Release form
Tritace Plus is available in tablet form.
5 + 12.5
The tablets are oblong, pink in color, and have a dividing line on each side. At the top there is a stamp 41/AV. Single dark inclusions are allowed.
10 + 12.5
The tablets are oblong, orange in color, with a dividing line on both sides. At the top there is a stamp 42/AY. Single dark inclusions are allowed.
5 + 25
Tablets are almost white, cream-colored with a dividing line, oblong in shape. There is a company logo and HNW stamp on both sides.
10 + 25
Pink tablets, oblong in shape. There is a dividing line on both sides. Stamped 39/AV on top. Single dark specks are allowed.
pharmachologic effect
Combined antihypertensive drug , which includes 2 active components.
Ramipril
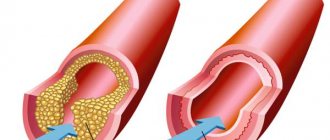
The active ingredient is an ACE enzyme inhibitor . The principle of action is based on preventing the transition of one form of angiotensin (I) to another (II).
In this case, there is no increase in heart rate through a compensatory mechanism; The production of aldosterone , the level of pressure in the capillaries of the pulmonary system does not change, the coronary blood supply , the filtration rate in the glomeruli of the renal system does not change, and the resistance in the vessels of the pulmonary system remains at the original level.
Clinical studies have shown that long-term therapy leads to a decrease in the severity of hypertrophy in the myocardium in patients suffering from hypertension . In ischemic myocardium, Ramipril increases blood circulation, reduces the frequency of myocardial reperfusion and the risk of arrhythmia .
The cardioprotective (heart + protection) effect is achieved by influencing the process of prostaglandin , as well as by inducing the formation of nitric oxide in endothelial cells. The active component is able to reduce platelet aggregation.
Hydrochlorothiazide
The active component is a thiazide diuretic and is capable of changing the reabsorption of potassium, chlorine, sodium, and magnesium ions. The active substance retains uric acid in the body, slows down the process of excretion of calcium ions, and changes the reabsorption of water in the nephrons (distal section).
The hypotensive effect is achieved by enhancing the depressor effect on the ganglia, reducing the severity of the pressor effect of norepinephrine , adrenaline and other vasoconstrictor amines; due to a decrease in the BCC indicator. With normal blood pressure, the hypotensive effect is not observed.
Ramipril and Hydrochlorothiazide are characterized by an additive effect. Hydrochlorothiazide flushes potassium from the body, and Ramipril neutralizes this effect, preventing the loss of K+.
Tritace® plus
The simultaneous use of Tritace® plus with drugs containing aliskiren or with angiotensin II receptor antagonists, leading to double blockade of the RAAS, is not recommended due to the risk of an excessive decrease in blood pressure, the development of hyperkalemia and deterioration of renal function.
The simultaneous use of Tritace® plus with drugs containing aliskiren in patients with diabetes mellitus and/or renal failure with a creatinine clearance <60 ml/min is contraindicated (see sections “Contraindications” and “Interaction with other drugs”).
Concomitant use with angiotensin II receptor antagonists in patients with diabetic nephropathy is contraindicated (see sections “Contraindications” and “Interaction with other drugs”).
Angioedema of the face, neck or limbs
(see section "Side effects").
During treatment with ACE inhibitors, mainly after taking the first dose, cases of angioedema have been observed. If angioedema develops during treatment with an ACE inhibitor, immediate cessation of its use is required.
Since angioedema involving the larynx can be fatal, in the event of swelling of the face, extremities, lips, tongue or vocal cords and, especially, the development of stridor breathing, you should immediately stop taking Tritace® plus and immediately begin treatment aimed at relieving the angioedema swelling. In cases where the swelling is localized to the face and lips, the condition usually resolves without treatment, although antihistamines may be used to relieve symptoms.
If swelling spreads to the tongue, vocal cords or pharynx, airway obstruction is possible, in such cases it is necessary to immediately begin appropriate treatment (including immediate subcutaneous or slow intravenous administration of epinephrine (adrenaline) under ECG and blood pressure monitoring). It is recommended to hospitalize for at least 12-24 hours and discharge from the hospital only after complete relief of the symptoms of angioedema
Angioedema of the small intestine
In patients receiving ACE inhibitors, the development of angioedema of the small intestine, which was manifested by abdominal pain (with or without nausea or vomiting), was reported, and in some cases angioedema of the face was simultaneously observed. The diagnosis is made using computed tomography of the abdominal cavity, ultrasound, or at the time of surgery. Symptoms of intestinal angioedema resolved after discontinuation of the ACE inhibitor.
Acute myopia and secondary acute angle-closure glaucoma
Hydrochlorothiazide is a sulfonamide derivative. Sulfonamide and sulfonamide derivatives can cause idiosyncratic reactions leading to the development of transient myopia and acute angle-closure glaucoma, the symptoms of which are acute decrease in visual acuity or eye pain. They usually occur within a few hours to several weeks after starting the drug. If left untreated, acute angle-closure glaucoma can lead to permanent vision loss. It is necessary to stop taking the drug as soon as possible. Urgent medical or surgical treatment may be required if intraocular pressure remains uncontrolled. Risk factors for the development of acute myopia or secondary angle-closure glaucoma are anamnestic indications of an allergy to sulfonamide derivatives or penicillins.
Cough
When taking Tritace® plus, a “dry” cough may occur, which usually disappears after discontinuation of the drug. This possibility must be taken into account when making a differential diagnosis of cough (see section “Side effects”).
Anaphylactoid reactions to ACE inhibitors
Life-threatening, rapid-onset anaphylactoid reactions, sometimes leading to shock, have been described with ACE inhibitors during hemodialysis using certain high-flux membranes (eg, polyacrylonitrile membranes) (see also membrane manufacturer's instructions).
The combined use of Tritace® plus and this type of membrane should be avoided, for example, for urgent hemodialysis or hemofiltration. In this case, it is preferable to use other types of membranes or avoid taking ACE inhibitors.
Similar reactions were observed with low-density lipoprotein apheresis using dextran sulfate. These reactions were avoided by temporarily stopping ACE inhibitor therapy before each apheresis.
Antihistamines are ineffective for treating these reactions.
There have been isolated reports of patients with prolonged life-threatening anaphylactoid reactions that occurred during desensitizing treatment with venom from bees, wasps, etc. In some patients, these reactions were avoided by preliminary temporary withdrawal of ACE inhibitors for a period of at least 24 hours.
Hypersensitivity reactions to hydrochlorothiazide do not depend on a history of allergies or bronchial asthma.
Excessive decrease in blood pressure
After using ramipril, usually after the first or second dose, or after increasing the dose, an excessive decrease in blood pressure is possible, which is most likely in patients whose circulating blood volume has been reduced as a result of diuretic therapy, limited intake of sodium chloride from food, dialysis, diarrhea, vomiting or excessive sweating.
It is generally recommended that dehydration, hypovolemia and hyponatremia be corrected before starting the drug (however, in patients with heart failure, volume replacement should be carried out with great caution, as there is a risk of decompensation due to excessive volume load). A transient excessive decrease in blood pressure is not a contraindication for continuing treatment after stabilization of blood pressure. In case of repeated excessive decrease in blood pressure, the dose should be reduced or the drug discontinued.
Patients with RAAS activation
In conditions in which the RAAS is activated and/or renal function depends on its activity (see section "Precautions"), with ACE inhibition there is an increased risk of a pronounced decrease in blood pressure and impaired renal function. Therefore, in such cases, at the beginning of treatment or at the beginning of an increase in the initially taken dose, careful monitoring of blood pressure is required until a further decrease in blood pressure is no longer expected.
In patients with severe heart failure (including those accompanied by renal failure), therapy with an ACE inhibitor may cause an excessive decrease in blood pressure and be accompanied by oliguria and (or) progressive azotemia with acute renal failure, including death. In such patients, initiation or continuation of treatment with Tritace® plus should be carried out only after taking measures against a sharp decrease in blood pressure and deterioration of renal function.
Patients for whom an excessive decrease in blood pressure is particularly dangerous
An excessive decrease in blood pressure is especially dangerous for patients with coronary heart disease or severe cerebral atherosclerosis, since in this case the development of myocardial infarction or stroke is possible (see section “With caution”). Such patients are subject to strict monitoring at the beginning of treatment and when increasing the dose of the drug.
Patients with dehydration
All patients should be warned that dehydration due to increased sweating (including during hot weather or physical activity), vomiting, diarrhea can lead to an excessive decrease in blood pressure, and in these cases the question of the dose of ramipril and hydrochlorothiazide used should be decided by a doctor .
Alcohol (ethanol) intake during treatment with Tritace® plus
During treatment with Tritace® plus, it is not recommended to drink alcohol (ethanol) (see section “Interaction with other drugs”).
In case of an excessive decrease in blood pressure, it is necessary to place the patient with his legs elevated, and, if necessary, begin an intravenous infusion of 0.9% sodium chloride solution to replenish the bcc (circulating blood volume).
Surgery and anesthesia
Before surgical interventions (including dental), it is necessary to warn the surgeon/anesthesiologist about taking ACE inhibitors. If an excessive decrease in blood pressure occurs during anesthesia, it can be corrected by replenishing the blood volume.
Thiazide diuretics may enhance the effects of tubocurarine. It is recommended that treatment with ACE inhibitors, including ramipril, be discontinued (if possible) one day before surgery.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism usually do not respond to antihypertensive drugs that act through inhibition of the RAAS. Therefore, Tritace® plus is not the drug of choice for the treatment of primary hyperaldosteronism.
Monitoring hematological parameters
When taking Tritace® plus, it is recommended to monitor the number of leukocytes to detect possible leukopenia. Regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, connective tissue diseases (systemic lupus erythematosus, scleroderma) or in patients receiving other drugs that can change the peripheral blood picture (see sections “Side effects”, “Interaction with other medicines").
If symptoms due to leukopenia appear (for example, fever, enlarged lymph nodes, tonsillitis), urgent monitoring of the peripheral blood picture is necessary. If signs of bleeding appear (tiny petechiae, red-brown rashes on the skin and mucous membranes), monitoring the number of platelets in the peripheral blood is also necessary.
Monitoring liver function
A complete liver function test and other liver tests should be performed if patients develop the following symptoms suggestive of liver dysfunction: flu-like symptoms occurring in the first weeks or months of treatment (such as fever, malaise, muscle pain, skin rash, or adenopathy indicating reactions hypersensitivity), abdominal pain, nausea or vomiting, loss of appetite, jaundice, itching or other unexplained symptoms. If liver dysfunction is confirmed, you should stop taking Tritace® plus and, if necessary, prescribe appropriate treatment.
In patients with impaired liver function or with progressive liver diseases, the use of thiazide diuretics requires caution, since in such patients even minimal disturbances in water and electrolyte balance can provoke the development of hepatic coma. There are no controlled clinical studies in patients with cirrhosis and/or liver dysfunction. Tritace® plus should be used with extreme caution in patients with pre-existing liver dysfunction, who should determine the state of liver function before starting the drug and regularly monitor it during treatment.
Monitoring kidney function
Due to suppression of the RAAS, renal function may deteriorate in predisposed patients; this risk increases with the simultaneous use of diuretics.
It is recommended to carefully monitor renal function in the first weeks of treatment and thereafter, especially in the following groups of patients:
— patients with heart failure;
- patients with renovascular diseases, including hemodynamically significant unilateral renal artery stenosis (in such patients, even a slight increase in serum creatinine concentrations may be a manifestation of a unilateral decrease in renal function);
— patients with impaired renal function;
— patients after kidney transplantation.
In patients with renal failure, special caution is required when treating with Tritace® plus, and in these cases lower doses of the drug are used (see section "Dosage and Administration").
Hydrochlorothiazide may promote or worsen azotemia. Cumulative effects of the drug are possible in patients with impaired renal function. If increasing azotemia and oliguria develop during treatment of severe progressive kidney disease, diuretic therapy should be discontinued. Insufficient experience has been gained with the use of Tritace® plus in patients with severe renal impairment (creatinine clearance less than 30 ml/min per 1.73 m2 body surface area) and in patients on hemodialysis. Monitoring electrolytes and serum glucose concentrations
Treatment with Tritace® plus requires regular monitoring of serum sodium, potassium, calcium, uric acid and blood glucose levels.
Patients with impaired renal function and impaired water and electrolyte balance require regular monitoring of potassium levels in the blood serum.
Other Cautions
Thiazide diuretics can reduce blood concentrations of protein-bound iodine without causing signs of thyroid dysfunction. Thiazide diuretics may cause a transient and small increase in serum calcium in the absence of known disorders of calcium metabolism. Severe hypercalcemia may indicate latent hyperparathyroidism. Before assessing parathyroid function, thiazide diuretics should be discontinued.
Risk factors for the development of hyperkalemia include renal failure, diabetes mellitus, and concomitant use of drugs to treat hypokalemia or other drugs that can increase serum potassium levels (see section “Interaction with other drugs”). Patients should be cautioned not to use salt substitutes containing potassium without first consulting their healthcare provider.
It should be taken into account that when using hydrochlorothiazide, a positive doping control is possible.
Pharmacodynamics and pharmacokinetics
The hypotensive effect of Ramipril is recorded 90 minutes after taking the tablet, and the maximum result is observed after 5-9 hours. The effect lasts throughout the day. Upon completion of therapy, the “withdrawal” syndrome does not form. The diuretic effect of Hydrochlorothiazide appears after 1-2 hours.
The maximum result is observed after 4 hours and can last up to 12 hours. The antihypertensive effect is observed after 3-4 days, but the optimal therapeutic effect can be achieved only after 3-4 weeks.
Pharmacodynamics
The active metabolite of ramipril, ramiprilat, formed under the influence of liver enzymes, is a long-acting ACE inhibitor, which is a peptidyl dipeptidase. ACE in blood plasma and tissues catalyzes the conversion of angiotensin I to angiotensin II and the breakdown of bradykinin.
Therefore, when ramipril is taken orally, the formation of angiotensin II decreases and bradykinin accumulates, which leads to vasodilation and a decrease in blood pressure. An increase in the activity of the kallikrein-kinin system in the blood and tissues determines the cardioprotective and endothelial-protective effects of ramipril due to the activation of the prostaglandin system and, accordingly, an increase in the synthesis of PGs that stimulate the formation of nitric oxide (NO) in endothelial cells.
Angiotensin II stimulates the production of aldosterone, so taking ramipril leads to a decrease in aldosterone secretion and an increase in serum concentrations of potassium ions.
By reducing the concentration of angiotensin II in the blood, its inhibitory effect on renin secretion by negative feedback is eliminated, which leads to an increase in plasma renin activity.
It is assumed that the development of some undesirable reactions (in particular, “dry” cough) is also associated with an increase in the concentration of bradykinin.
In patients with arterial hypertension, taking ramipril leads to a decrease in blood pressure in the supine and standing positions, without a compensatory increase in heart rate. Ramipril significantly reduces peripheral vascular resistance, causing virtually no changes in renal blood flow and glomerular filtration rate. The hypotensive effect begins to appear 1–2 hours after oral administration of a single dose of the drug, reaching its greatest value after 3–9 hours, and persists for 24 hours. With a course of administration, the hypotensive effect can gradually increase, usually stabilizing by 3–4 weeks of regular use drug and then persisting for a long time. Sudden discontinuation of the drug does not lead to a rapid and significant increase in blood pressure (no withdrawal syndrome).
In patients with arterial hypertension, ramipril slows down the development and progression of myocardial and vascular wall hypertrophy.
In patients with chronic heart failure, ramipril reduces peripheral vascular resistance (reducing afterload on the heart), increases venous capacity and reduces left ventricular filling pressure, which, accordingly, leads to a decrease in preload on the heart. In these patients, when taking ramipril, there is an increase in cardiac output, ejection fraction and improved exercise tolerance.
In diabetic and non-diabetic nephropathy, taking ramipril slows down the rate of progression of renal failure and the time of onset of end-stage renal failure and, thereby, reduces the need for hemodialysis or kidney transplantation. In the initial stages of diabetic or non-diabetic nephropathy, ramipril reduces the severity of albuminuria.
In patients at high risk of developing cardiovascular disease due to the presence of vascular lesions (diagnosed coronary artery disease, history of peripheral arterial occlusive disease, history of stroke) or diabetes mellitus with at least one additional risk factor (microalbuminuria, arterial hypertension, increased concentrations total cholesterol (TC), lowering concentrations of high-density lipoprotein cholesterol (HDL-C, smoking), adding ramipril to standard therapy significantly reduces the incidence of myocardial infarction, stroke and mortality from cardiovascular causes. In addition, ramipril reduces overall mortality, and also the need for revascularization procedures, and slows the onset or progression of chronic heart failure.
In patients with heart failure that developed in the first days of acute myocardial infarction (2–9 days), when taking ramipril, starting from 3 to 10 days of acute myocardial infarction, the risk of mortality is reduced (by 27%), the risk of sudden death (by 30%). ), the risk of progression of chronic heart failure to severe (III–IV functional class according to the NYHA classification)/resistant to therapy (by 27%), the likelihood of subsequent hospitalization due to the development of heart failure (by 26%).
In the general patient population, as well as in patients with diabetes mellitus, both arterial hypertension and normal blood pressure, ramipril significantly reduces the risk of developing nephropathy and microalbuminuria.
Contraindications
- renal artery stenosis (bilateral);
- angioedema;
- individual hypersensitivity;
- mitral stenosis with hemodynamically significant changes;
- primary hyperaldosteronism;
- pregnancy;
- stenosis of the renal arteries with a solitary kidney;
- breast-feeding;
- condition after kidney transplantation;
- aortic stenosis with hemodynamically significant changes;
- hemodialysis , which uses AN69 type dialysis membranes;
- hyponatremia;
- hypercalcemia;
- gout;
- pathology of the renal system;
- diabetes mellitus (severe);
- hypokalemia (refractory form).
Relative contraindications:
- severe damage to the cerebral and coronary arteries (with a sharp drop in blood pressure, blood flow may be disrupted);
- ventricular arrhythmias;
- hyponatremia;
- liver failure;
- heart failure;
- unstable form of angina;
- “pulmonary heart” (decompensation);
- hyperkalemia;
- renal failure;
- elderly age;
- vomiting, diarrhea syndrome and other conditions accompanied by a decrease in blood volume;
- inhibition of bone marrow circulation;
- systemic pathology of connective tissue;
- IHD;
- hypercalcemia;
- hepatic cirrhosis;
- diabetes.
Tritatse in Moscow
Before starting treatment with Tritace®, hyponatremia and hypovolemia must be eliminated. In patients who have previously taken diuretics, it is necessary to discontinue them or at least reduce their dose 2-3 days before starting Tritace® (in this case, the condition of patients with chronic heart failure should be carefully monitored, due to the possibility of developing them decompensation with an increase in blood volume).
After taking the first dose of the drug, as well as when increasing its dose and/or the dose of diuretics (especially loop diuretics), it is necessary to ensure careful medical monitoring of the patient for at least 8 hours in order to timely take appropriate measures in case of an excessive decrease in blood pressure.
If Tritace® is used for the first time or at a high dose in patients with increased activity of the renin-angiotensin-aldesterone system (RAAS), their blood pressure should be carefully monitored, especially at the beginning of treatment, because these patients have an increased risk of excessive reduction in blood pressure (see section "Precautions").
In case of malignant arterial hypertension and heart failure, especially in the acute stage of myocardial infarction, treatment with Tritace® should only be started in a hospital setting.
In patients with chronic heart failure, taking the drug can lead to the development of a pronounced decrease in blood pressure, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure.
Caution should be exercised when treating elderly patients, because they may be particularly sensitive to ACE inhibitors; in the initial phase of treatment, it is recommended to monitor renal function indicators (see also section “Method of administration and dosage”).
In patients for whom a decrease in blood pressure may pose a certain risk (for example, in patients with atherosclerotic narrowing of the coronary or cerebral arteries), treatment should begin under strict medical supervision.
Caution should be exercised during physical activity and/or hot weather due to the risk of increased sweating and dehydration with the development of arterial hypotension due to a decrease in blood volume and a decrease in sodium concentration in the blood.
It is not recommended to drink alcohol during treatment with Tritace®.
Transient arterial hypotension is not a contraindication for continuing treatment after stabilization of blood pressure. If severe arterial hypotension reoccurs, the dose should be reduced or the drug discontinued.
Cases of angioedema of the face, extremities, lips, tongue, pharynx or larynx have been observed in patients treated with ACE inhibitors. If swelling occurs in the face (lips, eyelids) or tongue, or difficulty swallowing or breathing, the patient should immediately stop taking the drug. Angioedema, localized in the area of the tongue, pharynx, or larynx (possible symptoms: difficulty swallowing or breathing), can be life-threatening and requires urgent measures to relieve it: subcutaneous administration of 0.3–0.5 mg or intravenous drip 0. 1 mg of epinephrine (under the control of blood pressure, heart rate and ECG) followed by the use of corticosteroids (iv, intramuscular, or orally); Intravenous administration of antihistamines (H1- and H2-histamine receptor antagonists) is also recommended. The patient should be hospitalized and monitored until symptoms are completely relieved, but not less than 24 hours.
Cases of intestinal angioedema, manifested by abdominal pain with or without nausea and vomiting, have been observed in patients receiving ACE inhibitors; in some cases, angioedema of the face was simultaneously observed. If a patient develops the symptoms described above during treatment with ACE inhibitors, the possibility of developing intestinal angioedema should be considered when making a differential diagnosis.
Treatment aimed at desensitization to insect venom (bees, wasps) and concomitant use of ACE inhibitors can initiate anaphylactic and anaphylactoid reactions (for example, decreased blood pressure, shortness of breath, vomiting, allergic skin reactions), which can sometimes be life-threatening. During treatment with ACE inhibitors, hypersensitivity reactions to insect venom (for example, bees, wasps) develop faster and are more severe. If desensitization to insect venom is necessary, the ACE inhibitor should be temporarily replaced with an appropriate drug of a different class.
Life-threatening, rapidly developing anaphylactoid reactions, sometimes leading to shock, have been described with the use of ACE inhibitors during hemodialysis or plasma filtration using certain high-flux membranes (for example, polyacrylonitrile membranes) (see also membrane manufacturer's instructions). The combined use of Tritace® and this type of membrane (for example, for urgent hemodialysis or hemofiltration) should be avoided. In this case, it is preferable to use other membranes or avoid taking ACE inhibitors. Similar reactions were observed with LDL apheresis using dextran sulfate. Therefore, this method should not be used in patients receiving ACE inhibitors.
In patients with impaired liver function, the response to treatment with Tritace® may be either enhanced or weakened. In addition, in patients with severe liver cirrhosis with edema and/or ascites, significant activation of the RAAS is possible, so special care should be taken when treating these patients (see also section "Dosage and Administration").
Before surgery (including dental surgery), it is necessary to warn the surgeon/anesthesiologist about the use of ACE inhibitors.
It is recommended to closely monitor neonates exposed in utero to ACE inhibitors for hypotension, oliguria, and hyperkalemia. In oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictors. These neonates are at risk of developing oliguria and neurological disorders, possibly due to decreased renal and cerebral blood flow due to the decrease in blood pressure caused by ACE inhibitors.
Monitoring laboratory parameters before and during treatment with Tritace® (up to 1 time per month in the first 3–6 months of treatment)
Monitoring kidney function (determining serum creatinine concentrations)
When treating with ACE inhibitors, it is recommended to monitor renal function in the first weeks of treatment and subsequently. Particularly careful monitoring is required in patients with acute and chronic heart failure, impaired renal function, after kidney transplantation, patients with renovascular diseases, including patients with hemodynamically significant unilateral renal artery stenosis in the presence of two kidneys (in such patients, even a slight increase in serum creatinine concentration may be indicator of decreased kidney function).
Electrolyte concentration monitoring
Regular monitoring of serum potassium concentration is recommended. Particularly careful monitoring of potassium concentration in the blood serum is required for patients with impaired renal function, significant disturbances in water and electrolyte balance, and chronic heart failure.
Monitoring hematological parameters (hemoglobin concentration, number of leukocytes, erythrocytes, platelets, leukocyte formula)
It is recommended to monitor the complete blood count to identify possible leukopenia. More regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, as well as in patients with connective tissue diseases or in patients simultaneously receiving other drugs that can change the peripheral blood picture (see section "Interactions"). Monitoring the number of leukocytes is necessary for the early detection of leukopenia, which is especially important in patients with an increased risk of its development, as well as at the first signs of infection. If neutropenia is detected (the number of neutrophils is less than 2000/μl), discontinuation of treatment with ACE inhibitors is required.
If symptoms due to leukopenia appear (for example, fever, enlarged lymph nodes, tonsillitis), urgent monitoring of the peripheral blood picture is necessary. If signs of bleeding appear (tiny petechiae, red-brown rashes on the skin and mucous membranes), monitoring the number of platelets in the peripheral blood is also necessary.
Determination of liver enzyme activity, bilirubin concentration in the blood
If jaundice or a significant increase in the activity of liver enzymes occurs, treatment with Tritace® should be discontinued and the patient should be monitored by a doctor.
Impact on the ability to drive a car and engage in other potentially hazardous activities.
During treatment with Tritace®, it is necessary to refrain from engaging in potentially hazardous activities, including driving a car, that require increased concentration and speed of psychomotor reactions, because While taking it, you may experience dizziness, decreased speed of psychomotor reactions, and decreased attention, especially after taking the first dose.
Side effects
The cardiovascular system:
- arrhythmia;
- drop in blood pressure;
- orthostatic form of hypotension;
- tachycardia;
- myocardial infarction;
- angina pectoris.
Genitourinary tract:
- decreased libido;
- proteinuria;
- decreased diuresis;
- increased severity of symptoms of renal failure.
Nervous system:
- nervous excitability;
- ischemic changes in the brain;
- dizziness;
- weakness;
- paresthesia;
- increased drowsiness;
- anxiety;
- anxiety;
- sleep disorders, insomnia;
- emotional instability;
- fainting;
- confusion;
- depressed mood;
- limb tremors.
Sense organs:
- change in taste perception;
- visual disturbances;
- vestibular disorders;
- noise in ears.
Digestive tract:
- thirst;
- vomit;
- diarrhea syndrome;
- nausea;
- stomatitis;
- glossitis;
- dry mouth;
- constipation;
- epigastric pain;
- cholestatic jaundice;
- intestinal obstruction;
- hepatitis;
- loss of appetite.
Respiratory system:
- bronchospasm;
- dry non-productive cough;
- sinusitis;
- rhinitis;
- dyspnea;
- rhinorrhea;
- bronchitis.
Allergic responses:
- angioedema of the tongue, lips, laryngopharynx or on the facial part of the head;
- skin rashes;
- angioedema of the extremities;
- serositis;
- pemphigus;
- Lyell's syndrome;
- photosensitivity;
- vasculitis;
- exfoliative dermatitis;
- skin itching;
- hives;
- myositis;
- arthritis;
- onycholysis;
- eosinophilia.
Blood-forming organs:
- pancytopenia;
- decrease in hemoglobin;
- agranulocytosis;
- thrombocytopenia;
- hemolytic anemia;
- erythropenia.
Possible effect on the fetus:
- deformation of the skull bones;
- hyperkalemia;
- detection of antinuclear antibodies;
- hyponatremia;
- limb contracture;
- hyperazotemia;
- changes in the functioning of the renal system;
- drop in blood pressure;
- oligohydramnios;
- hypoplasia of the skull bones.
Laboratory reactions:
- detection of antinuclear antibodies;
- hyperkalemia;
- hyperazotemia;
- hypercreatininemia;
- hyperbilirubinemia;
- increase in ALT, AST, bilirubin .
Other reactions:
- hyperthermia;
- convulsions;
- increased sweating;
- alopecia.
Negative reactions characteristic of Hydrochlorothiazide:
- arrhythmia;
- irritability;
- confusion;
- lability of psyche and mood;
- hypochloremic alkalosis;
- diarrhea syndrome;
- cholecystitis;
- tachycardia;
- anemia (aplastic, hemolytic);
- orthostatic hypotension;
- epigastric pain;
- sialadenitis;
- pancreatitis;
- anorexia;
- hyperuricemia;
- hyperglycemia;
- exacerbation of gout;
- necrotizing vasculitis;
- skin rashes;
- pneumonitis;
- pulmonary edema of non-cardiogenic origin.
Indications for Tritace®
essential hypertension;
chronic heart failure (as part of combination therapy, in particular in combination with diuretics);
diabetic or non-diabetic nephropathy, preclinical and clinically pronounced stages, incl. with severe proteinuria, especially when combined with arterial hypertension;
Reducing the risk of myocardial infarction, stroke or cardiovascular mortality in patients at high cardiovascular risk:
- in patients with confirmed coronary artery disease, a history of myocardial infarction or without it, including patients who have undergone percutaneous transluminal coronary angioplasty, coronary artery bypass grafting;
- in patients with a history of stroke;
- in patients with occlusive lesions of peripheral arteries;
- in patients with diabetes mellitus with at least one additional risk factor (microalbuminuria, arterial hypertension, increased plasma concentrations of TC, decreased plasma concentrations of HDL-C, smoking);
heart failure that developed during the first few days (2–9 days) after acute myocardial infarction (see section “Pharmacodynamics”).
Instructions for Tritace Plus (Method and dosage)
Dosing is carried out taking into account individual characteristics. Recommended time of administration is morning hours. A maximum of 2 tablets per day at a dose of 5+25 or 4 tablets at a dose of 2.5+12.5 is allowed, which corresponds to 50 mg of Hydrochlorothiazide and 10 mg of Ramipril.
If you miss a dose, try to take it as quickly as possible. Doubling the dose on your own is not allowed. The tablets must be washed down with water; breaking and chewing are not allowed. Eating does not affect the severity of the therapeutic effect of Tritace Plus.
Instructions for use TRITACE®
Prescribed internally.
It is recommended to take Tritace® every day at the same time of day.
Tritace® is taken with plenty of liquid, regardless of food intake. Food intake does not have a significant effect on the absorption of the active component of ramipril. The tablets must be swallowed whole (unchewed).
Adults
Patients treated with diuretics
Initiation of Tritace® may be accompanied by hypotension; this is more common in patients treated with diuretics.
The lack of salts and fluid in the body must be pre-corrected before starting Tritace® treatment; diuretics should be previously limited or discontinued, no later than 2-3 days.
Treatment of patients who have not stopped taking diuretics should be started with the smallest single dose of 1.25 mg ramipril. It is necessary to monitor kidney function and serum potassium levels. Subsequent dosage of Tritace® should be adjusted in accordance with the target blood pressure level.
Treatment of arterial hypertension
The dosage is calculated depending on the expected therapeutic effect and tolerability of the drug by the patient in each specific case.
Tritace® can be used either as monotherapy or in combination with other classes of drugs for the treatment of hypertension.
Initial dose
Treatment with Tritace® should be started with an initial dose of 2.5 mg daily.
In patients with a highly activated RAAS, a significant decrease in blood pressure may follow the initial dose. For such patients, the recommended starting dose is 1.25 mg, and initiation of treatment should be carried out under medical supervision.
Titration of an individual maintenance dose
The dose can be doubled at intervals of 2-4 weeks to achieve the target blood pressure level. The maximum daily dose is 10 mg. The daily dose is taken 1 time/day.
Prevention of cardiovascular accidents
Initial dose
The recommended starting dose is 2.5 mg Tritace® 1 time/day.
Titration of an individual maintenance dose
The dose is gradually increased depending on the patient's tolerance of the active substance. It is recommended to double the dose after 1-2 weeks of treatment, and after the next 2-3 weeks, increase the maintenance dose to 10 mg Tritace® daily.
Dosage recommendations should also be used in patients previously treated with diuretics.
Secondary prevention in patients with acute myocardial infarction with clinical
signs of heart failure
Initial dose
After 48 hours following myocardial infarction in clinically and hemodynamically stable patients, the recommended initial dose is 2.5 mg 2 times a day for 3 days. If the initial dose of 2.5 mg is not tolerated by the patient, it is necessary to prescribe 1.25 mg 2 times / day for 2 days before increasing the dose to 2.5 mg and 5 mg 2 times / day. If the dose cannot be increased to 2.5 mg 2 times / day, treatment should be discontinued.
Dosage recommendations should also be used in patients previously treated with diuretics.
Titration and individual maintenance dose
The daily dose is sequentially increased, doubling it at intervals of 1-3 days until a maintenance dose of 5 mg 2 times a day is reached.
It is recommended to divide the maintenance daily dose into 2 doses.
The maximum daily dose is 10 mg.
If a decision is made to treat Tritace® in a patient with severe (grade IV on the NYHA scale) chronic heart failure after myocardial infarction, it is recommended to start with a dose of 1.25 mg 1 time/day. The dose should be increased with extreme caution.
Treatment of kidney diseases
In patients with diabetes and microalbuminuria
Recommended starting dose
– 1.25 mg Tritace® 1 time/day.
The dose is sequentially increased depending on the patient's tolerance of the active substance. It is recommended to double the daily dose to 2.5 mg after 2 weeks of treatment, and then to 5 mg after the next 2 weeks.
In patients with diabetes and at least one cardiovascular risk factor
Recommended starting dose
– 2.5 mg Tritace® 1 time/day.
The dose is sequentially increased depending on the patient's tolerance of the active substance. It is recommended to double the daily dose to 5 mg after 2 weeks of treatment, and then to 10 mg after the next 2-3 weeks. The maximum daily dose is 10 mg.
In patients with nondiabetic nephropathy with macroproteinuria ≥ 3 g/day
Recommended initial
dose – 1.25 mg Tritace 1 time/day.
The dose is sequentially increased depending on the patient's tolerance of the active substance. It is recommended to double the daily dose to 2.5 mg after 2 weeks of treatment, and then to 5 mg after the next 2 weeks.
Treatment of symptomatic heart failure
Initial dose
For patients receiving diuretic therapy, the recommended initial dose is 1.25 mg Tritace 1 time / day.
Titration of an individual maintenance dose
It is recommended to double the dose of Tritace every two weeks to a maximum daily dose of 10 mg. It is preferable to divide the daily dose into 2 doses.
Patients
with impaired renal function
The daily dose for patients with impaired renal function is prescribed taking into account QC:
- if CC ≥ 60 ml/min, there is no need to adjust the initial dose (2.5 mg daily), the maximum daily dose is 10 mg;
- if CC is within 30-60 ml/min, there is no need to adjust the initial dose (2.5 mg daily), the maximum daily dose is 5 mg;
- if CC is in the range of 10-30 ml/min, the initial dose is 1.25 mg daily, and the maximum daily dose is 5 mg;
- in patients with hypertension undergoing hemodialysis: ramipril is poorly dialyzable; the initial dose is 1.25 mg daily, and the maximum daily dose is 5 mg; the drug must be taken several hours after hemodialysis.
Patients with liver dysfunction
Treatment of such patients should be carried out with extreme caution and only under medical supervision. The maximum permissible daily dose in such cases is 2.5 mg Tritace®.
Elderly patients
Initial doses should be lower and administered more gradually due to the increased risk of adverse reactions, especially in elderly and debilitated patients. The recommended initial daily dose is 1.25 mg Tritace®.
Children and teenagers under 18 years of age
Tritace® is not recommended for use in children and adolescents under 18 years of age due to insufficient relevant data on the safety and effectiveness of the drug.
Overdose
- weakness;
- dry mouth;
- bradycardia;
- drop in blood pressure;
- drowsiness;
- changes in water and electrolyte balance;
- shock;
- stupor;
- acute renal failure.
Therapy: the patient is placed in a horizontal position, legs are raised. Gastric lavage, administration of sodium sulfate and enterosorbing medications in the first 30 minutes after poisoning are effective.
For bradycardia, a pacemaker is used; If there is a sharp drop in blood pressure, catecholamines are administered intravenously. Hemodialysis has not proven effective.
Use during pregnancy and breastfeeding
Ramipril is contraindicated during pregnancy, as it can have an adverse effect on the fetus: impaired development of the fetal kidneys, decreased blood pressure in the fetus and newborns, impaired renal function, hyperkalemia, hypoplasia of the skull bones, oligohydramnios, contracture of the limbs, deformation of the skull bones, pulmonary hypoplasia.
Therefore, before starting to take the drug in women of childbearing age, pregnancy should be excluded.
If a woman is planning a pregnancy, treatment with ACE inhibitors should be discontinued.
If pregnancy occurs during treatment with Tritace®, you should stop taking it as soon as possible and transfer the patient to other drugs that will have the least risk for the child.
If treatment with Tritace® is necessary during breastfeeding, breastfeeding should be discontinued.
Interaction
Salty foods reduce the severity of the hypotensive effect. Ramipril can enhance the inhibitory effect of ethanol-containing drinks and solutions on the functioning of the central nervous system.
The hypotensive effect is enhanced by the simultaneous use of tricyclic antidepressants, diuretics, general anesthetics, and nitrates. Taking potassium-sparing diuretics ( Amiloride, Veroshpiron, Triamterene ) and potassium supplements can provoke hyperkalemia.
The hypotensive effect of Tritace Plus is reduced when treated with vasopressor types of sympathomimetics ( Norepinephrine, Epinephrine ). The risk of hematotoxicity increases with treatment with cytostatics, immunosuppressants, Allopurinol , Procainamide and glucocorticosteroids.
The active component Ramipril can reduce the excretion (slow down excretion) of lithium ions, which can lead to an increase in the severity of negative toxic reactions.
ACE inhibitors are characterized by an increased effect of hypoglycemic medications (sulfonylurea derivatives, insulin), which can provoke hypoglycemia. The hypotensive effect of Tritace Plus is weakened by treatment with Indomethacin , Acetylsalicylic acid and other NSAIDs. Heparin can provoke hyperkalemia.
The toxicity of glycosides increases significantly under the influence of hydrochlorothiazide, which is explained by hypomagnesemia and hypokalemia. Indirect anticoagulants, NSAIDs, Clofibrate and other drugs that bind to proteins to a high degree can enhance the diuretic effect of the drug.
The hypotensive effect of the drug is enhanced when taking tricyclic antidepressants, phenothiazines, barbiturates, beta blockers, vasodilators, ethanol.
The neurotoxicity of salicylates, the cardiotoxicity of lithium preparations and the effect of peripheral muscle relaxants increase with the use of hydrochlorothiazide.
The diuretic component of the drug slows down the elimination of Quinidine , weakens the effects of oral contraceptives, anti-gout medications, Epinephrine, hypoglycemic agents and Norepinephrine.
Hemolysis has been recorded during treatment with Hydrochlorothiazide and Methyldopa . The absorption of hydrochlorothiazide is reduced with the use of cholestyramine .
Pharmacokinetics
After oral administration, ramipril is rapidly absorbed from the gastrointestinal tract (50–60%). Eating slows down its absorption, but does not affect the completeness of absorption. Ramipril undergoes extensive first-pass metabolism/activation (mainly in the liver by hydrolysis), resulting in the formation of its only active metabolite, ramiprilat, whose ACE inhibitory activity is approximately 6 times greater than that of ramipril. In addition, as a result of the metabolism of ramipril, diketopiperazine, which does not have pharmacological activity, is formed, which is then conjugated with glucuronic acid. Ramiprilat is metabolized to diketopiperazic acid and glucuronidated.
The bioavailability of ramipril after oral administration ranges from 15% (for a dose of 2.5 mg) to 28% (for a dose of 5 mg). The bioavailability of the active metabolite, ramiprilat, after oral administration of 2.5 mg and 5 mg of ramipril is approximately 45% (compared to its bioavailability after intravenous administration in the same doses).
After oral administration of ramipril, Cmax of ramipril and ramiprilat in plasma is reached after 1 and 2–4 hours, respectively. The decrease in plasma concentration of ramiprilat occurs in several stages: a distribution and elimination phase with a T1/2 of ramiprilat of approximately 3 hours, then an intermediate phase with a T1/2 of ramiprilat of approximately 15 hours, and a final phase with a very low plasma concentration of ramiprilat. and T1/2 of ramiprilat, which is approximately 4–5 days. This final phase is due to the slow release of ramiprilat from its strong binding to ACE receptors. Despite the long final phase with a single oral dose of ramipril during the day at a dose of 2.5 mg or more, the equilibrium plasma concentration of ramiprilat is achieved after approximately 4 days of treatment. With a course prescription of the drug, the “effective” T1/2, depending on the dose, is 13–17 hours.
Plasma protein binding is approximately 73% for ramipril and 56% for ramiprilat.
After intravenous administration, the volume of distribution of ramipril and ramiprilat is approximately 90 and 500 L, respectively.
After oral administration of radiolabeled ramipril (10 mg), 39% of the radioactivity is excreted through the intestines and about 60% by the kidneys. After intravenous administration of ramipril, 50–60% of the dose is found in the urine in the form of ramipril and its metabolites. After IV administration of ramiprilat, about 70% of the dose is found in the urine in the form of ramiprilat and its metabolites, in other words, with IV administration of ramipril and ramiprilat, a significant part of the dose is excreted through the intestines with bile, bypassing the kidneys (50 and 30%, respectively ). After oral administration of 5 mg ramipril in patients with bile duct drainage, almost equal amounts of ramipril and its metabolites are excreted by the kidneys and intestines during the first 24 hours after administration.
Approximately 80–90% of the metabolites in urine and bile were identified as ramiprilat and ramiprilat metabolites. Ramipril glucuronide and ramipril diketopiperazine account for approximately 10–20% of the total amount, and the content of unmetabolized ramipril in urine is approximately 2%.
In animal studies, ramipril has been shown to be excreted into human milk.
In cases of renal dysfunction with creatinine Cl less than 60 ml/min, the excretion of ramiprilat and its metabolites by the kidneys slows down. This leads to an increase in plasma concentrations of ramiprilat, which decreases more slowly than in patients with normal renal function.
When taking ramipril in high doses (10 mg), impaired liver function leads to a slower first-pass metabolism of ramipril to active ramiprilat and a slower elimination of ramiprilat.
In healthy volunteers and patients with arterial hypertension, after 2 weeks of treatment with ramipril at a daily dose of 5 mg, no clinically significant accumulation of ramipril and ramiprilat was observed. In patients with chronic heart failure, after 2 weeks of treatment with ramipril at a daily dose of 5 mg, a 1.5-1.8-fold increase in plasma concentrations of ramiprilat and AUC is observed.
In healthy elderly volunteers (65–76 years), the pharmacokinetics of ramipril and ramiprilat do not differ significantly from those in young healthy volunteers.
special instructions
An assessment of the functional state of the renal system before starting antihypertensive therapy with Tritace Plus is mandatory. The special observation group includes patients with lesions of the renal vascular system (stenosis). Creatinine and urea levels are the main indicators of the condition of the renal system.
In chronic renal failure, hyperkalemia may occur. With pathology of the hepatic system, the formation of the active metabolite slows down and the metabolic .
The risk of low blood pressure increases significantly in patients who are on a salt-free (or low-salt) diet. Symptomatic hypotension develops with decreased blood volume.
In transient forms of arterial hypotension, therapy with Tritace Plus can be carried out only after stabilization of blood pressure.
In patients undergoing hemodialysis using special dialysis membranes such as AN69, the risk of anaphylactoid responses and hypersensitivity increases. Similar reactions were observed when apheresis of LDL was performed with dextran sulfate.
Tritace®
Before starting treatment with Tritace®, hyponatremia and hypovolemia must be eliminated. In patients who have previously taken diuretics, it is necessary to discontinue them or at least reduce their dose 2-3 days before starting Tritace® (in this case, the condition of patients with chronic heart failure should be carefully monitored, due to the possibility of developing their decompensation with an increase in circulating blood volume).
After taking the first dose of the drug, as well as when increasing its dose and/or the dose of diuretics (especially loop diuretics), it is necessary to ensure careful medical monitoring of the patient for at least 8 hours in order to timely take appropriate measures in case of an excessive decrease in blood pressure.
If Tritace® is used for the first time or at a high dose in patients with increased RAAS activity, their blood pressure should be carefully monitored, especially at the beginning of treatment, since these patients have an increased risk of an excessive decrease in blood pressure (see section "With caution") .
In case of malignant arterial hypertension and heart failure, especially in the acute stage of myocardial infarction, treatment with Tritace® should only be started in a hospital setting.
In patients with chronic heart failure, taking the drug can lead to the development of a pronounced decrease in blood pressure, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure.
Caution should be exercised when treating elderly patients, as they may be particularly sensitive to ACE inhibitors; it is recommended to monitor renal function in the initial phase of treatment (see also section "Dosage and Administration").
In patients for whom a decrease in blood pressure may pose a certain risk (for example, in patients with atherosclerotic narrowing of the coronary or cerebral arteries), treatment should begin under strict medical supervision.
Caution should be exercised during physical activity and/or hot weather due to the risk of increased sweating and dehydration with the development of arterial hypotension due to a decrease in circulating blood volume and a decrease in sodium levels in the blood.
It is not recommended to drink alcohol (ethanol) during treatment with Tritace®.
A transient excessive decrease in blood pressure is not a contraindication for continuing treatment after stabilization of blood pressure. In case of repeated development of a pronounced decrease in blood pressure, the dose should be reduced or the drug discontinued.
The simultaneous use of Tritace® with drugs containing aliskiren or with ARA II, leading to double blockade of the RAAS, is not recommended due to the risk of an excessive decrease in blood pressure, the development of hyperkalemia and deterioration of renal function compared to monotherapy.
The simultaneous use of Tritace® and drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or moderate to severe renal failure (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients (see Sections “Contraindications” and “Interaction with other drugs”).
Concomitant use of ARA II is contraindicated in patients with diabetic nephropathy and is not recommended in other patients (see sections “Contraindications” and “Interaction with other drugs”).
Angioedema
Cases of angioedema of the face, extremities, lips, tongue, pharynx or larynx have been observed in patients treated with ACE inhibitors. If swelling occurs in the face (lips, eyelids) or tongue, or difficulty swallowing or breathing, the patient should immediately stop taking the drug.
Angioedema, localized in the area of the tongue, pharynx or larynx (possible symptoms: difficulty swallowing or breathing), can be life-threatening and requires urgent measures to relieve it: subcutaneous administration of 0.3-0.5 mg or intravenous drip of 0.1 mg of epinephrine (adrenaline) (under the control of blood pressure, heart rate and ECG) followed by the use of glucocorticosteroids (iv, intramuscular or orally); Intravenous administration of antihistamines (H1- and H2-histamine receptor antagonists) is also recommended, and in case of deficiency of the C1-esterase enzyme inactivator, the need to administer C1-esterase enzyme inhibitors in addition to epinephrine (adrenaline) can be considered. The patient should be hospitalized and monitored until symptoms are completely relieved, but not less than 24 hours.
Cases of intestinal angioedema, manifested by abdominal pain with or without nausea and vomiting, have been observed in patients receiving ACE inhibitors; in some cases, angioedema of the face was also observed simultaneously.
If a patient develops the symptoms described above during treatment with ACE inhibitors, the possibility of developing intestinal angioedema should be considered when making a differential diagnosis.
When used simultaneously with other drugs that can cause the development of angioedema, the risk of angioedema increases (see sections “Contraindications”, “Interaction with other drugs”).
Treatment aimed at desensitization to insect venom (such as bees, wasps) and concomitant use of ACE inhibitors can initiate anaphylactic and anaphylactoid reactions (eg, decreased blood pressure, shortness of breath, vomiting, allergic skin reactions), which can sometimes be life-threatening. During treatment with ACE inhibitors, hypersensitivity reactions to insect venom (such as bees, wasps) develop faster and are more severe. If desensitization to insect venom is necessary, the ACE inhibitor should be temporarily replaced with a corresponding drug from another group.
Life-threatening, rapidly developing anaphylactoid reactions, sometimes leading to shock, have been described with the use of ACE inhibitors during hemodialysis or plasma filtration using certain high-flux membranes (for example, polyacrylonitrile membranes) (see also membrane manufacturer's instructions). The combined use of Tritace® and the use of this type of membrane, for example, for emergency hemodialysis or hemofiltration, should be avoided. In this case, it is preferable to use other types of membranes or avoid taking ACE inhibitors.
Similar reactions were observed with low-density lipoprotein apheresis using dextran sulfate. Therefore, this method should not be used in patients receiving ACE inhibitors.
Liver dysfunction
In patients with impaired liver function, the response to treatment with Tritace® may be enhanced or weakened. In addition, in patients with severe liver cirrhosis with edema and/or ascites, significant activation of the RAAS is possible, so special care should be taken when treating these patients (see also section "Dosage and Administration").
Surgical interventions
Before surgery (including dental surgery), it is necessary to warn the surgeon/anesthesiologist about taking ACE inhibitors.
Cough
When using the drug Tritace®, a dry, unproductive, prolonged cough may occur, which disappears after stopping the use of ACE inhibitors, which must be taken into account in the differential diagnosis of cough during the use of an ACE inhibitor.
Ethnic characteristics
The drug Tritace®, like other ACE inhibitors, has a less pronounced antihypertensive effect in patients of the Negroid race compared to representatives of other races.
The drug Tritace® should be prescribed with caution to patients of the Black race due to a higher risk of developing angioedema.
Patients after kidney transplantation
There is insufficient experience with the use of Tritace® in patients who have recently undergone kidney transplantation.
Monitoring laboratory parameters before and during treatment with Tritace® (up to 1 time per month in the first 3-6 months of treatment)
Monitoring kidney function (determining serum creatinine concentrations)
When treating with ACE inhibitors, it is recommended to monitor renal function in the first weeks of treatment and subsequently. Particularly careful monitoring is required in patients with acute and chronic heart failure, impaired renal function, after kidney transplantation, patients with renovascular diseases, including patients with hemodynamically significant unilateral renal artery stenosis in the presence of two kidneys (in such patients, even a slight increase in serum creatinine concentration may be indicator of decreased kidney function).
Electrolyte control
Regular monitoring of serum potassium and sodium levels is recommended. Particularly careful monitoring of potassium levels in the blood serum is required for patients with impaired renal function, significant disturbances in water and electrolyte balance, and chronic heart failure.
Monitoring of hematological parameters (hemoglobin, number of leukocytes, erythrocytes, platelets, leukocyte formula)
It is recommended to monitor general blood dialysis levels to identify possible leukopenia. More regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, as well as in patients with connective tissue diseases or in patients simultaneously receiving other drugs that can change the peripheral blood picture (see section "Interactions with other drugs") .
Monitoring the number of leukocytes is necessary for the early detection of leukopenia, which is especially important in patients with an increased risk of its development, as well as at the first signs of infection. If neutropenia is detected (the number of neutrophils is less than 2000/μl), discontinuation of treatment with ACE inhibitors is required.
If symptoms due to leukopenia appear (for example, fever, enlarged lymph nodes, tonsillitis), urgent monitoring of the peripheral blood picture is necessary. If signs of bleeding appear (tiny petechiae, red-brown rashes on the skin and mucous membranes), monitoring the number of platelets in the peripheral blood is also necessary.
Determination of the activity of “liver” enzymes, the concentration of bilirubin in the blood
If jaundice or a significant increase in the activity of liver enzymes appears, treatment with Tritace® should be discontinued and the patient should be monitored medically.
Analogs
Level 4 ATX code matches:
Akkuzid
Enap-N
Iruzid
Co-Diroton
Enalozide
Enap NL
Enapril-N
Capozide
Enzix
Liprazid
Co-Renitec
Hartil N
Hartil D
Noliprel
Ko-Perineva
Kaptopres
- Amprilan ND;
- Amprilan NL;
- Hartil D;
- Ramazid N.
Tritace Plus price, where to buy
The cost of the medication depends on the combination, pharmacy chain and region of sale.
The average price of Tritace Plus in Russia is 600 rubles.
- Online pharmacies in UkraineUkraine
Pharmacy24
- Tritace plus 10 mg/12.5 mg N28 tablets Sanofi-Aventis S.p.A.,Italy/Sanofi S.P.A.Italy
206 UAH.order - Tritace plus 5 mg/12.5 mg No. 28 tablets Sanofi-Aventis S.p.A., Italy
141 UAH order
Tritace plus tablets 10mg/12.5mg No. 14x2
Name
Tritace plus 10 mg/12.5 mg tablet in blister pack. in pack No. 14x2
Description
Tritace® Plus 10 mg/12.5 mg: oblong orange tablets with a score on both sides. Top stamp: 42/AV. Bottom stamp: absent. There may be inclusions of a darker color. Tritace® Plus 10 mg/25 mg: pink oblong tablets scored on both sides. Top stamp: 39/AV. Bottom stamp: absent. There may be inclusions of a darker color.
Main active ingredient
Ramipril, hydrochlorothiazide
Release form
Pills
Dosage
10mg/12.5mg
pharmachologic effect
Drugs affecting the renin-angiotensin system. ACE inhibitors and diuretics. ATX code: C09BA05.
Indications for use
This drug is indicated for the treatment of hypertension in patients for whom this combination therapy is suitable. This drug is not intended for initial therapy (see Dosage and Administration). Patients who started taking ramipril and diuretics simultaneously may develop symptomatic hypotension. Dose titration should be carried out for each drug component separately. If the individual dose of drugs and the frequency of administration are determined during titration and correspond to the combined form, then it may be more convenient to use Tritace Plus for treating the patient. If dose adjustment is required during maintenance therapy, it is better to carry out treatment with separate medicinal components. When using Tritace Plus, the possibility of developing angioedema should be taken into account (see Contraindications and Special instructions and precautions for use. Immune system. Angioedema). Elderly patients (>65 years) Clinical data on the use of the drug in patients over 65 years of age are limited (see Special instructions and precautions for use). Children (
Directions for use and doses
General information Dosage is individual. Tritace Plus (ramipril/hydrochlorothiazide) is not intended for initial therapy. The dose of Tritace Plus is selected during titration of individual components. Particular attention is paid to patients on dialysis. Recommended dose and dose adjustment Adults The dose is selected individually depending on the patient's condition (see Precautions) and blood pressure control. Tritace Plus 10 mg/12.5 mg tablets and Tritace Plus 10 mg/25 mg tablets are taken one tablet per day. The maximum permitted daily dose is 10 mg ramipril and 25 mg hydrochlorothiazide. Doses for elderly patients Initial doses should be reduced and subsequent dose adjustments should be more gradual due to the greater likelihood of adverse effects, especially in very old or debilitated patients (see Precautions). Doses for patients with impaired renal function Moderate impairment of renal function (creatinine clearance 30 - 60 ml/min per 1.73 m2 body surface area): In patients with moderate impairment of renal function, treatment begins with monotherapy with ramipril at a dose of 1.25 mg/day . Then the dose of ramipril is gradually increased, treatment with the combination begins with a daily dose of 2.5 mg ramipril/12.5 mg hydrochlorothiazide. The maximum permitted daily dose: 5 mg ramipril/25 mg hydrochlorothiazide (such patients should not be prescribed Tritace Plus 10 mg/12.5 mg and Tritace Plus 10 mg/25 mg). Tritace Plus is contraindicated in patients with severe renal impairment (creatinine clearance less than 30 ml/min per 1.73 m2 body surface area) and hemodialysis patients (see Contraindications). Doses for patients with hepatic impairment Mild or moderate hepatic impairment: In patients with mild or moderate hepatic impairment, treatment with Tritace Plus should only be initiated under strict medical supervision; the maximum daily dose is 2.5 mg ramipril/12.5 mg hydrochlorothiazide. The use of Tritace Plus 5 mg/25 mg, 10 mg/12.5 mg and 10 mg/25 mg is prohibited in such patients. Tritace Plus is contraindicated in patients with severe hepatic impairment (see Contraindications). Dosage for patients treated with diuretics In patients treated with diuretics, consider discontinuing the current diuretic at least 2-3 days or even earlier (depending on the duration of action of the diuretic) before starting treatment with Tritace Plus or at least reduce the dose of diuretic. If it is impossible to discontinue diuretic therapy, treatment should begin with the lowest possible dose of ramipril (1.25 mg/day) in the form of a free combination. Subsequently, it is recommended to replace the initial daily dose with no more than 2.5 mg ramipril/12.5 mg hydrochlorothiazide. Missed Doses If a dose of the drug is missed, it should be taken as soon as possible. However, if the fact of missing a dose is discovered close to the time of taking the next dose, then you should not take the missed dose, but follow the regular dosing schedule. Do not double the dose! Directions for use Tritace Plus tablets should be taken with a sufficient amount of liquid (about half a glass). Tablets should not be chewed or bitten. It is usually recommended to take the entire daily dose in the morning at one time. Food does not have a significant effect on the therapeutic effects of Tritace Plus.
Use during pregnancy and lactation
Pregnancy Ramipril Tritace Plus is not recommended for use during the first trimester of pregnancy (see Precautions), the drug is contraindicated during the second and third trimesters (see Contraindications). Epidemiological data on the teratogenic risk of exposure to ACE inhibitors during the first trimester of pregnancy are equivocal, but a slight increase in risk cannot be ruled out. Unless treatment with ACE inhibitors is essential, patients planning pregnancy should be switched to alternative antihypertensive therapy with a known safety profile in pregnancy. If pregnancy is detected, treatment with inhibitors should be stopped immediately and, if necessary, alternative therapy should be prescribed. The use of ACE inhibitors/angiotensin receptor antagonists type 2 (AAR2) during the second and third trimesters of pregnancy is known to have fetotoxic effects (decreased renal function, oligohydramnios, delayed ossification of the skull bones) and toxic neonatal effects (renal failure, hypotension, hyperkalemia) ( see Pharmacokinetics). If ACE inhibitors are used during the second trimester of pregnancy, ultrasound assessment of the fetal skull and renal function is recommended. Neonates whose mothers took ACE inhibitors should be closely monitored for early detection of hypotension, oliguria, and hyperkalemia (see Precautions and Contraindications). Hydrochlorothiazide Hydrochlorothiazide, in cases of prolonged exposure during the third trimester of pregnancy, may cause fetoplacental ischemia and the risk of developmental delay. Moreover, rare cases of hypoglycemia and thrombocytopenia in newborns have been reported when they were exposed to the drug in the last weeks of pregnancy. Hydrochlorothiazide may cause a decrease in plasma volume as well as uteroplacental blood flow. Breastfeeding Tritace Plus is contraindicated during breastfeeding. Ramipril and hydrochlorothiazide are excreted into breast milk in such quantities that their effects may occur in a breastfed baby if a nursing woman uses ramipril and hydrochlorothiazide in therapeutic doses. Ramipril There is insufficient information on the use of ramipril during breastfeeding, therefore, during this period, it is recommended to use alternative therapies with a better established safety profile during breastfeeding, especially when feeding newborns or premature infants. Hydrochlorothiazide Hydrochlorothiazide is excreted in human milk. Thiazides are associated with decreased or suppressed lactation in nursing mothers. It is possible to develop hypersensitivity to drugs based on sulfonamide derivatives, hypokalemia and kernicterus. Due to the possibility of serious reactions in breastfed children caused by each of the active substances, the physician should decide whether it is advisable to stop breastfeeding or discontinue therapy, taking into account the significance of the therapy for the mother.
Precautionary measures
Important warnings and precautions ACE inhibitors, if taken during pregnancy, can cause harm to the developing fetus and even cause its death (see Special instructions. Special groups of patients. Pregnancy). If you become pregnant, you should stop taking Tritace Plus (ramipril and hydrochlorothiazide) as soon as possible. General Cough A dry, persistent cough has been described, usually disappearing only after discontinuation of Tritace Plus. It is probably associated with taking ramipril, an ACE inhibitor included in the drug. This possibility must be taken into account when making a differential diagnosis of cough (see Side effects. Effects identified during clinical trials). Dual blockade of the renin-angiotensin system (RAS) There is evidence that the use of angiotensin-converting enzyme (ACE) inhibitors, such as ramipril in Tritace Plus, or angiotensin receptor blockers (ARBs) with aliskiren in patients with diabetes mellitus (types 1 and 2) and/or moderate to severe renal impairment (GFR 65 years), increased sensitivity is possible. Monitoring and laboratory tests Hematology It is necessary to pay attention to periodic monitoring of the number of peripheral blood leukocytes in order to identify possible leukopenia caused by ramipril, which is part of Tritace Plus. More frequent monitoring is recommended in the initial phase of treatment and in patients with impaired renal function, in patients with concomitant collagen diseases (for example, lupus erythematosus, scleroderma) and in patients undergoing treatment with other drugs that can cause changes in the blood picture (see Measures). precautions. Hematology. Neutropenia and agranulocytosis). Metabolism Appropriate control of electrolytes and blood sugar is necessary. Renal function The use of Tritace Plus should be accompanied by appropriate monitoring of renal function. During treatment, it is necessary to carry out the same strict monitoring of renal function as for renal failure (see Precautions: Kidney). Particularly carefully it is necessary to monitor patients with: heart failure; renovascular diseases, including patients with hemodynamically significant unilateral renal artery stenosis. In the latter group of patients, even a slight increase in serum creatinine may indicate unilateral loss of renal function; impaired renal function; kidney transplants in elderly or geriatric patients. Use of the drug during pregnancy and breastfeeding Pregnancy Ramipril Tritace Plus is not recommended for use during the first trimester of pregnancy (see Precautions), the drug is contraindicated during the second and third trimesters (see Contraindications). Epidemiological data on the teratogenic risk of exposure to ACE inhibitors during the first trimester of pregnancy are equivocal, but a slight increase in risk cannot be ruled out. Unless treatment with ACE inhibitors is essential, patients planning pregnancy should be switched to alternative antihypertensive therapy with a known safety profile in pregnancy. If pregnancy is detected, treatment with inhibitors should be stopped immediately and, if necessary, alternative therapy should be prescribed. The use of ACE inhibitors/angiotensin receptor antagonists type 2 (AAR2) during the second and third trimesters of pregnancy is known to have fetotoxic effects (decreased renal function, oligohydramnios, delayed ossification of the skull bones) and toxic neonatal effects (renal failure, hypotension, hyperkalemia) ( see Pharmacokinetics). If ACE inhibitors are used during the second trimester of pregnancy, ultrasound assessment of the fetal skull and renal function is recommended. Neonates whose mothers took ACE inhibitors should be closely monitored for early detection of hypotension, oliguria, and hyperkalemia (see Precautions and Contraindications). Hydrochlorothiazide Hydrochlorothiazide, in cases of prolonged exposure during the third trimester of pregnancy, may cause fetoplacental ischemia and the risk of developmental delay. Moreover, rare cases of hypoglycemia and thrombocytopenia in newborns have been reported when they were exposed to the drug in the last weeks of pregnancy. Hydrochlorothiazide may