What is diabetes mellitus? And what types is it?
Diabetes mellitus is a term that unites a group of diseases accompanied by an increase in glucose (sugar) in the blood. There are many different types of diabetes, but the main two are:
- Type 1, insulin-dependent
- it is also called “childhood” or “young people’s diabetes”, since it mainly affects children or young people; - Type 2, non-insulin dependent
- it is called “diabetes of the elderly”, since it is more common in older people. However, recently it has been diagnosed in young people and even children.
What is the etiology of diabetes mellitus?
The etiology is not exactly known.
But one of the reasons for the occurrence of diabetes is that the risk of the disease can be inherited. But this does not mean that if one of your family members has diabetes, then your child will definitely have it. Or, on the contrary, it may be that neither the mother, nor the father, nor the grandparents had diabetes, but the child was diagnosed with it. Diabetes mellitus can occur for various reasons: childhood infections and viral colds, as well as stress in children who have an increased predisposition to this disease. Moreover, the impact of these factors can occur long before the first signs of diabetes appear. Type 1 diabetes occurs because the body does not have enough insulin .
As a result, blood sugar levels increase.
Correct analysis
In order not to traumatize an impressionable child with a picture of medical realities, you can purchase a glucometer, which allows you to carry out the procedure at home as simply as possible. But for prevention once a year, such a purchase is unlikely to be rational, since it is not cheap. In this case, it is easier to use the services of laboratories.
A blood sugar test should certainly be carried out on an empty stomach, approximately eight or nine hours after eating food, performing intense exercise and drinking a significant amount of liquid. Children under three years of age are allowed a maximum of 3 hours of fasting.
In addition, it must be taken into account that the glucose level can fluctuate significantly during illnesses, especially severe ones. In this regard, it is better to refuse to perform the study at this time.
Blood from children is taken from a finger. And for babies also - from a toe, earlobe or heel.
What are the symptoms of diabetes?
One of the first symptoms of diabetes is frequent urination
. Due to the fact that the child begins to go to the toilet frequently, gets up at night, becomes thirsty, and begins to drink more liquid. Parents usually notice that the child begins to drink a lot of water. Due to the fact that the sick child drinks and eats a lot, he begins to lose weight. Next, weakness and fatigue appear.
How is diagnosis carried out? Childhood diabetes is fairly easy to diagnose. We measure blood and urine glucose levels, as well as ketone levels.
How dangerous is this disease?
This disease is associated with a lack of insulin in the body.
And the only treatment so far is the administration of this hormone. Since insulin was invented only in the 20s of the 20th century, in former times children with diabetes died. If insulin is not administered at the right time, glucose cannot enter the cell. Insulin, like a key, opens the entrance to the cell for glucose. Our body uses glucose as energy, like fuel for a car. Thanks to this we move, breathe, work, think. If there is no main source of energy - glucose, then our body begins to draw energy from other sources: proteins and fats, which is why children lose weight. And when fat is used as energy, many harmful substances are formed that poison the child’s body ,
which can lead to death.
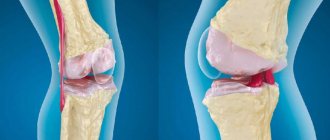
Does its clinical picture differ from diabetes mellitus in adults? In type 1 diabetes, the pancreas produces almost no insulin. In type 2 diabetes, insulin in the blood may even be increased, but due to a decrease in the sensitivity of body cells to insulin, its action is impaired. Most often this occurs due to obesity.
Well, the symptoms, as a rule, are exactly the same: frequent urination, thirst.
Are there any pre-diabetic conditions that would suggest a problem? In children, this is often an acute process. If pancreatic cells produce insulin in sufficient quantities, then there is no increase in blood glucose. Childhood diabetes occurs when less than 10% of insulin-producing cells remain.
Who is at risk? Hard to tell. For childhood diabetes there is no such thing as a risk group - it can “shoot” in any child ,
in any family.
Of course, the risk of developing diabetes is higher for those who have a family history of the disease. But, as I already said, this does not mean that it will necessarily develop. Also, premature babies and children born with low birth weight are more susceptible to this disease, as well as children who are bottle-fed and those who already have some kind of autoimmune disease. Parental smoking can play an unfavorable role.
Hypoglycemic state in children
A rare case of organic hyperinsulinism in a 3-month-old child
The fasting blood glucose level in a practically healthy person ranges from 3.3 to 5.5 mmol/l when determined by the glucose oxidase method. During the day, glucose in blood plasma can normally fluctuate from 2.8 to 8.8 mmol/l. Blood glucose levels below 2.7 mmol/l are commonly called hypoglycemia.
The main cause of the hypoglycemic symptom complex is hyperinsulinism.
Hyperinsulinism is a pathological condition of the body caused by an absolute or relative excess of insulin, causing a significant decrease in blood sugar; as a consequence, glucose deficiency and oxygen starvation of the brain occur, which leads primarily to disruption of higher nervous activity.
Absolute hyperinsulinism is a condition associated with pathology of the insular apparatus (primary organic hyperinsulinism). The most common causes of organic hyperinsulinism are insulinoma - a tumor of b-cells of the islets of Langerhans, secreting excess amounts of insulin (in adults and older children) and nesidioblastosis - hyperplasia of the pancreatic islets (in children of the first year of life). Another common cause of hyperinsulinism in young children is functional hyperinsulinism in newborns from mothers with diabetes.
Benign adenoma of the islets of Langerhans was first discovered in 1902 during an autopsy by Nicholls. In 1904, L.V. Sobolev described the “struma of the islets of Langerhans.” In 1924, Harris and the domestic surgeon V.A. Oppel independently described the symptom complex of hyperinsulinism. In the same year, G. F. Lang observed multiple adenomatosis of pancreatic islets. In Russia, a successful operation to remove insulinoma was performed in 1949 by A. D. Ochkin, and in 1950 by O. V. Nikolaev. An insulin-secreting tumor has been described in all age groups, from newborns to the elderly, but more often it affects people of working age - from 30 to 55 years. Among the total number of patients, children make up only about 5%. 90% of insulinomas are benign. About 80% of them are solitary. In 10% of cases, hypoglycemia is caused by multiple tumors, 5% of them are malignant, and 5% are nesidioblastosis (Antonov A.V. Clinical endocrinology, 1991).
The term nesidioblastosis was introduced by G. Laidlaw in 1938. Nesidioblastosis is a total transformation of the ductal epithelium of the pancreas into β-cells that produce insulin. In children of the first year of life, this is the most common cause of organic hyperinsulinism (only 30% of hyperinsulinism in children is caused by insulinoma, 70% by nesidioblastosis). This is a genetically determined disease.
The diagnosis is established only morphologically after excluding insulinoma. Clinically, it manifests itself as severe hypoglycemia that is difficult to correct, as a result of which, in the absence of a positive effect from conservative treatment, it will be necessary to resort to reducing the mass of pancreatic tissue. The generally accepted volume of surgery is 80 - 95% resection of the gland.
Insulinomas in children are extremely rare and are located either in the tail or in the body of the pancreas. Their diameter ranges from 0.5 to 3 cm. The small size of insulinomas creates difficulties for diagnosis (the information content of the ultrasound method is no more than 30%). To determine the location of insulinoma, selective angiography, CT and MRI, or scanning with an octreotide isotope (an analogue of somatostatin) are used. The most informative is angiography with selective blood sampling from the pancreatic veins (60 - 90%).
Insulinoma is manifested by a more or less sharp drop in blood sugar levels, which is caused by increased secretion of insulin into the blood. The radical method of treating insulinoma is surgery (insulinomectomy); the prognosis in most cases is favorable (88 - 90%) with timely surgical intervention.
Organic hyperinsulinism (insulinoma, nesidioblastosis) is the cause of severe pancreatic hypoglycemia with a drop in blood sugar to 1.67 mmol/l and lower (during an attack). These hypoglycemia are always non-ketotic (acetone in the urine is negative due to the suppression of lipolysis processes).
The most common in clinical practice is ketotic hypoglycemia (with acetonuria). Ketotic hypoglycemia is extrapancreatic and can be endocrine- and non-endocrine-dependent. They are accompanied by relative hyperinsulinism, that is, not associated with the pathology of the insular apparatus of the pancreas (secondary, functional, symptomatic hyperinsulinism). Relative hyperinsulinism is caused by an increase in the body's sensitivity to insulin normally secreted by b-cells of the pancreatic islets or a violation of the compensatory mechanisms involved in the regulation of carbohydrate metabolism and in the inactivation of insulin.
Endocrine-dependent ketotic hypoglycemia (without increasing the level of insulin in the blood) is detected with a deficiency of counter-insulin hormones in patients with hypofunction of the anterior pituitary gland (cerebral-pituitary dwarfism, isolated GH deficiency, hypopituitarism), thyroid gland (hypothyroidism), and adrenal cortex (Addison's disease).
Without an increase in insulin levels, extrapancreatic hypoglycemia can occur, which occurs with extrapancreatic tumors (chest, abdominal cavity, retroperitoneal, etc.), hypoglycemia accompanying diffuse liver diseases, chronic renal failure. In children of the first year of life, the cause of ketotic non-endocrine-dependent hypoglycemia (without hyperinsulinism) is congenital enzymopathies (glycogenosis).
In clinical practice, reactive hypoglycemia is often encountered - functional hyperinsulinism with vegetative-vascular dystonia. They are observed in obese individuals, in neurotic children of preschool age against the background of acetonemic vomiting due to disruption of the processes of gluconeogenesis, etc.
Hypoglycemia of an exogenous nature (caused by the administration of insulin, hypoglycemic agents, salicylates, sulfonamides and other drugs) is also common.
With functional hyperinsulinism, hypoglycemia is clinically less pronounced, blood sugar does not fall below 2.2 mmol/l.
Hypoglycemia can be detected by clinical signs; more often, low blood sugar levels are a laboratory finding. Detection of hypoglycemia in the early morning hours or on an empty stomach before breakfast in capillary blood at least 2-3 times is considered reliable (in the absence of clear clinical data). The indication for examination in a hospital is a classic clinical picture of hyperinsulinism or three times confirmed morning hypoglycemia (without clinical manifestations) below age indicators (decrease in fasting glycemia for newborns - less than 1.67 mmol/l, 2 months - 18 years - less than 2.2 mmol/l , over 18 years old - less than 2.7 mmol/l).
Whipple's triad is pathognomonic for hypoglycemic disease:
- the occurrence of attacks of hypoglycemia after prolonged fasting or physical activity;
- a decrease in blood sugar during an attack below 1.7 mmol/l in children under 2 years of age, below 2.2 mmol/l in children over 2 years of age;
- relief of a hypoglycemic attack by intravenous administration of glucose or oral administration of glucose solutions.
Most symptoms of hypoglycemia are caused by insufficient glucose supply to the central nervous system. When glucose levels decrease to hypoglycemia, mechanisms aimed at glycogenolysis, gluconeogenesis, mobilization of free fatty acids, and ketogenesis are activated. These processes involve mainly 4 hormones: norepinephrine, glucagon, cortisol, growth hormone. The first group of symptoms is associated with an increase in the content of catecholamines in the blood, which causes weakness, tremors, tachycardia, sweating, anxiety, hunger, and pale skin. Symptoms from the central nervous system (symptoms of neuroglycopenia) include headache, double vision, behavioral disturbances (mental agitation, aggressiveness, negativism), followed by loss of consciousness, convulsions, and coma with hyporeflexia, shallow breathing, and muscle atony. Deep coma leads to death or irreversible damage to the central nervous system. Frequent attacks of hypoglycemia lead to personality changes in adults and decreased intelligence in children. The difference between the symptoms of hypoglycemia and real neurological conditions is the positive effect of food intake, the abundance of symptoms that do not fit into the clinic.
The presence of pronounced neuropsychiatric disorders and insufficient awareness of doctors about hypoglycemic conditions often lead to the fact that, due to diagnostic errors, patients with organic hyperinsulinism are treated for a long time and unsuccessfully under a variety of diagnoses. Erroneous diagnoses are made in 3/4 of patients with insulinoma (epilepsy is diagnosed in 34% of cases, brain tumor - in 15%, vegetative-vascular dystonia - in 11%, diencephalic syndrome - in 9%, psychosis, neurasthenia - 3% (Dizon A. M., 1999).
The period of acute hypoglycemia is the result of a breakdown of counterinsular factors and the adaptive properties of the central nervous system.
Most often, an attack develops in the early morning hours, which is associated with a long night break in eating. Typically, patients cannot “wake up” due to various kinds of disorders of consciousness. There may be lethargy and apathy in the morning. The epileptiform seizures observed in these patients differ from the true ones by their longer duration, chorioform convulsive twitching, hyperkinesis, and abundant neurovegetative symptoms. Recognition of the disease requires a thorough examination of the anamnesis and careful observation of patients. This is especially important for diagnosing organic hyperinsulinism as a cause of hypoglycemia in children.
In children of the first year of life, it is difficult to clinically detect hypoglycemia, since the symptoms are vague and atypical. This may be cyanosis, pallor of the skin, decreased muscle tone, respiratory arrest (apnea), tremors, convulsions, “rolling” of the eyeballs (nystagmus), anxiety. In the congenital form (nesidioblastosis), there is a large body weight (large fetus), swelling, and a round face.
In children of preschool and school age with organic hyperinsulinism, benign insulinoma is more often registered. These children are characterized by morning incapacity, difficulty waking up in the morning, impaired concentration, pronounced feelings of hunger, cravings for sweets, negativism, and palpitations. Hyperinsulinism leads to increased appetite and obesity. The younger the child, the greater the tendency for low blood sugar in response to longer intervals between meals.
Among the laboratory parameters for suspected organic hyperinsulinism (insulinoma or nesidioblastosis), a special place is occupied by the study of immunoreactive insulin (IRI). But, as practice has shown, proven insulinoma does not always have elevated values. IRI is usually assessed simultaneously with the glycemic level. An important index is the ratio of insulin to glucose - IRI mked/ml/venous glucose mmol/l. In healthy people and against the background of hypoglycemia without hyperinsulinism, this index is less than 5.4.
Among the functional tests used to diagnose organic hyperinsulinism, the most common is the fasting test.
The test is based on the development of hypoglycemia in people with hyperfunction of the pancreatic insular apparatus when the intake of carbohydrates from food is stopped. During the test, the patient is allowed to drink only water or tea without sugar. The younger the child and the more frequent the attacks of hypoglycemia, the shorter the test.
Test duration: children under 3 years old - 8 hours; 2 - 10 years - 12-16 hours; 10 - 18 years - 20 hours; over 18 years old - 72 hours (recommendations of the Department of Pediatric Endocrinology of the Russian Medical Academy of Postgraduate Education, Moscow).
For children 2 years of age and older, the last meal should be the night before; For children under 2 years of age, the test begins in the early morning hours.
In a healthy person, overnight or longer fasting moderately reduces the level of glycemia and, characteristically, reduces the level of insulin in the blood. In the presence of a tumor that constantly produces excess amounts of insulin, under starvation conditions, the prerequisites are created for the development of hypoglycemia, since there is no glucose supply from the intestine, and hepatic glycogenolysis is blocked by tumor insulin.
Before starting the test, the glucose content in the blood plasma is determined. Next, glycemia in capillary blood (with a glucometer) is examined in children under 2 years of age once an hour, in children aged 2 years and older - once every 2 hours. When blood sugar decreases to 3.3 mmol/l or less, the test intervals are reduced by 2-3 times. The threshold of acceptable glycemia, at which fasting is stopped and research is carried out, is 1.7 mmol/l in a child under 2 years old, 2.2 mmol/l in children over 2 years old. After threshold hypoglycemia is registered with a glucometer, the blood serum is examined for the content of IRI and counter-insulin hormones, blood glucose is examined using a biochemical method (since after the glucose level is reduced to 3.3 mmol/l and below, the glucometer gives an inaccurate result), and the level of blood lipids is examined.
An attack of hypoglycemia is stopped by administering 40% glucose intravenously; immediately after the administration of glucose and 3 hours after the end of the test, urine is examined for the content of ketone bodies.
Interpretation of sample results
- If acetone is not detected in the urine, then hypoglycemia is caused by hyperinsulinism (increased insulin suppresses the breakdown of fatty acids - lipolysis). The presence of acetonuria indicates the intensive formation of ketone bodies from fatty acids coming from fat depots. With hypoglycemia not associated with hyperproduction of insulin, lipolysis is turned on as an energy source, which leads to the formation of ketone bodies and the formation of positive acetone in the urine.
- With hyperinsulinism, the content of lipids in the blood is not changed or reduced; with ketotic hypoglycemia, the lipid level is increased.
- A decrease in the level of counter-insulin hormones is observed in endocrine-dependent ketotic hypoglycemia; with organic hyperinsulinism the indicators are not changed.
- The IRI/venous glycemia index in healthy children and against the background of hypoglycemia without hyperinsulinism was less than 5.4, whereas with organic hyperinsulinism this figure increases significantly.
If hyperinsulinism is confirmed as the cause of hypoglycemia, further examination and treatment in a specialized endocrinology department is necessary.
In all cases, surgical treatment is indicated with insulin. For nesidioblastosis, therapy can be conservative or radical. The drug diazoxide (proglycem, zaroxolin) has currently received the greatest recognition. The hyperglycemic effect of this non-diuretic benzothiazide is based on inhibition of insulin secretion from tumor cells. The recommended dose for children is 10 - 12 mg per kg of body weight per day in 2 - 3 doses. In the absence of pronounced positive dynamics, surgical treatment is indicated - subtotal or total resection of the pancreas (with possible transition to diabetes mellitus).
S. A. Stolyarova, T. N. Dubovaya, R. G. Garipov S. A. Malmberg, Doctor of Medical Sciences V. I. Shirokova, Candidate of Medical Sciences Children's Clinical Hospital No. 38 FU "Medbioextrem" under the Ministry of Health of the Russian Federation, Moscow
Patient Zakhar Z., 3 months. , was admitted to the Department of Psychoneurology of Children's Clinical Hospital No. 38 of the FU Medbioextrem in Moscow on November 1, 2002 with a referral diagnosis of epilepsy.
A child with a moderately burdened perinatal history. This was the mother’s first pregnancy and proceeded with toxicosis in the first half and anemia. Delivery at 40 weeks, large fetus (birth weight 4050 g, length 54 cm). Apgar score: 8/9 points. From the neonatal period to 2 months. tremor of the chin was periodically noted; from the age of 2 months, paroxysmal states appeared in the form of stopping gaze, decreased motor activity, twitching of the right half of the face, right hand (attacks of focal convulsions) - for several seconds 3-4 times a day. He was treated as an outpatient by a neurologist and received anticonvulsant therapy without a significant positive effect. On the eve of hospitalization, choreiform twitching appeared in the morning against the background of impaired consciousness. Hospitalized in the department of psychoneurology with a referral diagnosis of epilepsy.
Upon admission, the child's condition was moderate. In the somatic status - the skin has manifestations of atopic dermatitis, the pharynx is clean, there are no wheezes in the lungs, heart sounds are sonorous, tachycardia up to 140 - 160 beats. per minute The abdomen is soft, liver +2 cm, spleen +1 cm. Urination is not impaired. In neurological status - lethargic, fixed gaze, poor head support. CN - intact, muscle tone is reduced, more in the arms, symmetrical. Tendon reflexes are low, D = C, unconditioned reflexes are low - according to age. Weight - 7 kg, height - 61 cm (excess weight is noted against the background of the average age growth rate).
In the hospital, a biochemical fasting blood test revealed for the first time a decrease in blood sugar to 1.6 mmol/l in the absence of ketone bodies in the urine.
Results of laboratory and instrumental examination:
- Oculist - no pathology was detected in the fundus.
- ECG - heart rate 140, sinus rhythm, vertical position of the EOS.
- Allergist - atopic dermatitis, common form, mild course.
- Ultrasound of the abdominal organs - the pancreas is not clearly visualized in its typical location. Ultrasound of the adrenal glands - no changes. Ultrasound of the kidneys - reactive changes in the walls of the jaw, Fraley syndrome on the left, pyelectasis on the left cannot be excluded. Spleen - moderate splenomegaly.
- General blood test - Hb 129 g/l, er - 5.08 million, l - 8.7 thousand, ESR - 3 mm/hour.
- General urine analysis - protein, sugar, acetone - neg., L - 2 - 3 in the field of vision, er - 0 - 1 in the field of view.
- Blood biochemistry (upon admission) - total protein. - 60.5 g/l, ALT - 20.2 g/l, AST - 66.9 g/l, bilirubin total. - 3.61 µmol/l, glucose - 1.6 mmol/l, creatinine - 36.8 µmol/l, urea - 1.88 mmol/l, total cholesterol. — 4.44 mmol/l, iron total. - 31.92 µmol/l, potassium - 4.9 mmol/l, sodium - 140.0 mmol/l.
Dynamic monitoring of glucose levels revealed persistent hypoglycemia in capillary and venous blood. On an empty stomach and 2 hours after feeding with breast milk during the day, glycemia ranged from 0.96 to 3.2 mmol/l. Clinically, hypoglycemia was manifested by increased appetite, lethargy, tachycardia, episodes of “rolling” of the right eyeball, and generalized epileptiform convulsions. During the interictal period, the state of health is satisfactory. Hypoglycemic conditions were relieved by oral glucose intake, as well as intravenous administration of 10% glucose.
For diagnostic purposes, to confirm hyperinsulinism, the child underwent a fasting test: the last night feeding at 6 a.m., before feeding, glycemia was 2.8 mmol/l, 3.5 hours after feeding, the glucometer showed a decrease in glycemia to 1.5 mmol/l (below the acceptable threshold). Against the background of hypoglycemia, blood serum was taken for hormonal studies (IRI, c-peptide, cortisol, STH). Venous blood was collected for biochemical testing of glucose and lipid levels. After relief of hypoglycemia with intravenous injection of glucose, a three-hour portion of urine was collected for the content of ketone bodies.
Test results: no acetonuria. The level of counter-insulin hormones is not reduced (cortisol - 363.6 when the norm is 171 - 536 nmol/l, STH - 2.2 when the norm is 2.6 - 24.9 µU/ml). C-peptide - 0.53 at a normal level of 0.36 - 1.7 pmol/l. IRI - 19.64 with normal - 2.6 - 24.9 mmkE/ml. Venous glucose - 0.96 mmol/l. Blood lipid levels are at the lower limit of normal (triglycerides - 0.4 mmol/l, total cholesterol - 2.91 mmol/l, high-density lipoprotein cholesterol - 1.06 mmol/l, low-density lipoprotein cholesterol - 1.06 mmol/l - 1.67 mmol/l. IRI/glucose index (19.64 /0.96) was 20.45, with the norm being less than 5.4.
Data from the anamnesis, dynamic observation, and clinical and laboratory examination allowed us to make a diagnosis: non-ketotic hypoglycemia. Hyperinsulinism. Nesidioblastosis?
To clarify the genesis of the disease and treatment tactics, the child was transferred to the endocrinology department of the Russian Children's Clinical Hospital in Moscow, where insulinoma was ruled out in the boy. The diagnosis of nesidioblastosis was confirmed. A trial of conservative treatment with proglycem at a dose of 10 mg per kg of body weight was prescribed. There was a tendency towards normalization of carbohydrate metabolism indicators. Further follow-up is planned to adjust treatment tactics.
The considered clinical case dictates the need to study the parameters of carbohydrate metabolism in all young children with convulsive syndrome, due to the erasure of the clinical symptoms of hypoglycemia in infants and young children, in order to exclude diagnostic errors.
What is the prognosis for treatment?
With proper and well-chosen treatment, the prognosis is favorable.
There are different types of insulin. Many children use insulin pump therapy. But it is important to know that much here depends not on the treatment, but on how the child and his parents perceive the diagnosis and how they treat it. They will have to learn a lot. The first thing is to streamline your diet
and lifestyle. Please note that the diet does not change completely, it just becomes correct. And this is not just eating chips, chocolates and sandwiches.
Secondly, in childhood diabetes mellitus, blood glucose control
. Children do this often: optimally 6–8 times a day. There are now many different means to control blood glucose. First of all, these are glucometers, when for each measurement of glucose in the blood the child needs to prick his finger. But now there are systems where a sensor is placed in children for two weeks (for example, in the shoulder area). And with a special device (scanner) you can determine blood glucose every minute by bringing this scanner to the sensor. And then you don’t need to prick your fingers 6–8 times a day.
Is a full life possible, and why will you have to give up forever? And our children live full lives
. Participate in various competitions and competitions. I would say, on the contrary, they are smarter and more capable than children without diabetes. Probably because they had to grow up earlier. Learn to lead a healthy lifestyle, eat right, and maintain a proper daily routine. They count bread units (this is the amount of carbohydrates) in order to correctly inject themselves with the required dose of insulin.
However, children with diabetes and their parents should be aware that they will be faced with the difficult question of choosing a profession. The fact is that some professions are contraindicated for diabetes:
- with heavy physical activity (miners);
- with significant neuropsychological stress (air traffic controllers, transport drivers);
- with irregular working hours, at night, with an unfavorable microclimate, with contact with toxic substances (chemical production).
How to proceed
Once the test results are confirmed, the pediatrician will refer you to an endocrinologist. Treatment begins with selecting an effective dosage of insulin.
The little patient is prescribed a low-carbohydrate diet and regular blood tests for grape sugar levels. Parents are taught to monitor portion size, food quality, control sugar using a glucometer, and the method of administering insulin.
Scrupulous adherence to the doctor’s recommendations will compensate for impaired insulin production and avoid the development of complications.
Without treatment, the child will begin to lag behind his peers in growth and mental development, vision problems, neurological and vascular pathologies will appear.