Remeron®
Pediatric patients
Remeron® should not be used in children and adolescents under 18 years of age. Suicidal behavior (suicide attempts and suicidal ideation) and hostility (primarily aggression, oppositional behavior and anger) were observed significantly more often in clinical trials in children and adolescents taking antidepressants compared with age-matched patients taking placebo. If, based on clinical need, a decision is made to use the drug, the appearance of suicidal symptoms in patients should be carefully monitored. In addition, there are no long-term safety data regarding growth, maturation, and cognitive and behavioral development in children and adolescents.
Suicide/suicidal thoughts or clinical worsening of the disease
Any depressive disorder itself increases the risk of suicidal thoughts and behavior. This risk persists until significant remission is achieved. Since improvement may not occur during the first few weeks of therapy (or longer), patients should be closely monitored until improvement occurs. Clinical observations indicate that the risk of suicide may increase in the early stages of recovery.
Patients who have a history of suicidal behavior, as well as patients who had significant suicidal intentions before starting therapy, are at increased risk of developing suicidal thoughts or suicide attempts and should be closely monitored. A meta-analysis of results obtained from placebo-controlled clinical trials of antidepressants in adult patients with mental disorders revealed a higher risk of suicidal behavior in patients receiving antidepressants compared with the placebo group in the age group under 25 years.
Patients receiving antidepressant therapy (especially patients at increased risk) should be closely monitored, especially at the beginning of therapy, and also in case of dose adjustment. Patients (and their caregivers) should be warned to promptly identify any signs of clinical deterioration, suicidal behavior, suicidal ideation, or unusual behavior, and to promptly report the occurrence of these symptoms to their physician.
Taking into account the possibility of suicide, especially at the beginning of therapy, the patient should be prescribed the smallest number of tablets of the drug in order to reduce the risk of overdose.
Bone marrow suppression
Psychiatry Psychiatry and psychopharmacotherapy named after. P.B. Gannushkina No. 07 2003
Clinical experience and medical statistics unanimously indicate that depression has gone beyond the scope of psychiatry. It is estimated that 20% of the world's population currently suffers from depression or has had a depressive episode in the past. Today, certain signs of depression are detected in 68% of patients at an outpatient appointment with a general practitioner; the number of neurological hospital patients suffering from depression reaches 80% [1]. Thus, the increase in the prevalence of depression indicates the predominance of psychogenic depression over organic depression, caused by an endogenous mental organic disease. This also indicates the predominance of mild and moderate forms of the disease, an increase in the number of patients with atypical or masked depression. Depression in neurological pathology may be a clinical manifestation of an organic neurological disease. Thus, the occurrence of depression is characteristic of parkinsonism, multiple sclerosis, stroke, and many degenerative diseases. However, the number of such patients is small. Depression has the most important pathogenetic significance in widespread chronic pain syndromes, autonomic disorders, dissomnias, and motivational-endocrine disorders, which served as a criterion for selecting clinical groups in this study. To successfully treat these extremely numerous forms of pathology, a neurologist must have the skills to diagnose depression, including atypical and hidden forms. Antidepressants are widely used in treatment; an adequate choice of drug is made taking into account the entire spectrum of its clinical action and side effects. Dosages and duration of treatment may differ significantly from those used in psychiatry [2]. Many antidepressants, starting with amitriptyline, follow a traditional path from psychiatry to neurology and then into therapy; receive new indications for their clinical use. Remeron (mitrazapine) is a new antidepressant that appeared in the Netherlands () in 1994. Currently, Remeron is used in many countries around the world, such as Austria, Brazil, Denmark, Finland, USA, UK, etc. By January 1998, more 750,000 patients have been treated with Remeron. The drug was mainly used in psychiatric clinics for the treatment of various types of depression of severe and moderate severity and showed high efficiency and good tolerability [3–5]. In 1998–2000 open studies of the therapeutic effectiveness of the drug were conducted in several psychiatric clinics in Russia. The mechanism of action of remeron is fundamentally different from previously known antidepressants and is designated as noradrenergic and specific serotonergic action (NASSA). The drug increases noradrenergic transmission by blocking alpha-2 adrenergic receptors. In addition, remeron increases serotonergic neurotransmission through two mechanisms: increasing the excitability of the serotonergic neuron signal and blocking alpha-2 heteroreceptors. Remeron specifically increases 5-HT1 mediator transmission by blocking 5-HT2 and 5-HT3 receptors. Unlike amitriptyline, it does not have cardiotoxic side effects, as well as effects associated with the effect on intraocular pressure and urination [6]. In addition, the selective action on serotonin receptors allows one to avoid the insomnia, anxiety, agitation, sexual dysfunction and nausea characteristic of selective serotonin reuptake inhibitors [7–10]. The purpose of the study was to study the effectiveness of the antidepressant Remeron in neurological practice. The following objectives were set: 1. Determination of the clinical effectiveness of remeron in the treatment of patients with chronic pain syndromes and insomnia. 2. Comparative assessment of the speed of onset of clinical and antidepressant effects. 3. Assessment of the anxiolytic effect of remeron, taking into account the high comorbidity (up to 70%) of depressive and anxiety disorders in neurological pathology. 4. Study of the level of attention during treatment with Remeron. 5. Determination of unwanted side effects of the drug. 6. Determination of optimal daily doses when using remeron in neurological practice. Research material
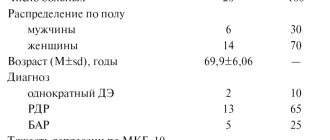
The study included 71 patients: 21 people (9 men and 12 women), average age 40.9 years, with chronic musculoskeletal pain; 30 people with headache, of which 10 people (9 women and 1 man), average age 39.5 years, with migraine, 20 people (17 women and 3 men), average age 36.6 years, with chronic tension-type headache (GBN); 20 people (17 women and 3 men), average age 45.7 years, with insomnia.
Research methods
1. Clinical and neurological examination (includes determination of the nature, intensity of pain syndromes, their frequency, as well as the nature of insomnia disorders). 2. Beck Depression Inventory and Hamilton Depression Inventory. 3. Spielberger test for assessing reactive and personal anxiety. 4. Scale for subjective assessment of the quality of night sleep. 5. Questionnaire to assess the severity of signs of vegetative dystonia syndrome (VDS). 6. Quality of life questionnaire. 7. Assessment of attention (according to the Munstenberg method). The daily dose of remeron was 15–30 mg, the drug was prescribed once 30–40 minutes before bedtime. The duration of therapy was 50 days. The study was carried out before the start of treatment, on the 7th day of therapy and at the end of treatment on days 43–50.
Chronic musculoskeletal pain
Back pain is one of the most common complaints when visiting a neurologist or therapist.
About 20% of the adult population suffer from recurrent back pain. In the majority of cases, pain goes away with treatment within 1 month, and in 4% it becomes chronic. More than 60% of patients with chronic dorsalgia have signs of emotional disorders of a depressive nature, which can be caused by both their existing pain syndrome and psychogenic causes. However, in any case, depression, by reducing the activity of antinociceptive systems, leads to increased pain syndrome, contributes to the chronification of pain and causes the low effectiveness of traditional treatment in these cases. The criterion for selecting patients for this study was chronic back pain of vertebrogenic (osteochondrosis, osteoarthritis, functional blocking of intervertebral joints) and myofascial origin. Among them, lumbar pain was observed in 57% of patients, cervicothoracic pain – in 15%, widespread pain syndrome – in 28% of patients. The pain was almost daily, the duration of the pain syndrome ranged from 4 months to 18 years. The main part of the study group consisted of patients with reflex muscular-tonic and myofascial pain syndromes against the background of spinal osteochondrosis, static-locomotor disorders, developmental anomalies of the musculoskeletal system, reversible functional blocks; some patients had residual effects of radiculopathy. Vertebrogenic changes were detected in 42% of patients, according to neuroimaging data. Patients received Remeron 30 mg once daily for 50 days. In addition, non-medicinal treatment methods were used: physiotherapy, massage, exercise therapy, and patients also did individually selected gymnastics based on self-postisometric relaxation techniques, according to a schedule established by the doctor. Treatment was carried out on an outpatient basis. Thus, patients with chronic musculoskeletal pain received complex treatment; they had previously used non-drug methods in various combinations without significant clinical effect; the prescription of the antidepressant Remeron was new. 16 people completed the full course of treatment; 3 did not show up for re-examination, and in 2 patients Remeron was discontinued for medical reasons. The therapy contributed to a significant reduction in pain intensity on average in the group from 4.86 to 1.86 points on the visual analogue scale (VAS). According to this indicator, the treatment effect can be assessed as excellent in 43% (pain reduction over 75%), good in 32% (pain reduction by 50–75%), satisfactory in 12.5% (pain reduction by 25–50%) , therapy was ineffective in 12.5% of patients. In a clinical study of patients at the end of the course of treatment, a decrease or complete reduction of reflex muscular-tonic syndrome in significant muscle groups, the transition of active myofascial trigger points to a latent state was determined, an increase in the motor capabilities of patients, a decrease in functional postural changes, and some optimization of the motor stereotype were noted ( Table. 1
). Residual effects of radiculopathy and dysfunction of the sacroiliac joints did not reveal significant changes.
The reduction in chronic musculoskeletal pain as a result of the treatment contributed to an improvement in the quality of life of patients: before treatment it was reduced by 41%, after it – only by 17% (p <0.05). In a psychometric study conducted before the start of complex therapy, emotional disorders were identified in patients (depression and anxiety, night sleep disturbances, decreased level of attention according to the Munstenberg test), and the average score on the vegetative questionnaire was significantly higher than that of healthy subjects. After the course of treatment, statistically significant changes were observed in the improvement of the quality of night sleep (before treatment – 17.57 points; after treatment – 21.9 points, p<0.05), reduction in depressive symptoms according to the Beck test (before treatment – 16.52 points, after – 8.94 points, p<0.05) and an increase in the level of attention (the percentage of errors before treatment was 33.25, after treatment – 25.0, p<0.05). Thus, complex therapy of chronic musculoskeletal pain, which included the antidepressant Remeron, reduced the severity of reflex muscular-tonic and myofascial syndromes, which led to an increase in the motor abilities of patients, an improvement in their quality of life, and also reduced the severity of depressive symptoms. Considering the sedative effect of the drug, it was important that there were no disturbances in attention during the treatment.
Headache
Antidepressants have long been successfully used in the treatment of headaches.
In the chronic form of tension-type headache, they are the first-line drugs, which is undoubtedly due to the leading role of depressive disorders in the pathogenesis of this type of headache. In case of migraine, the occurrence of depressive or anxiety-depressive disorders in a patient under the influence of emotional stress can significantly influence the course of the headache, causing an increase in migraine attacks, causing attacks of panic migraine (a combination of migraine hemicrania with a panic attack), and in some cases leading to its transformation into chronic daily headache [1, 2]. In this regard, antidepressants are used in the preventive treatment of migraine, the goal of which is to reduce the frequency of headache attacks, reduce comorbid psychovegetative disorders, and improve the quality of life. In the preventive treatment of migraine with frequent attacks, high effectiveness of IGB was noted in 70%, average – in 30%. In the treatment of chronic tension-type headache, high efficiency was also observed in 60%, average - in 20%, low - in 20%. An experimental psychological study of patients was carried out before the start of antidepressant therapy (day 0), a week after the start of treatment (day 7) and after its completion (day 50). It should be noted that initially, in patients with migraine, the severity of depression, both according to subjective assessment (Beck Self-Esteem Scale) and objective assessment (Hamilton Scale), was of insignificant severity. Indicators of the level of both reactive and personal anxiety exceeded normative data ( Table 2
). In patients with chronic tension-type headache, depression and anxiety were significantly more pronounced, which is fully consistent with literature data [1].
A decrease in anxiety and depressive disorders was noted within 1 week after the start of therapy. At the end of the treatment course, both groups experienced a significant decrease in levels of both anxiety and depression. Patients in both groups had polymorphic autonomic disorders before starting antidepressant therapy. The total score on the questionnaire for the severity of vegetative dystonia syndrome before treatment in both groups exceeded the indicators of healthy subjects: migraine - 41.4, tension-type headache - 46.5, control group - no more than 25 points (p <0.05). During treatment, patients with migraine showed a decrease in the severity of vegetative dystonia syndrome after 7 days, and by the end of the course it reached statistically significant values (migraine - 31.4 points). With HDN, slightly more pronounced phenomena were noted before treatment, and after the course, their dynamics were insignificant (THN - 40.2, p < 0.05). Most of the headache patients we studied complained of disrupted night sleep. These complaints were objectified by a sleep quality questionnaire. Treatment with Remeron normalized nighttime sleep in both groups, positive dynamics were noted after a week of treatment, a significant increase in indicators for migraine and tension-type headache to the level of healthy subjects was noted on the 50th day of treatment. Attention indicators were tested using the Munstenberg test, where all correct answers within 2 minutes were taken as 100%. Our study showed that remeron not only does not cause a decrease in the level of attention, but even, on the contrary, patients become more attentive by the end of treatment. On the image
The dynamics of attention indicators and their significant improvement by the 50th day are shown.
The impact of headaches on the quality of life of patients and its changes during treatment is demonstrated by the quality of life test. In the study before the start of therapy, the greatest decrease in quality of life was noted by patients with chronic tension headaches by 54.6%, with migraine by 40%. At the end of the course of therapy, the quality of life of patients in both groups significantly improved compared to the indicators before treatment, and the percentage of decrease in quality of life decreased more significantly in patients with chronic tension-type headache (migraine - 29.7% tension-type headache - 29.4% p<0.05. ) Considering the fact that patients received different dosages of remeron, for chronic tension-type headache, an analysis of the clinical effectiveness of the drug was carried out depending on the dose: 15 or 30 mg. The most important clinical indicator was headache intensity according to the VAS scale; its dynamics turned out to be similar in both groups (before treatment: 15 mg – 8, 30 mg – 7.7 points, after treatment: 15 mg – 3, 30 mg – 2.7 points).
The dynamics of psychovegetative indicators are presented in table. 3
.
Noteworthy is the initially higher level of depression on the Beck scale and a higher level of reactive anxiety in the group taking 30 mg. After a 50-day course of therapy with Remeron at a dose of 30 mg, a relatively greater significant decrease in depression according to the Beck test and reactive anxiety was noted. Quality of life also showed more positive changes when taking a higher dose of the drug. Thus, it can be noted that the antipain effect of different doses of remeron was the same, however, the anxiety-depressive syndrome regressed, and the quality of life improved to a greater extent when taking 30 mg.
Insomnia
Insomnia is a basic pathology of sleep medicine.
The high prevalence [11] of night sleep disorders (28–45% of the population) and the insufficient effectiveness of modern hypnotics [12] suggest a constant search for the most effective hypnotics. Another important problem is depression, the high prevalence of which can take 2nd place after coronary heart disease among the causes of disability. The close connection between night sleep disorders and depression [7, 13, 14] forces the use of antidepressants both for the treatment of depressive disorders and for the normalization of concomitant night sleep disorders [9]. Antidepressants are a pathogenetic method of treating insomnia caused by depressive disorders. As is known, remeron, being a representative of a new class of antidepressants with noradrenergic and specific serotonergic activity, has a hypnotic effect [4, 15], however, the effectiveness and safety of taking remeron in patients with insomnia in outpatient neurological practice remain not fully studied. The study involved patients with complaints of nighttime sleep disturbance, regardless of the etiological factor, who had not taken any psychotropic drugs with a hypnogenic effect less than 2 weeks before the start of the examination. 20 patients with insomnia (17 women and 3 men) were studied; the average age of the patients was 45.7 years. The average duration of night sleep disturbances in the group was about 5 years. The average score on the Hamilton Depression Rating Scale was 16.5. The presence of depression was also confirmed by the Beck Self-Esteem Scale (20.8 points). These results indicate the presence of depression in the studied group of patients with insomnia, the severity of which in most patients was mild or moderate. Depression was accompanied by anxiety disorders, the presence of which was determined both clinically and using the Spielberger test: the average level of reactive anxiety was 40.0 and personal anxiety was 42.4. Assessment of the quality of life questionnaire before treatment revealed a relatively low level (53.9 points out of 100 possible). The autonomic questionnaire indicates the presence of autonomic disorders (33.7 points); in only 1 patient, autonomic disorders did not reach clinically significant values (above 25 points) and amounted to 17 points. The Munstenberg attention test revealed that patients detected only 61% of words (39% errors). The subjective picture of insomnia, according to the sleep questionnaire (assessment was made on a 5-point system, the higher the score, the better the sleep), was characterized by difficulty falling asleep, insufficient sleep duration, a large number of night awakenings, low quality of sleep and well-being after waking up in the morning, almost in the same degree of expression. Treatment of patients showed that the subjective assessment of sleep has a positive trend already during the first week of treatment for almost all subjective characteristics with the exception of the number of dreams and the quality of morning awakening, which did not undergo significant changes. The obtained data are presented in table.
4 .
The study of the severity of anxiety and depressive disorders, the severity of SVD, and the level of attention a week after the start of treatment did not reveal any significant dynamics of indicators. Analysis of subjective sleep indicators showed that by the end of the 2-month course of treatment, most indicators of subjective sleep assessment had significantly higher scores (better quality). Analysis of the dynamics of psychovegetative indicators after a 2-month course of treatment showed a significant decrease in depression according to the Beck test and reactive anxiety according to the Spielberger test. There were no significant changes in the level of attention and severity of autonomic disorders in the group as a whole, and at the same time, the quality of life of the patients increased significantly. Half of the patients (10 people) with insomnia (group 1) took 15 mg of remeron and group 2 (10 people) took 30 mg. An analysis of the effectiveness of the drug depending on the prescribed dose on the subjective characteristics of night sleep was carried out. The total score of subjective assessment of the quality of night sleep in both groups significantly exceeded the values before treatment, which indicated the effectiveness of both 15 mg and 30 mg of the drug in the treatment of insomnia. However, when the drug was prescribed at a dose of 30 mg, a better quality of morning awakening, a decrease in the number of night dreams and a decrease in the number of night awakenings were noted.
Tolerability of remeron when used in neurological practice
The majority of patients tolerated treatment with Remeron well, noted a pronounced clinical effect of the drug and, despite some unwanted side effects, completed the full course of treatment, which was accompanied by an improvement in quality of life. Only in 3 patients out of 70 people (2 patients with chronic musculoskeletal pain and 1 patient with insomnia) the drug was discontinued due to a rapid and pronounced increase in body weight, the occurrence of a hypomanic state with disturbances in night sleep and significant increases in blood pressure in the first 3 day of treatment. Side effects observed in patients with neurological pathology who completed a full (50 days) course of treatment with the antidepressant Remeron could be divided into three groups: 1) drowsiness and lethargy; 2) dry mouth, nausea and feeling of lightheadedness; 3) increased appetite and weight gain. It should be noted that side effects groups 1 and 2 were short-lived and were observed for 1 or 2 weeks at the beginning of taking the drug. However, it was they who did not allow increasing the dose of the drug to 30 mg in patients who continued to work during treatment. Only mild dry mouth remained during the entire course of treatment. The most consistent side effects included increased appetite and weight gain, observed in 30% of patients. It should be noted that an increase in body weight was observed mainly in patients receiving 30 mg of remeron per day. Patients with insomnia were warned in advance about a possible increase in body weight, an increase in appetite and a decrease in general physical activity (if drowsiness occurs), and therefore they were advised to carefully monitor their diet. This made it possible to reduce the number of patients with weight gain from 30% in the group as a whole to 5%.
conclusions
1. Remeron has a pronounced analgesic effect in patients with chronic musculoskeletal pain and can be used in complex therapy along with non-drug treatment methods - massage, manual therapy, exercise therapy. 2. Remeron has been shown to be highly effective in the treatment of primary headaches – migraine and chronic tension-type headache. 3. Remeron has a pronounced hypnogenic effect and significantly improves the subjective characteristics of night sleep - it shortens the time of falling asleep, reduces the number of night awakenings and dreams, increases the duration of night sleep and, most importantly, improves the quality of morning awakening. 4. The psychotropic and hypnogenic effect of the drug occurs quickly - after just 1 week of treatment. 5. Considering the clinical properties of the antidepressant Remeron, it may be the drug of choice in the treatment of chronic pain syndromes accompanied by severe sleep disturbances and anxiety disorders. 6. In outpatient neurological practice, it is possible to use a half dose of 15 mg, which can significantly reduce the unwanted side effects of the drug and improve its tolerability, without significantly reducing the clinical effectiveness for this pathology. 7. To avoid a significant increase in body weight during the course of treatment with Remeron, the patient should be warned about a possible increase in appetite, and he should be advised to monitor his diet more closely. 8. The drug does not have a negative effect on the cognitive abilities of patients during treatment. On the contrary, in a number of cases it improved attention indicators, apparently due to the reduction of anxiety and depressive disorders.