Author of the article: Sergey Vyalov, gastroenterologist, hepatologist, Ph.D.
The duodenal bulb (DU) is called the bulbar region. Hence the name of the disease: bulbitis is an inflammation of the mucous membrane of the duodenal bulb. It is quite popular that bulbitis causes gastritis. Actually this is not true. The diseases are interconnected, but still develop in parallel to each other.
Description
Bulbitis is an inflammatory lesion of the duodenal bulb (from the Latin bulbus - bulb). It is a type of duodenitis and often occurs against the background of hyperacid gastritis and other diseases of the digestive system. It can be acute or chronic, catarrhal or erosive. Has code K26.9 according to ICD-10. It can develop in people of any age, including children. Women aged 20-40 who suffer from neuroses and hormonal disorders most often fall ill.
Causes
The main cause of chronic bulbitis is Helicobacter pylori infection in patients with hyperacid gastritis. The risk of developing the disease increases under the following circumstances:
- Anatomical features . Normally, the mesentery of the duodenum forms and then disappears in the embryonic period. Some people retain this organ throughout their lives. The presence of the mesentery creates favorable conditions for the formation of intestinal loops and subsequent stagnation of the contents.
- Psychological factors . Emotional instability and frequent stress cause changes in the level of catecholamines in the blood and cause excessive activation of the sympathetic nervous system. This causes a narrowing of intestinal vessels with impaired blood supply and contributes to the development of inflammatory processes.
- Endogenous factors . The protective properties of the intestinal mucosa are reduced in severe somatic pathologies, immunodeficiencies of various etiologies, and the presence of certain genetic and constitutional characteristics. There is a connection between bulbitis and celiac disease, Zollinger-Ellison syndrome, and Crohn's disease.
- Exogenous factors . When consuming strong alcoholic drinks, too spicy, sweet and salty foods, microtraumas of the mucous membranes occur, against which surface inflammation occurs. Damage to the mucous membranes is also caused by taking certain medications. With frequent trauma or other circumstances, acute inflammation becomes chronic.
The cause of acute bulbitis can be foodborne illness, dysentery, salmonellosis, or viral hepatitis A.
Development mechanism
The bulb is the initial part of the duodenum (duodenum). It is located immediately after the pylorus - a muscular sphincter in the lower part of the stomach. The environment in the stomach is acidic, while in the underlying parts of the digestive tract it is alkaline. The main function of the onion is to neutralize the acidity of the food bolus after it comes from the stomach. If the contents are too acidic (with hyperacid gastritis), this adversely affects the mucous membrane of the bulb.
Tissues are damaged, against this background inflammation occurs, provoked by Helicobacter pylori infection. Helicobacter pylori bacteria are well adapted to exist in an acidic environment. They form a protective shell around themselves and potentiate the production of substances that aggravate damage to the intestinal wall. With prolonged or too aggressive exposure, the formation of erosions and ulcers is possible.
Causes
The causes of bulbitis are in many ways similar to the causes of gastritis:
- pharmaceuticals;
- chemical burns;
- love of alcoholic drinks;
- habit of eating too hot food;
- infection with helminths or lamblia (especially typical for children);
- variant of manifestation of Crohn's disease, etc.;
- poor nutrition (eating on the go, addiction to junk food, habit of eating once a day, but a lot, etc.);
- bacteria Helicobacter pylori (especially in the case of catarrhal form or mixed bulbitis);
- mechanical trauma to an organ (swallowing an indestructible object, which can damage the walls of the organ, often leading to focal damage).
Symptoms
Photo: health.24tv.ua
The main manifestation of bulbitis is pain. In the catarrhal form of the pathology, the pain is insignificant, pulling or aching. They usually occur 1.5 or more hours after eating and are localized in the epigastric region. In patients with erosive bulbitis, the pain is intense, cutting, and paroxysmal. Appear on an empty stomach or a few minutes after eating.
Over time, the location of pain often changes. There is irradiation to the right, and in some cases to the left hypochondrium. The pain does not occur in the epigastrium, but in the navel area. The severity of the pain syndrome is determined by the phase of the disease. During the period of remission, the symptom disappears or becomes mildly expressed, during the period of exacerbation it intensifies and becomes more frequent. With erosive and ulcerative forms, night pain is possible.
Other symptoms include a feeling of heaviness and fullness in the stomach after eating, heartburn, and belching something bitter or sour. Some patients note a frequent taste of bitterness in the mouth or bad breath. There are disturbances in appetite, nausea, and sometimes single vomiting. With ulcerative lesions, bleeding is possible, which is manifested by vomiting mixed with blood, black stools (melena), weakness, decreased blood pressure, tachycardia, and fainting. With significant blood loss, there is a risk of developing hemorrhagic shock.
Acute bulbitis due to intestinal infections is characterized by general hyperthermia, weakness, weakness, severe nausea, repeated vomiting, and cramping abdominal pain. The severity of the patient's condition is determined by the type of infectious agent and the extent of gastrointestinal lesions. When a significant part of the intestine is involved, diarrhea with copious loose stools, body aches, chills, tachycardia, dry and pale skin are detected.
Types of bulbite
According to the nature of its course, bulbitis has an acute and chronic form:
- The acute form of bulbitis is accompanied by severe pain, nausea, vomiting and a bitter taste in the mouth.
- The chronic form of bulbitis is accompanied by bursting or aching pain in the solar plexus. Sometimes there is a feeling of nausea without vomiting. Chronic bulbitis lasts for years with seasonal exacerbations.
Depending on the form of the course and the characteristic features of inflammation, the disease is divided into the following main types:
- erosive;
- surface;
- catarrhal
Other types of bulbite
- Follicular bulbitis is quite rare and causes severe digestive disorders and causes serious inconvenience to the patient.
- Moderate bulbitis can occur latently, similar to the superficial form, and may be accompanied by headache, nausea and vomiting. Such symptoms are especially pronounced in cases of exacerbation of the disease.
- Focal bulbitis affects small areas of the duodenal bulb - lesions - hence its name. With such bulbitis, along with the main treatment, strict diets are prescribed. Focal bulbitis is very dangerous, and its symptoms are quite eloquent; you should not delay seeking medical help.
- Atrophic bulbitis causes dysfunction of the duodenum. Such disturbances cause severe vomiting. A characteristic feature is loss of body weight.
Diagnostics
Photo: belhope.ru
A gastroenterologist examines patients with bulbitis. The specialist finds out when the unpleasant symptoms first appeared and how the disease developed. Clarifies the frequency and duration of exacerbations, severity of manifestations.
The appearance of the patient with chronic bulbitis is not changed, the condition is satisfactory except for cases of bleeding, when pale skin, tachycardia and hypotension may be noted. The condition of acute bulbitis depends on the severity of symptoms. On palpation, pain in the epigastric region is determined. White coating and teeth marks are visible on the tongue. The diagnostic program includes the following methods:
- Esophagogastroduodenoscopy . It is a basic examination method for suspected bulbitis. Allows you to conduct a visual examination of the stomach and duodenum and take a biopsy for morphological analysis. A decrease or increase in folding, swelling and hyperemia of the bulb are detected. Sometimes erosions, ulcers, cicatricial narrowings, and sources of bleeding are visualized.
- X-ray studies . Plain radiography of the abdominal cavity helps to confirm a violation of the relative position of the stomach and duodenum, the formation of intestinal loops, indicating the presence of a mesentery. When performing gastroduodenography, changes in relief, contrast delay (bulbostasis), asynchrony of contractions, the presence of spasmodic areas, deformations, an increase in the size or narrowing of the bulb, and filling defects (with ulcers) may be observed.
- Specific tests . With hyperacid gastritis, according to pH-metry, an increase in the acidity of gastric juice is detected. The easiest way to confirm the presence of Hilobacter pylori is a breath test. Antibodies and microbial fragments are detected by enzyme immunoassay or polymerase chain reaction using blood, stool, saliva or urine.
- Other laboratory tests . According to histological or cytological examination, inflammatory infiltration of the mucosa is confirmed. A biochemical blood test may reveal an increase in pancreatic and liver enzymes. In case of bleeding, a complete blood count (decrease in the level of hemoglobin and red blood cells) and a stool test for occult blood are informative.
- Ultrasound of the abdominal organs . It is necessary because bulbitis often accompanies other diseases of the digestive system. Makes it possible to diagnose pathologies of the liver and pancreas, determine signs of cholecystitis and biliary dyskinesia.
How to treat chronic bulbitis?
For chronic and catarrhal bulbitis, antibacterial therapy is prescribed, since this type of bulbitis develops, as a rule, due to Helicobacter pylori infection. Antibiotics are prescribed taking into account the sensitivity of the pathogen to them. These can be certain groups of antibiotics that act on the cell of the pathogen itself - Amoxicycline, Vilprafen, Summed, De-nol and others. Sometimes Metronidazole can be prescribed, but nowadays its effectiveness among potential “killers” of Helicobacter is disputed.
Also, with this type of bulbitis, a long-term diet is prescribed. In addition, you must stop smoking. Avoid stressful situations whenever possible. It is necessary to stop taking all kinds of food additives; they can also be a provoking factor for the exacerbation of catarrhal and chronic bulbitis. Also, in stressful situations, during the treatment of this type of bulbitis, sedatives and sedatives are prescribed.
You should understand and be psychologically prepared for the fact that you will have to reconsider your usual way of life, since the treatment will be complex and long-term.
Treatment
Photo: corpmsp.ru
Treatment of bulbitis is often conservative and includes medicinal and non-medicinal measures. The therapeutic program involves the use of the following techniques:
- Diet . In the acute phase, frequent split meals are indicated with the exception of too hot or cold, coarse, spicy and spicy foods. Recommended are puree soups and steamed dishes. During the period of remission, the patient is advised to refrain from eating foods that irritate the duodenal mucosa.
- Eradication of Helicobacter . It is carried out using standard complex schemes. Metronidazole destroys the DNA of microorganisms. Proton pump inhibitors provide an increase in the concentration of the antibiotic in the stomach and duodenum. Bismuth attacks the cell walls of bacteria and reduces the activity of urease, which is involved in the life cycle of the pathogen.
- Other drugs . For increased acidity, H-2 histamine receptor blockers, M-anticholinergics, and antacids are prescribed. For erosions and ulcers, medications are used that stimulate mucus formation and accelerate the restoration of the mucous membrane: licorice root, sea buckthorn and rose hip oils, and other astringent and enveloping medications. Antispasmodics are effective for pain; prokinetics are effective for bulbostasis and reflux.
During periods of exacerbation, electrophoresis with antispasmodics and painkillers is useful. In the remission phase, sanatorium-resort treatment is recommended. In the presence of concomitant gastrointestinal diseases, appropriate therapy is carried out. Patients with neurotic disorders are referred to a psychotherapist and, if necessary, antidepressants are prescribed.
Emergency surgical interventions are indicated when bleeding develops and are carried out using endoscopic equipment. Bleeding vessels are sutured, cauterized or clamped using a clip. If the source of bleeding cannot be determined during gastroduodenoscopy, the duodenal ulcer is sutured using open access.
Planned operations are performed for ulcers and duodenal stenosis. For ulcers, trunk, proximal or selective vagotomy is used. After crossing the vagus nerve or its branches, the secretion of hydrochloric acid by secretory gastric cells decreases, and favorable conditions for ulcer healing are created in the duodenum. When the 12-gut is narrowed, reconstructive interventions are performed aimed at restoring normal passage of food.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Prognosis and prevention
If you seek specialized help in a timely manner, prescribe adequate therapy for bulbitis and eradicate Helicobacter, the prognosis is favorable. Patients must follow dietary therapy recommendations and, if necessary, adjust their lifestyle. You should stop smoking and drinking alcohol.
Prevention of bulbitis involves timely treatment of gastritis with mandatory post-therapy tests confirming the eradication of the pathogen. Even without exacerbations, it is necessary to regularly attend medical examinations. Many drugs are aggressive to the mucous membrane of the stomach and duodenum, therefore, for bulbitis, all drugs should be used only after consultation with a doctor.
To prevent infection with Helicobacter, you should maintain food hygiene and wash your hands thoroughly before eating.
Diet
A necessary condition for effective treatment is adherence to a diet, the basic principles of which are aimed at reducing the load and ensuring a state of rest for the duodenum and stomach.
Eating with bulbitis, as well as with gastritis, which may be the cause of its development, is necessary in compliance with the rules of food preparation.
Eating should be moderate, unhurried, and long breaks should not be taken between meals. It must be steamed, especially at first, without using seasonings or spices.
It is recommended to exclude from the diet all foods that irritate the mucous membrane of the digestive system: spicy, sour, fried, salty, smoked, fatty, carbonated drinks, black coffee, alcohol.
For dietary purposes it is useful to use:
- milk or dairy products;
- lean meat: rabbit, chicken, veal;
- fish: pollock, hake, cod;
- white bread, pasta, cereals;
- compote, tea, jelly.
There are cases where strict adherence to a diet in the initial stages of the disease helped patients get rid of the disease without the use of medications.
Complications
In advanced cases, bulbitis is burdened with serious complications.
A focal figure can cause disturbances in the functioning of the digestive system. Without proper treatment, they progress to erosion. When ulcers occur, food can enter the abdominal cavity, which leads to peritonitis.
In the erosive form of inflammation of the bulbin, a duodenal ulcer may occur. If it is in a blister, there is a risk of perforation and bleeding.
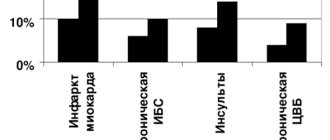
Superficial chronic bulbitis is characterized by bleeding in the gastrointestinal tract, about 10% of bleeding develops due to this type of disease. The second complications are the development of larger duodenal cancer.
The administered treatment is fatal.
Symptoms of acute pyelonephritis in men
Since in men the pathology develops mainly due to narrowing of the urethra, tissue proliferation, and the presence of tumor-like formations, the symptoms of pyelonephritis are complicated by signs of the primary disease:
- suppression of appetite leading to weight loss;
- weakness, fatigue;
- difficulty urinating;
- soreness in the lower back;
- a feeling of incomplete emptying of the bladder, constant thirst;
- frequent urge to urinate.
As in women, in men acute pyelonephritis occurs with signs of general intoxication of the body. These include high fever, chills, and excessive sweating. If dark blood streaks or admixtures of fresh blood appear in the urine, this may indicate displacement of the stone.