Acute neck pain (cervicalgia) is one of the most common reasons for seeking medical help and temporary disability. Periodically occurring acute neck pain is observed in 12.1-71.5% of people of working age [1, 2]. Its manifestations vary - from a single episode to chronic pain. Within 1 year, 1.7% of adults experience at least one disabling episode of neck pain, and 11.5% experience significant disability [3]. In young patients, the most common cause of neck pain is myofascial syndrome. With age, the prevalence of cervicalgia increases, which is primarily due to skeletal deformation.
The development of neck pain associated with musculoskeletal disorders is closely related to occupational activity. The highest prevalence of cervicalgia (74%) was thought to be among crane operators [4]. In recent years, there has been an increase in the prevalence of neck pain due to many other professions and circumstances, which is associated with both prolonged stay in one position (sitting at a computer), low physical activity, as well as an increase in neck injuries, including non-severe ones, for example as a result of road traffic accidents [5].
Acute cervicalgia is characterized as stiffness and/or pain in the cervical spine, often accompanied by classic symptoms of inflammation - redness, muscle tension, fever, limited movement. The causes of acute neck pain are damage to the muscles, ligaments, discs, and facet joints, followed by the development of inflammation and painful muscle tension. The most common source of pain is the muscles and ligaments. When exposed to provoking factors (postural stress, hypothermia, microtrauma), inflammatory mediators, prostaglandins, are released, which stimulate nociceptors, causing pain.
The role of myofascial syndrome in provoking primary headaches is actively discussed. Population-based studies have shown the prevalence of neck pain among patients with migraine or other types of primary headaches [3]. D. Watson et al. [6] showed that pressing on trigger points provokes a typical primary headache for the patient - tension-type headache (TTH) - in 100%, migraine - in 96% of cases. In the absence of primary headache, pressing on trigger points provoked cephalalgia only in 57% of cases [6, 7]. The importance of active myofascial trigger points in the chronification of primary headache, especially tension-type headache, has been noted [8].
At the same time, neck muscle tension is considered by many authors as a correlate of central sensitization. The most common myofascial trigger points for patients with chronic migraine or chronic tension-type headache are located in the trapezius muscle [9, 10]. Moreover, painful tension in the neck muscles is a prodromal symptom of a migraine attack in 38% of patients [11]. Stressful events and anxiety and depressive disorders play a significant role in the development of painful muscle tension [12].
According to the International Classification of Headache Disorders III (2003), headache associated with neck myofascial syndrome should be coded as infrequent tension-type headache with pericranial muscle tension (2.1.1), frequent tension-type tension with pericranial muscle tension (2.2.1), or chronic tension-type headache with tension. pericranial muscles (2.3.1). It is also possible to use the diagnosis of headache associated with cervical myofascial syndrome (section A11.2.5 of the classification supplement).
Diagnostic criteria for headaches associated with cervical myofascial syndrome are presented below and include the following disorders:
A. Headache and/or neck pain meeting criterion C
B. Identifies sources of myofascial pain in the neck muscles, including reproducible trigger points
C. There is evidence of a relationship (at least 2 of the following criteria)
1. One or both of:
a) headache developed in a temporary relationship with cervical myofascial syndrome
b) headache has significantly decreased or regressed after regression of cervical myofascial syndrome
2. Increased sensitivity to palpation of the neck muscles, consistent with the patient’s complaints of pain
3. Headache significantly decreases or regresses temporarily after injection of anesthetic into trigger points or after massage of trigger points
D. The headache does not meet the criteria for another form of headache to a greater extent.
The localization of myofascial trigger points gives a specific clinical pattern of headache. So, if the myofascial trigger point is located in the upper portion of the trapezius muscle, then pain is localized in the temporal region, cervical region and in the area of the angle of the lower jaw. The trigger, located in the sternal part of the sternocleidomastoid muscle, gives pain in the occipital region, periorbital region, and a little less often in the parietal region. A trigger in the clavicular part of the sternocleidomastoid muscle causes pain in the periauricular and frontal areas on both sides. Trigger points in the suboccipital muscles cause pain in the temporal, periauricular, and preiorbital regions. Triggers in the splenius muscles lead to pain in the parietal region [9].
In most cases, acute cervicalgia regresses completely, but in 10% of patients it can become chronic. Therefore, the main goal of treatment for acute neck pain is to relieve the pain syndrome as early and completely as possible.
Treatment of myofascial pain syndrome is carried out in several directions - effective pain relief with non-steroidal anti-inflammatory drugs (NSAIDs), reduction of pathological muscle tension (muscle relaxants), non-drug treatment methods (massage, manual therapy, acupuncture, etc.). The use of NSAIDs in the treatment of acute cervicalgia can quickly relieve pain. As a rule, NSAIDs are prescribed in a short course. When choosing an NSAID, attention should be paid to the safety of the drug. Long-acting drugs that have a long-lasting analgesic effect have an advantage. This allows you to reduce the frequency of administration, especially at night, and combine it with muscle relaxants.
NSAIDs include tenoxicam, which belongs to the group of cyclooxygenase-1 and -2 inhibitors. It has unique pharmacokinetic properties: it is rapidly absorbed - maximum plasma concentration is achieved within 2 hours, bioavailability is 100%. Moreover, the drug has a long half-life of 72 hours, which accounts for its prolonged analgesic effect. This drug has been studied quite well [13-18]. More than 150 clinical studies of its effectiveness and safety have been conducted, including long-term treatment of rheumatoid arthritis, osteoarthritis, and other rheumatic diseases. The effectiveness of tenoxicam in acute pain syndromes has also been proven in a number of controlled studies. The persistent effect of tenoxicam over 24 hours in acute pain syndromes was shown in a double-blind, placebo-controlled study. The effectiveness of tenoxicam in the treatment of acute cervicalgia has not been studied.
The purpose of the study was to study the effectiveness and safety of tenoxicam (Texamen) in the treatment of acute neck pain.
Material and methods
The criteria for inclusion of patients in the study were acute cervicalgia associated with myofascial syndrome, patient age 18-55 years. Exclusion criteria were significant structural changes in the cervical spine, radiculopathy, neck pain due to whiplash, and pain lasting more than 7 days.
We observed 50 patients, 42 women and 8 men with acute cervicalgia. Their average age was 42.2±6.8 years.
The sample was recruited from individuals attending the University Headache Clinic and by mailing information about the study. The control group consisted of patients from the database of the University Headache Clinic.
The main group, consisting of 30 patients, was prescribed tenoxicam at a dose of 20 mg once in the morning for 7 days. These patients were also recommended to undergo therapeutic exercises with elements of post-isometric relaxation for the neck muscles. The control group consisted of 20 patients who took muscle relaxants, as well as massage of the cervical-collar area and gymnastics with elements of post-isometric relaxation. Patients in the control group were not prescribed NSAIDs due to contraindications (peptic ulcer of the stomach or duodenum, exacerbation of gastritis, bronchial asthma, allergic reactions).
The main and control groups were comparable by gender and age.
When examining patients, complaints and anamnesis were analyzed, and a general clinical and neurological examination was performed. The severity of pain was assessed using a visual analogue scale (VAS) of 10 points. Myofascial syndrome was assessed by palpation algometry. Cutaneous allodynia was assessed using the ASC-12 scale [19]. Patients kept a headache diary, in which they noted the frequency, duration and intensity of pain, as well as associated symptoms.
The main criterion for the effectiveness of treatment was the dynamics of pain intensity (according to VAS). The remaining indicators served as additional performance criteria.
results
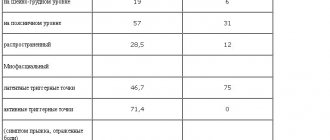
The cause of cervicalgia in 100% of patients was myofascial syndrome. Trigger points were noted in 90% of patients in the splenius muscles, in 84% in the trapezius muscle on one or both sides, in 52% in the internal oblique muscle, in 42% in the temporal muscles, in 24% in the sternocleidomastoid muscles. The duration of the exacerbation was 4.2 days (1-7 days). 76% of patients had previously had episodes of acute cervicalgia. Provoking factors for the development of cervicalgia were prolonged stay in an uncomfortable position (working at a computer) - in 62%, hypothermia - in 46%, stressful events - in 74%, sleep disturbances - in 28%. Patients included in the study had one of the forms of primary headache - episodic (44%) or chronic migraine (12%), episodic tension-type headache (33%). It is important to note that in 76% of patients, acute cervicalgia provoked an increase in frequency or occurrence of attacks of the existing primary headache.
Pain intensity was high in 62% of patients included in the study and moderate in 38%. The total score obtained by palpation algometry was 9.6±2.2. The average pain intensity was 7.2±1.7 points according to VAS. 58% of patients had pain at rest and all patients had pain with movement in the cervical spine. 42% had mild or moderate cutaneous allodynia in the head and neck area (5.8±1.2 points).
The dynamics of pain intensity in the group of patients receiving Texamen, as well as in the control group, are presented in Fig. 1
.
Figure 1. Dynamics of pain intensity (VAS scores) in the main and control groups.
Here and in Fig. 2: x axis - days of taking the drug; * — significance of differences between groups at p<0.05 level. It shows that significant differences between the groups were observed already on the 1st, 2nd and 3rd days of therapy: in the main group, the analgesic effect occurred faster. Thus, the introduction of NSAIDs, in particular Texamen, into the course of treatment of acute cervicalgia can significantly accelerate pain relief. Additional efficacy indicators were the proportion of patients with pain at rest and the proportion of patients with pain on movement in the cervical spine before the start of treatment, on days 1, 2, 3 and 7 after the start of therapy. There were no significant differences in the dynamics of pain at rest between the groups (Fig. 2)
.
Figure 2. Proportion of patients (in%) with pain in the cervical spine at rest and with movement in the main group compared to the control group.
* — significance of differences between groups during movement at the p<0.05 level. However, in the main group, pain regression during movement in the cervical spine occurred faster than in the group of patients receiving muscle relaxants in combination with therapeutic massage. Since texamen differs from other NSAIDs in its long half-life (72 hours), the analgesic effect was long lasting throughout the day. 16.6% of patients taking Texamen noted increased pain in the evening on the 1st day of use and 10% on the 2nd day. 23.3% of patients in the main group used an additional dose of the drug or another NSAID (ibuprofen) and a day triptan for headache relief.
In 86.6% of patients in the Texamena group and in 80% of patients in the control group, the pain syndrome completely regressed after 7 days of therapy ( p
=0.2). 73% of patients had headaches with less frequent attacks.
Significant regression of myofascial syndrome within 7 days of therapy was observed in 93% of patients in the main group and 95% of patients in the control group. Significant changes in the total score of palpation algometry were noted in the main group (from 9.3±1.8 to 3.1±0.6 points, p
<0.001) and in the control group (from 9.5±1.3 to 3.8±0.9 points,
p
<0.001).
The dynamics of regression of allodynia was more significant in the group of patients treated with Texamen (from 5.6±1.3 to 1.2±0.5 points) compared to the control group (from 5.9±1.1 to 3.7 ±0.9 points), p
<0.01. Subjective assessment of the effectiveness of therapy was “excellent” in 60% of patients, “good” in 33.3%, and “satisfactory” in 6.3%.
Treatment with Texamen was well tolerated by patients. Among the side effects, 23.3% of patients noted nausea, 13.3% - heartburn, 3.3% - diarrhea. Subjective assessment of therapy tolerability was “excellent” in 50% of patients, “good” in 26.6%, and “satisfactory” in 23.3%.
Discussion
This work is the first study of the effectiveness and safety of tenoxicam in the treatment of acute cervicalgia. The study showed that tenoxicam significantly accelerates the regression of pain compared to treatment with muscle relaxants in combination with therapeutic massage. Tenoxicam reduces pain during movement in the cervical spine. The drug can be used in a short course, with a single dose per day being sufficient. The use of tenoxicam in combination with kinesiotherapy made it possible to reduce the severity of painful muscle tension, comparable to that when taking muscle relaxants. Physical activity and kinesiotherapy are the most effective methods of treating cervicalgia, and prolonged analgesia with tenoxicam allows for sufficient physical activity. It should be noted that tenoxicam, in addition to its analgesic effect, has a pronounced anti-inflammatory effect. Apparently, due to the anti-inflammatory effect, the dynamics of regression of pain during movement was more significant in the main group compared to the group receiving muscle relaxants and therapeutic massage.
Of interest is the relationship between acute cervicalgia and the frequency of primary headache attacks, as well as clinical correlates of central sensitization (cutaneous allodynia). It has been shown that in patients with migraine there is hyperexcitability of the pathways connecting neurons of the trigeminal nucleus and neurons of the upper cervical segments of the spinal cord (the so-called trigeminocervical complex) [20]. This is due to a deficiency in the inhibitory effect of the periaqueductal gray matter in migraine. The presence of hyperexcitability of neurons of the trigeminocervical complex can explain the phenomenon of increased frequency or resumption of attacks of primary headache in acute cervicalgia. The results of the study suggest similar mechanisms for the development of increased frequency of tension-type headaches. Treatment of acute cervicalgia with tenoxicam also reduced the frequency of primary headaches and the severity of cutaneous allodynia, which is a clinical marker of central sensitization. This makes it possible to assume the presence of a central mechanism of action of tenoxicam. The central analgesic effect of tenoxicam was shown in the work of P. Braga et al. — the drug affects hyperexcitable neurons of the thalamus and reduces central sensitization [21].
An important aspect of the use of NSAIDs in the treatment of pain syndromes is their safety. For mild to moderate pain, local use of NSAIDs in the form of gels, creams, patches, etc. is recommended, which reduces the systemic effect of the drug. For high-intensity pain, oral and injectable forms are used. Medicines with a rapid onset of action and prolonged effect significantly reduce the need for repeated use of NSAIDs and the associated risk of side effects. The safety profile of tenoxicam allows the drug to be widely used for the relief of acute pain syndromes.