesterol in the blood (preferably also other indicators of lipid metabolism), creatinine in the blood - at least once a year.
Blood pressure at every visit to the doctor or on your own at home.
Protein in the urine (microalbuminuria) - at least once a year.
Examination by an ophthalmologist with a dilated pupil - at least once a year.
Medical examination of the feet at least once a year. If problems are detected, more frequent monitoring is required, as well as treatment prescribed by a doctor and carried out with the active participation of the person himself.
The main reason for the development and progression of diabetes complications is long-term decompensation of the disease. In addition to daily self-monitoring of glycemia and blood pressure, and following foot care rules, a diabetic patient must undergo a series of annual examinations
Symptoms of type 1 diabetes
External signs help determine diabetes, because the disease affects the functioning of the entire body. In young people under 18 years of age, diabetes develops very quickly and rapidly. It often happens that 2-3 months after a stressful event (ARVI, moving to another country), a diabetic coma occurs. In adults, symptoms may be milder and gradually worsen.
The following signs are cause for concern:
- Frequent urination, a person goes to the toilet several times a night.
- Weight loss (dieting and the desire to lose weight in adolescence is fraught with the rapid development of hyperglycemia).
- The appearance of age-appropriate wrinkles, dry skin.
- Increased feeling of hunger with lack of weight.
- Lethargy, apathy, the teenager quickly gets tired, he begins to have painful thoughts.
- Fainting, severe headache, vision problems.
- Constant thirst, dry mouth.
- A specific smell of acetone from the mouth, and in severe cases from the body.
- Night sweats.
If at least a few symptoms are noticed, the patient should be immediately sent to an endocrinologist.
The younger the body, the faster the coma sets in.
Diagnosis of diabetes mellitus
The endocrinologist will definitely prescribe the following tests for diabetes:
- Test for blood glucose levels
. Blood is taken on an empty stomach; the last meal should be no earlier than 8 hours before. A reading below 5.5 mmol/liter is considered normal. An indicator of up to 7 mmol/liter indicates a high predisposition; 10 mmol/liter and above indicates hyperglycemia. - Oral glucose tolerance test
. This test is done for those who are at risk of developing diabetes. The patient takes a glucose solution on an empty stomach. Then, 2 hours later, blood is taken for sugar. Normally, the reading should be below 140 mg/dL. A blood sugar level above 200 mg/dL confirms diabetes mellitus. - Test for glycosylated hemoglobin A1C
. Excess sugar in the blood reacts with hemoglobin, so the A1C test shows how long the body's sugar levels have been above normal. Monitoring is carried out every 3 months, the level of glycosylated hemoglobin should not exceed 7%. - Blood test for antibodies
. Type 1 diabetes is characterized by an abundance of antibodies to the cells of the islets of Langerhans. They destroy body cells, which is why they are called autoimmune. By identifying these cells, the presence and type of diabetes is determined. - Urinalysis - microalbuminuria
. Detects protein in urine. It appears not only with kidney problems, but also with vascular damage. High levels of albumin protein lead to heart attack or stroke. - Screening for retinopathy
. High glucose levels lead to blockage of small vessels and capillaries. The retina of the eye does not receive nourishment; it peels off over time and leads to blindness. Special digital equipment allows you to take pictures of the back surface of the eye and see the location of damage. - Test for thyroid hormones.
An overactive thyroid gland leads to hyperthyroidism—excessive production of hormones. Hyperthyroidism is dangerous because the breakdown products of thyroid hormones increase the level of glucose in the blood; diabetes is accompanied by acidosis (high levels of acetone in the urine), osteoporosis (leaching of calcium from the bones), and arrhythmia (failure of heart rhythm).
Treatment of type 1 diabetes
Type 1 diabetes is not curable because beta cells cannot be restored. The only way to maintain normal blood sugar levels in a sick person is to take insulin, a hormone produced by the beta cells of the islets of Langerhans.
Based on the speed of action and duration of effect, medications containing insulin are divided into categories:
- Short-acting (Insuman Rapid, Actrapid)
. They begin to act 30 minutes after administration, so they should be taken half an hour before meals. When the drug is administered intravenously, it is activated after a minute. The duration of the effect is 6-7 hours. - Ultra-short-acting (Lispro, Aspart).
They begin to work 15 minutes after the injection. The action lasts only 4 hours, so the drug is used for pump administration. - Medium duration (Insuman Bazal, Protafan).
The effect occurs an hour after administration and lasts 8-12 hours. - Long-term exposure (Tresiba).
The drug is administered once a day, it does not have a peak effect.
Medicines are selected individually for the patient in combination with other drugs that prevent the negative effects of high blood glucose.
Diet
For type 2 disease with excess weight, it is recommended to reduce caloric intake in order to reduce body weight. We are not talking about strict restrictions (on the contrary, strict diets and fasting are contraindicated), but about the gradual formation of a healthy eating style. To lose weight, you need to limit animal fats and sugars, reduce starchy foods and proteins in the menu. Vegetables rich in fiber can be eaten in unlimited quantities.
It is recommended to supplement the menu with polyunsaturated fatty acids: fish, vegetable oils 7. Dishes are prepared boiled, stewed, baked, or steamed. If possible, meals should be divided into 3-6 meals. Daily salt intake should be reduced to 5-8 g. When using insulin, it is important to calculate the amount of carbohydrates.
Drinking alcohol is harmful to health. In diabetes mellitus, alcoholic beverages can also complicate disease control. In the absence of complications of diabetes and digestive pathology, the maximum permissible dose for men is 2 conventional units per day, for women - 1 conventional unit per day, without daily use (1 conventional unit = 15 g of ethanol or 40 g of strong drinks, or 140 g of wine, or 300 ml beer).
Dosed use of sweeteners is acceptable 8.
Exercise for diabetes
Physical activity for type 1 diabetes is simply necessary, although there are restrictions regarding the type of sport. Exercise normalizes blood pressure, improves well-being, and normalizes weight. But in some cases, physical activity causes spikes in blood glucose levels.
If you have type 1 diabetes, you cannot overload yourself, so training should not exceed 40 minutes a day. The following sports are acceptable:
- walking, cycling;
- swimming, aerobics, yoga;
- table tennis, football;
- exercises in the gym.
Any exercise is contraindicated if ketones, protein breakdown products, are found in the urine, and if blood pressure has increased or problems with blood vessels have appeared.
Consequences and complications
Due to the use of an excessive dose of hypoglycemic drugs, excessive physical activity, and during prolonged fasting, a state of hypoglycemia develops - low blood glucose levels. Symptoms: palpitations, trembling, extreme hunger, sweating, dizziness and loss of consciousness. It is necessary to urgently increase the glucose level, because with its prolonged deficiency, loss of consciousness or even a hypoglycemic coma can develop.
Elevated glucose levels over a long period of time disrupt the structure of small and large vessels. Small vessel lesions most often occur in the kidneys and retina. Pathological changes in large vessels can cause heart attacks, strokes, and the formation of long-term non-healing ulcers, which can lead to loss of limbs 5.