How does infection occur and who is at risk?
The routes of infection with polio mainly come down to the penetration of the virus through the digestive tract - if water, food or hands have previously come into contact with contaminated substances. For example, feces of a sick person get into a pond, and then when swimming, the patient gets the virus along with the contaminated water. The causative agent of the disease is poliovirus.
You can become infected through water, food, dirty clothes, etc. At risk are:
- children under 7 years old. Poliomyelitis occurs much more often in children than in adults;
- Pregnant women;
- people with very weakened immune systems. This can be facilitated by various diseases, as well as disorders at the endocrine level, periods after operations, etc.;
- people suffering from immunodeficiencies.
The risk of infection is higher during the warm season: summer or autumn. The virus is very tenacious; in a humid environment it can live up to 4 months.
Victory of Soviet scientists
The fate of the live polio vaccine and its further role in global epidemiology was decided by Sabin’s meeting with the Soviet scientist Mikhail Chumakov. At that time, Mikhail Petrovich was in America - together with his wife and colleague, he was sent to the States to exchange experiences. Chumakov quickly seized on this theory, and after some time several thousand doses of polio vaccines were brought to the USSR.
The drug, which had not been fully tested, was tested on everyone - myself, relatives, colleagues. Understanding perfectly well the danger of such experiments, none of my relatives objected. Everyone knew that this was necessary to protect their children from a terrible disease.
Production of live Sabin vaccine has begun at the Polio Institute. However, the Ministry of Health did not approve of this idea - “if the drug was abandoned in America, why should we test and produce it”? Chumakov decided to take a risk and carried out a successful vaccination, after which the polio epidemic was ended in just a year and a half, and the vaccine was exported to more than 60 countries.
Symptoms of polio and course of the disease
The polio virus causes the following symptoms:
- signs of intoxication: nausea, vomiting, diarrhea, rash;
- cold-like disorders: cough, runny nose, sore throat, difficulty breathing and swallowing;
- fluctuations in blood pressure, fatigue, general poor health, headache;
- in rare cases - various types of paralysis that can lead to the death of the patient.
It is important to note that in 90% of cases, polio has no symptoms and does not affect the nervous system. And in 10% of cases there are very severe forms, involving inflammation of the membranes of the brain - with serious consequences, even fatal.
The incubation period of polio is quite short - it does not exceed 5 days. In this case, recovery in the case of a mild form occurs within 3 days. However, as we have already said, there are also complex forms - they are quite rare, but extremely dangerous. In this case, treatment may last for months, years, or may be completely useless.
Are you experiencing symptoms of polio?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Preparalytic stage
It is characterized by a rather acute onset, high body temperature, general malaise, headache, gastrointestinal disorders, rhinitis, pharyngitis. This clinical picture persists for 3 days, then the condition normalizes for 2-4 days. Afterwards there comes a sharp deterioration in the condition with the same symptoms, but more pronounced intensity. The following signs are included:
- pain in legs, arms, back;
- decreased reflexes;
- increased sensitivity;
- decreased muscle strength;
- convulsions;
- confusion;
- excessive sweating;
- spots on the skin;
- "goose pimples".
How is polio diagnosed?
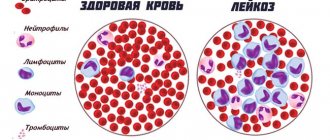
If obvious symptoms of polio occur, the patient is admitted to an infectious diseases hospital, where an infectious disease specialist takes over the examination. To understand what the reason is, they carry out a number of manipulations, be sure to investigate:
- blood and urine tests;
- materials from the nasopharynx;
- feces;
- cerebrospinal fluid.
All this allows us to find out which pathogen caused the disease and make a correct diagnosis.
Paralytic stage
This is the stage when the patient suddenly suffers from paralysis (within a couple of hours). This stage lasts from 2-3 to 10-14 days. Patients during this period often die from severe respiratory and circulatory disorders. It has the following symptoms:
- flaccid paralysis;
- defecation disorders;
- decreased muscle tone;
- limitation or complete absence of active movements in the limbs and body;
- damage mainly to the muscles of the arms and legs, but the muscles of the neck and torso may also be affected;
- spontaneous muscle pain syndrome;
- damage to the medulla oblongata;
- urinary disorders;
- damage and paralysis of the diaphragm and respiratory muscles.
During the recovery period of polio, which lasts up to 1 year, tendon reflexes are gradually activated and movements in individual muscle groups are restored. The mosaic nature of the lesion and uneven recovery causes the development of atrophy and muscle contractures, growth retardation of the affected limb, the formation of osteoporosis and bone tissue atrophy.
The residual period, or the period of residual effects, is characterized by the presence of persistent paresis and paralysis, accompanied by muscle atrophy and trophic disorders, the development of contractures and deformation in the affected limbs and parts of the body.
How the disease is treated in Moscow
Treatment of polio is carried out in an infectious diseases hospital and involves an integrated approach, including:
- strict bed rest. The patient should remain calm, in a favorable environment;
- protection of paralyzed muscles. For this purpose, special splints can be applied;
- physiotherapy. This includes physical therapy, swimming in the pool under the supervision of a trainer, and massage. This also includes electrical stimulation, paraffin applications, UHF therapy and much more. The procedures are aimed at stabilizing the nervous system, helping paralyzed muscles;
- Ventilation Clinical guidelines for polio also suggest major life-sustaining interventions. The use of a mechanical ventilation device is indicated for patients whose paralysis has affected the respiratory system, and therefore threatens respiratory arrest;
- use of special medications.
It is very important that a polio patient be closely monitored, especially when the disease is progressing or not showing significant improvement.
There were no effective treatments
How did they try to treat polio? At the end of the 19th and beginning of the 20th centuries, when the disease acquired the character of epidemics, the sick ended up in hospitals for a long time: for months and even years. Unfortunately, the consequences of paralysis in most cases remained for life and could not be treated.
If the virus affected the muscles of the diaphragm, patients were placed in so-called “iron lungs” - boxes in which pressure changes helped the lungs work.
The worst thing is that this treatment did not help. Children and adults infected with the virus lived and died while shackled in a metal structure. After spending a year in such a chamber, the patients' respiratory muscles atrophied; they could not even be connected to modern artificial stimulation devices. By the way, there are still people who use “iron lungs”; unfortunately, it is not possible for them to return to normal life.
Prevention of polio
The main preventive measure is vaccination of children, which is carried out at an early age and then again. There is a special vaccination calendar, on the basis of which pediatricians recommend undergoing this procedure. When vaccinated correctly, lifelong immunity and resistance to poliovirus are developed.
If we talk about the prevention of polio at the household level, it means:
- refusal to swim in dirty bodies of water that are not suitable for this;
- compliance with personal hygiene rules;
- refusal of potentially dangerous products. In this sense, raw milk is undesirable - a pathogen is often found in it;
- Quarantine measures if a child with a disease is detected in a children's group. At the same time, all objects and things are processed and disinfected.
Now polio is quite rare - this is due to centralized vaccination, thanks to which children from an early age develop immunity to the polio virus, and therefore calmly tolerate contact with it.
Features of the childhood vaccination scheme in Russia and the world
There are two types of polio vaccines:
- IPV, i.e. inactivated polio vaccine (with killed virus),
- OPV, i.e. oral polio vaccine (live, with a weakened virus, so-called attenuated).
Live may contain one individual or a combination of strains of the 1st, 2nd or 3rd type of poliovirus types. And the inactivated one can be single-component (only for polio) or be part of combination drugs for several infections.
IPV is administered intramuscularly or subcutaneously and is considered safer than OPV because... does not carry any risk of developing vaccine-associated paralytic poliomyelitis. Possible side effects after IPV injection: redness (0.5–1%), induration (3–11%) and soreness (14–29%) at the injection site.
OPV, unlike IPV, comes in the form of drops and is administered orally, that is, through the mouth. The effectiveness of OPV is close to 100%. The main advantage of the live vaccine is the ability to form a local immune response in the intestines, which makes it impossible for wild polioviruses to multiply in the body of vaccinated children.
ON A NOTE! A vaccinated child releases the vaccine virus into the environment for up to several weeks. The vaccine virus can be transmitted from a child vaccinated with OPV to unvaccinated children through dirty toys and dishes, protecting them too. Scientists have also identified an interesting effect of OPV vaccination - the development of nonspecific immunity, which reduces mortality in general.
The main disadvantage of OPV is the existing possibility of a complication - vaccine-associated polio (VAPP), which is no different from wild infection. The disease is rare (one child out of 1-1.5 million vaccinated children and one out of 14 million contacts). At risk are children who are not vaccinated at all, with an irregular schedule or immunodeficiency, but who are in contact with recently vaccinated people, as well as those who immediately received a live drug without prior administration of an inactivated one.
ATTENTION! Even one dose of an inactivated drug before vaccination with a live virus eliminates the occurrence of vaccine-associated paralytic poliomyelitis.
Scientists have long known about the nuances of these vaccines, and have found a solution. To reduce the risk of VAPP, polio is first vaccinated using IPV, and only then a live vaccine (OPV) is included. This tactic has been in effect according to WHO recommendations for all countries since 2016, and has existed in Russia since 2008. In our country, such sequential vaccination (2 doses of IPV + 1 dose of OPV, subsequent revaccination with OPV) helped reduce the number of VAPP cases by 2.6 times.
Isolation of vaccinated children is an important condition for prevention. Children who have been vaccinated with an attenuated vaccine should be isolated from those who have not been vaccinated or who have been vaccinated less than three times. This requirement is enshrined in the legislation of the Russian Federation in the Decree of the Chief Doctor of Russia, and applies to all institutions in which children are located.
The isolation period is 60 days after vaccination. How this happens, who needs to be isolated and from whom - these issues are resolved on the spot by parents, educators, doctors, and so on. Despite the fact that vaccine-associated polio is not so common, ignoring prevention recommendations, according to experts, can lead to a new increase in incidence and outbreaks of the epidemic.
Also in 2016, they stopped using three-component OPV, because the 2nd type of wild poliovirus was completely exterminated. It was this component that caused a greater risk of VAPP (40% of cases). The vaccine used in Russia now contains not 3, but 2 strains (hence the “Bi” particle (lat. bi... two (x)) in the name: BiVac-Polio).
So, in Russia, vaccination against polio occurs according to the following scheme:
1. IPV vaccination is given twice by injection at 3 and 4.5 months; 2. third vaccination - in six months with a live vaccine in the form of drops (OPV); 3. at 18 and 20 months, the first and second revaccination with a live vaccine (OPV again); 4. at the age of 14, the third revaccination with live vaccine (OPV) is carried out.
At the same time, for some children, according to indications, all vaccinations are given with an inactivated vaccine.
It is important to note that in the case of polio vaccination, there are often cases of schedule violations when children ultimately do not receive all vaccinations according to the approved schedule. This may be due to the child’s illness (medical issues), or to the reluctance or doubts of the parents (“to do it or not”). Sometimes parents purchase the wrong vaccine; for example, they prefer to vaccinate against several diseases at once with a combination drug. In this case, it turns out that the child is not vaccinated with a live vaccine a sufficient number of times.
Questions and answers on the topic of polio
Is it necessary to get the OPV vaccine?
Parents have the opportunity to refuse such vaccination - they can write a written refusal and not undergo this procedure. However, doctors warn against such a decision: remember that if 10% of children get sick, the consequences will be irreversible, and for some children such a refusal will cost their lives. Currently, OPV vaccination is the only way to be 100% protected against the polio pathogen.
How is the polio vaccine given?
The vaccination is done twice, starting from the age of three months. The injection is given intramuscularly and contains the virus killed by formaldehyde.
How effective is vaccination against this disease?
Since the active fight against polio (1988), thanks to vaccination, it has been possible to reduce the number of cases from 350 thousand people per year to 359 cases (in 2014). These data speak for themselves: after receiving the vaccine, the disease becomes harmless and no longer threatens the person.
Development of the first vaccine
The first polio vaccine appeared in early 1952. Its creator was virologist Jonas Salk from the United States. By that time, the disease had spread throughout the globe - in America alone, during 1952, the virus killed more than 3,000 people, and left more than 21,000 paralyzed.
Dead viruses were taken as the basis, since by the time the polio vaccine was created, Jonas Salk was developing a flu vaccine, and while testing the drug on patients, he noticed that killed viruses also triggered a response from the immune system. Almost 20,000 monkeys were involved in the search process. However, the scientist understood that this was not enough, and for large-scale production it was necessary to somehow reproduce the pathogen in test tubes. To implement the idea, Salk took advantage of the achievements of Frederick Robbins, John Enders and Thomas Weller.
The scientist first administered the resulting drug to himself and his loved ones – his three sons and his wife. What was happening was recorded on photos and video cameras - these materials were later used to reassure the population during mass immunization. It turned out that the vaccine was safe and effective, and already in 1954, the untested composition was administered to five thousand school students. Not a single child got sick after vaccination.
Cultivation of polioviruses
Cultivation of polio viruses is carried out on cultures of monkey kidney cells, human embryos, fibroblasts, continuous cultures of HeLa cells, etc. In the presence of the virus, cell lysis is observed (cytopathic effect).
Rice. 9. Poliomyelitis in a child. Spinal shape. The muscles of the upper and lower extremities are affected.
Effectiveness of vaccination
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. Following widespread use of the polio vaccine, the incidence of the disease fell sharply in many industrialized countries. Since 1988, the number of polio cases has decreased by more than 99%, from 350,000 to 73 cases reported in 2015, according to WHO.
Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed. This decrease was the result of global efforts to eradicate the disease. In fact, this is the largest peacetime mobilization of people in history.
In 2014, only three countries in the world (Afghanistan, Nigeria and Pakistan) remained endemic for polio; in 2015, Nigeria was removed from this list, while in 1988 the number of such countries exceeded 125. Failure to eradicate polio in these remaining persistent foci could result in up to 200,000 new cases of the disease occurring annually worldwide within 10 years. The world can be freed from the threat of polio if everyone commits to it - from parents to government workers and from political leaders to the international community.
Forecast for life
Mild forms of poliomyelitis (occurring without damage to the central nervous system and meningeal) pass without a trace. Severe paralytic forms can lead to permanent disability and death.
Thanks to many years of targeted vaccine prevention of polio, the structure of the disease is dominated by mild inapparent and abortive forms of infection; paralytic forms occur only in unvaccinated individuals.
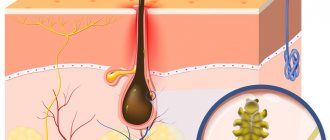
Reproduction of poliovirus
Poliomyelitis pathogens enter the child’s body through the mucous membranes of the digestive tract and nasopharynx. They have an affinity for nerve cells, so they quickly reach the spinal cord and brain with the bloodstream and settle in the gray matter. The target cells are motor neurons of the anterior horns of the spinal cord and medulla oblongata.
Stage 1. Polio viruses attach to the cell membrane of target cells. Their adsorption occurs mainly on lipoprotein receptors of cells.
Stage 2. The poliovirus genome enters the target cell by endocytosis or injection of RNA through its cytoplasmic membrane.
Stage 3. Destruction of the virus capsid and release of the replicative form of RNA, which is the matrix for the synthesis of messenger RNA and RNA of future virions.
Stage 4. Assembly of virions and reproduction of viral particles (reproduction) occur in the cytoplasm of the target cell. First, a single giant polypeptide is synthesized, which is cut into fragments under the influence of proteolytic enzymes. The capsid is built from some fragments (capsomeres), others are internal proteins, and others are virion enzymes. Several hundred virions are formed in each cell.
Stage 5. Destruction (destruction) of cells and release of virions to the outside.
Rice. 7. Pathogens of polio (view under an electron microscope).
Treatment
The initial diagnosis is made by a pediatrician or emergency physician. Further observation is carried out by an infectious disease specialist and a pediatric orthopedist. Depending on the nature of the lesion, a neurologist, cardiologist, gastroenterologist and other specialists may be involved.
The development of clinical symptoms similar to polio requires immediate hospitalization of the child. The first thing to do is to ensure bed rest and complete rest. It is necessary to fix the limbs in the correct physiological position. Prescribe a high-calorie diet, taking ascorbic acid and B vitamins. Drug therapy is symptomatic (palliative) therapy aimed at eliminating individual manifestations of the disease.
All research should be kept to a minimum. It is necessary to protect the patient from physical and psychological stress. There is no specific treatment for polio. As a rule, the patient remains in isolation in the hospital for 40 days. Then comes the recovery period.
An important role is played by rehabilitation therapy carried out by an orthopedist, physical therapy doctor, physiotherapist and other specialists. In some cases, surgery may be required to correct residual deformities. The rehabilitation program includes physical therapy courses, water treatments, massage, electrical myostimulation, and physiotherapy. Spa treatment is recommended.