Tranquilizers are a group of psychotropic drugs with an anti-anxiety effect, relieving anxiety and internal tension, anxiety, tremors and muscle tension of neurotic origin, and a feeling of fear. Some drugs in this group, in addition to their normalizing psycho-emotional state and nighttime sleep effect, can have a tonic effect.
Among tranquilizers (from the Latin tranquillo - to calm down) there are typical and atypical ones, which do not have pronounced non-core effects and do not cause dependence when taken for a long time. Based on their chemical structure, anxiolytics are divided into benzodiazepine derivatives (chlordiazepoxide, diazepam, phenazepam, oxazepam, medazepam, midazolam) and drugs of other chemical groups (meprotane, benactizine, phenibut, mebicar, benzoclidine).
The pharmacodynamic activity of all anxiolytics comes down to five main components: sedative, anti-anxiety, hypnotic, relaxant and anticonvulsant. Each specific drug has its own degree of severity of a particular therapeutic effect, which determines its clinical use (for example, in psychiatry, neurology, cardiology, gastroenterology, otolaryngology, anesthesiology).
Anxiolytics are prescribed to relieve states of agitation (1) and asthenia (2) accompanying various mental disorders:
- anxiety, panic, fear, irritability, dysphoria, problems with going to bed, decreased sleep duration, autonomic lability, autonomic crises;
- asthenia, chronic fatigue, hypochondria, problems with attention and remembering information, decreased intellectual activity, weakness, fatigue, lethargy, apathy, irritability, lack of vigor after sleep.
As a rule, the above conditions occur against the background of the following mental disorders:
- neuroses and neurosis-like conditions (F40–F48);
- behavioral disorders in children and adolescents (F91);
- personality disorders (F60–F69);
- fears and phobias (F40);
- insomnia (F51);
- panic attacks (F41);
- generalized anxiety disorder (F41.1);
- mixed anxiety and depressive disorder (F41.2);
- schizotypal disorder (F21);
- acute psychoses (F23, tranquilizers are prescribed as part of complex therapy);
- anorexia (F50.0–F50.1 and bulimia (F50.2);
- psychosomatic diseases (F04–07; F44.4–F44.7; F45; F50–F53).
In the practice of a neurologist, tranquilizers can be prescribed, for example, when states of agitation and asthenia occur due to traumatic brain injuries, strokes accompanied by increased muscle tone, epilepsy, and spinal osteochondrosis. Other somatic doctors prescribe anxiolytics for the treatment of functional disorders in the gastrointestinal tract (gastroenterologist), cardiovascular system (cardiologist), urinary system (gynecologist, urologist), withdrawal states and consequences of organic damage to the central nervous system (narcologist, toxicologist).
Mechanism of action of tranquilizers
The therapeutic mechanism of action of tranquilizers is the ability to influence the interneuronal transmission of nerve impulses in the diencephalon (intermediate) and spinal cord, reduce the activity of subcortical areas of the brain, reduce the level of dopamine and norepinephrine, as well as processes in the GABA systems of the brain, and block cholinergic receptors.
A feature of the therapeutic effect of tranquilizers is a calming effect on the central nervous system, excluding a pronounced antipsychotic effect. Therefore, they are widely used for mild (reversible) disorders of the central nervous system as an alternative to antipsychotic drugs.
The mechanism of action of tranquilizers depends on their chemical structure. Among anxiolytics, six classes of organic substances can be distinguished, represented by main chemical groups (according to the Anatomical Therapeutic Chemical Classification of Medicines, ATC):
- benzodiazepine derivatives;
- diphenylmethane derivatives;
- carbamates;
- dibenzo-bicyclo-octadiene derivatives;
- azaspirodecanedione derivatives;
- other anxiolytics.
The targets of anxiolytics are the following brain structures:
- limbic system of the hypothalamus;
- reticular formation of the brain stem,
- thalamic nuclei.
To date, the mechanism of action of tranquilizers of benzodiazepine derivatives has been well studied. Benzodiazepine receptors are involved in biochemical processes associated with GABAergic inhibition at all levels of the central nervous system. The versatile activity of tranquilizers is determined by their effect on various types of benzodiazepine receptors, thus allowing them to have anxiolytic, sedative, hypnotic, muscle relaxant and anticonvulsant effects.
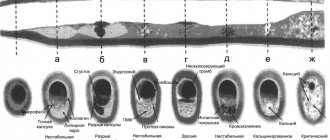
Rice. 1. The mechanism of action of tranquilizers.
Anxiolytic (anti-anxiety) effect
The main task of tranquilizers is to provide an anxiolytic (anti-anxiety) effect: relieve anxiety, anxiety, fear (antiphobic effect), reduce emotional stress. In addition, anxiolytics help to cope with obsessive thoughts and hypochondria, irrational worries about one’s own health.
Tranquilizers are not antipsychotic drugs, so they do not relieve hallucinations, delusions, affective and productive disorders. Their therapeutic effect is aimed at other structures in the nervous system that are not responsible for the occurrence of such symptoms.
Sedative (calming) effect
Anxiolytics have a sedative (calming) effect, which is expressed in a decrease in hyperactivity, psychomotor excitability, speed of motor and mental reactions, and concentration. The sedative effect can be considered complementary to the anxiolytic.
Hypnotic effect
In case of sleep disorders (difficulties in falling asleep, in the presence of superficial sleep, sensitive to external stimuli, as well as short sleep, insufficient for restoration of strength), which, as a rule, arise against the background of mild and borderline mental disorders, tranquilizers help to cope with these conditions through a hypnotic (hypnotic) effect.
Muscle relaxant (relaxing) effect
In psychopathological conditions that cause tension in the skeletal muscles, muscle and motor excitation, the muscle relaxant (relaxing) effect of anxiolytics is useful. However, if the patient’s professional activity or lifestyle is associated with the need to maintain a rapid mental and physical reaction, strict selection of the drug in the correct dosage is necessary. Otherwise, a subjective feeling of lethargy and weakness may appear.
Anticonvulsant effect
The anticonvulsant effect of tranquilizers is usually used for conditions accompanied by epileptogenic activity. In particular, this effect finds therapeutic use in hysteroepilepsia (non-epileptic paroxysmal conditions), non-convulsive epilepsy, neuropsychogenic seizures (for example, breath holding, parasomnia, panic disorder, cardiogenic seizures, tension headaches).
Vegetative stabilizing effect
The therapeutic action profile of some tranquilizers includes a vegetative stabilizing effect - stabilizing the functional activity of the autonomic nervous system. When taking such drugs, autonomic manifestations of anxiety are stopped, for example: rapid heartbeat, high blood pressure, sweating, gastrointestinal disorders.
Rice. 2. The principle of prescribing tranquilizers.
Tranquilizers in neurology: pro and contra
Galina Mikhailovna Dyukova, neurologist, MD, professor of the Department of Nervous Diseases of the Federal Faculty of Physics, Moscow Medical Academy named after. I. M. Sechenov.
Tranquilizers are one of the most frequently prescribed drugs in neurological practice, but neither doctors nor patients should forget that they must be taken with great caution.
The World Health Organization does not recommend the use of tranquilizers for long-term treatment, as they can lead to physical dependence. The duration of treatment with tranquilizers should not exceed 1 month. However, WHO recommendations state that tranquilizers are used only for symptomatic and additional treatment.
Due to their wide range of clinical effects, tranquilizers are used in neurology to treat a number of syndromes:
- psycho-vegetative disorders (permanent and panic);
- pain syndromes (acute and chronic);
- sleep disorders and parasomnia (bruxism, sleepwalking, nightmares, movement disorders: restless legs syndrome, myoclonus, periodic leg movements in sleep, etc.);
- extrapyramidal disorders (tremor, dystonia, myoclonus);
- epileptic disorders (epileptic seizures);
- diseases of the neuromuscular system (rigid person syndrome).
Panic disorders
Tranquilizers are used to treat panic disorders only in the following cases:
1. As first aid to relieve a panic attack.
2. As a drug for course monotherapy, if:
- the duration of the disease is insignificant;
- agoraphobic syndrome and depression are absent.
3. If therapy with antidepressants is impossible due to:
- patient's reluctance;
- intolerance to antidepressants due to side effects;
- In case of combination of panic disorder with epileptic syndromes.
4. In combination with antidepressants:
- as an adjuvant to accelerate the clinical effect,
- for the correction of anxiety and panic disorders, the intensification of which is provoked by the start of taking antidepressants;
- if the dose of an antidepressant is insufficient, and its increase is limited by side effects.
Pain
Tranquilizers are used in neurology to treat both acute and chronic pain. They have a muscle relaxant, analgesic and anti-anxiety effect, due to which their therapeutic effect is formed and the prevention of chronic pain is ensured.
Dream
A number of benzodiazepine tranquilizers have a hypnotic effect and are used as hypnotics. Among them:
- midazolam (Dormikum),
- brotizolam (Lendormin),
- triazolam (Halcion),
- nitrozepam (Radedorm Eunoctin),
- flunitrozepam (Rohypnol),
- bromazepam (Lexotan),
- flurazepam (Dalmadorm).
The first three drugs have the shortest half-life, so they are the most effective and safe as a sleep aid.
Negative aspects of using tranquilizers
Tranquilizers may cause hypersedation. Its main symptoms are: daytime sleepiness, muscle relaxation, lethargy, unsystematic dizziness, psychomotor retardation, decreased concentration and reaction speed. In young people, hypersedation leads to decreased activity and causes difficulties in driving and performing professional duties. In old age, especially with cerebrovascular insufficiency, taking tranquilizers can lead to impaired coordination of movements, ataxia, disorientation and confusion.
In some patients, tranquilizers cause “paradoxical reactions,” that is, instead of a calming effect, they increase aggressiveness, agitation, and sleep disturbances. This effect is typical for impulsive and psychopathic individuals, patients who abuse alcohol or are prone to loss of self-control. In these cases, it is preferable to prescribe antipsychotics.
When taking tranquilizers, physical and psychological dependence can develop, up to the formation of substance abuse. The degree of risk of addiction depends on the drug, its dose, duration of use, withdrawal strategy and the personality of the patient. The risk increases in individuals prone to alcohol abuse, spontaneous increases in doses, and long-term and continuous use of the drug.
If the drug is prescribed incorrectly or is discontinued, o.s. syndrome may develop.
Withdrawal syndrome occurs when there is a sharp decrease in the concentration of the drug in the blood. At the same time, anxiety, irritability, insomnia, weakness, headache, muscle twitching and muscle pain, tremors, sweating, dizziness, nausea, loss of appetite, hypersensitivity to sensory stimuli, impaired perception, depersonalization, and sometimes confusion increase. To avoid withdrawal syndrome, the drug should be gradually withdrawn.
Predictors of withdrawal syndrome are:
- age over 60 years,
- a history of withdrawal symptoms after treatment with other drugs,
- long duration of treatment,
- rapid withdrawal of a high daily dose.
A “rebound phenomenon” may occur with the use of short-acting benzodiazepines. It is manifested by the appearance of anxiety and other symptoms of the disease in the intervals between doses of the drug. To avoid the “rebound phenomenon,” it is recommended to take the drug more frequently or replace it with a long-acting drug.
Features of the tranquilizer "Grandaxin"
Tofisopam (trade name Grandaxin) belongs to the group of benzodiazepine tranquilizers. Is a 2-3 benzodiazepine. Potentiates the binding of other (endogenous) benzodiazepines to benzodiazepine receptors.
Grandaxin has been known to neurologists for quite a long time - since the 80s of the last century. During this time, it has established itself as a drug with unique clinical properties:
- It does not have a sedative-hypnotic effect, but has a slight stimulating effect.
- Does not cause muscle relaxant effect.
- Particularly effective against autonomic disorders that accompany anxiety.
- It has very low toxicity and mild side effects.
- Does not cause either physical or mental dependence.
- There is no development of tolerance to the drug.
- No withdrawal syndrome noted.
In Russia, with the participation of Professor G. M. Dyukova, a large multicenter study was conducted on the effectiveness and tolerability of the tranquilizer Grandaxin (tofisopam) for psychovegetative disorders. The study involved 270 patients aged 18 to 55 years from 11 cities in Russia. The main group (n=162) took Grandaxin at a dose of 150 mg/day, the control group included 108 people.
A 28-day course of therapy with Grandaxin allowed to normalize psycho-vegetative imbalance, increase activity, quality of sleep and life of the subjects. In both groups, treatment had a positive effect on anxiety, however, in the main group, the anxiolytic effect was achieved already by the 2nd week of treatment, in contrast to patients in the control group, which was subjectively perceived by patients as an improvement in well-being, regression of the disease. During therapy with Grandaxin, there was a significant decrease in the level of autonomic dysfunction, noted by the patients themselves and according to objective assessments by doctors.
The supposed psychostimulant effect of Grandaxin was not confirmed by the study data. There was no need to reduce the dose or move it to the morning. An improvement in the quality of night sleep was noted in patients taking Grandaxin, which makes it possible to prescribe it to patients suffering from psychovegetative disorders in combination with insomnia disorders.
Thus, the good tolerability of the drug Grandaxin and the absence of adverse events during treatment allows the drug to be used at a dose of 150 mg/day in patients with both an isolated psycho-vegetative symptom complex and concomitant somatic and neurological pathologies.
Side effects of tranquilizers
Tranquilizers confidently entered minor and borderline psychiatry in the second half of the 20th century as first-choice drugs, displacing antipsychotics and antidepressants, due to the lack of pronounced side effects and good tolerability. The search for new drugs in this group has been going on since 1959, after the first tranquilizer, chlordiazepoxide (Elenium), proved itself to be the best in clinical practice. It is worth noting that today there are more than 50 types of benzodiazepine tranquilizers alone, which have an improved action profile and tolerability.
Abuse and non-medical use
The main side effects of tranquilizers that occur due to abuse or non-medical use of drugs in this group include:
- hypersedation - drowsiness, decreased concentration, memory problems;
- hypermyorelaxation - lethargy, muscle weakness;
- behavioral toxicity - impairment of cognitive functions and psychomotor skills;
- paradoxical reactions - agitation, aggressiveness, sleep disturbances;
- Dependence - mental and physical dependence with manifestations of neurotic anxiety.
Drug intoxication
The effects of abuse and non-medical use of tranquilizers are somewhat similar to barbiturate addiction. The consequences of intoxication depend on the drug taken, however, the severity of the side effects of tranquilizers is small and does not reach serious intellectual, mental and affective disorders. Such drug intoxication can be expressed in a variety of conditions:
- analogue of alcohol intoxication;
- severe lethargy;
- decreased reaction speed;
- drowsiness;
- excessive muscle relaxation;
- increased physical activity;
- euphoria.
The side effects of tranquilizers when used over a long distance are reflected in the appearance and behavior of a person, obvious to others. In such a person, coordination of movements is impaired, the gait becomes sluggish and staggering; speech is unintelligible and confused, but animated; the condition of the skin worsens - it becomes pale; pupils are dilated and react sluggishly to light; the oral cavity is dry, the tongue is covered with a white coating.
Non-medical use of tranquilizers leads to addiction. It is expressed in a change in the nature of intoxication, increasing the dosage of the drug taken in order to achieve the same effect (euphoria). However, euphoria and disinhibition are replaced by irritability and aggression. Ultimately, acute intoxication with tranquilizers leads to the development of a psychotic state - hallucinations, disorders of consciousness, psychomotor agitation. An overdose can lead to coma.
From the somatoneurological side, side effects of tranquilizers can be expressed by the following conditions:
- photophobia;
- hyperhidrosis;
- tachycardia (pulse rate reaches 100 beats per minute);
- hypotension;
- hyperthermia;
- dizziness;
- nausea, vomiting;
- blurred vision;
- tinnitus;
- headaches;
- tactile hypersensitivity;
- olfactory hypersensitivity;
- attacks of fever and chills;
- convulsive seizures.
Treatment for tranquilizer dependence includes drug withdrawal and psychosocial rehabilitation. As a rule, abrupt cessation of taking tranquilizers can cause withdrawal symptoms, accompanied by epileptic seizures, therefore, during treatment, it is necessary to replace it with another (weak) tranquilizer in order to gradually reduce the dosage.
Psychopathology associated with long-term non-medical use of tranquilizers varies from mild anxiety-phobic states to a state of depersonalization-derealization. In addition, in the process of addiction treatment there is a high likelihood of increased low mood, hypochondriacal conditions, lack of initiative and sleep disturbances, which can lead to depression. Having an impact on the quality of life in general, such a person necessarily needs long-term work with a psychotherapist, including in the area of resocialization.
BENZODIAZEPINES
One of the most common tranquilizers. They are widely used in the practice of psychiatrists, psychotherapists, psychiatrists - narcologists, neurologists, cardiologists, surgeons, anesthesiologists and resuscitators. With long-term use they can cause dependence (mental and physical). Benzodiazepine tranquilizers have a specific antagonist (a drug with the opposite effect) - FLUMAZENIL (anexate), which is used to stop breathing and loss of consciousness in cases of overdose and poisoning with benzodiazepines.
- Chlozepid (Librium, Radepur, Chlordiazepoxide, Elenium). The very first benzodiazepine tranquilizer with a strong sedative effect. Sibazon (Relanium, Relium, Seduxen, apaurin, diazepam).
- Bromodihydrochlorophenylbenzodiazepine (phenazepam, elzepam). Domestic development, widely distributed in the countries of the former USSR.
- Nozepam (tazepam, oxazepam).
- Lorazepam (calmese, loram, lorafen).
- Bromazepam (Lexilium).
- Mezapam (rudotel, medazepam).
- Gidazepam.
- Estazolam (nuctanol).
- Clorazepate (Tranxene).
- Clobazam (freesium).
- Alprazolam (Xanax, Zoldac, Neurol). One of the most powerful drugs in this group.
- Tetrazepam (myolostane).
- Tofisopam (Grandaxin). It is distinguished by its ability to have an activating effect.
List of tranquilizer drugs
In the international Anatomical Therapeutic Chemical Classification (ATC), adopted by the Ministry of Health of the Russian Federation in 2002, anxiolytics (N05B) are included in the subsection of the section Drugs for the treatment of diseases of the nervous system (N) - Psycholeptics (N05). This subsection includes six groups of tranquilizers:
- benzodiazepine derivatives (N05BA): Chlordiazepoxide, Medazepam, Oxazepam, Potassium clorazepate, Lorazepam, Adinazolam, Bromazepam, Clobazam, Ketazolam, Prazepam, Alprazolam, Galazepam, Pinazepam, Camazepam. Nordazepam, Fludiazepam, Ethyl loflazepate, Etizolam, Clotiazepam, Cloxazolam, Tofisopam, Lorazepam in combination with other drugs;
- diphenylmethane derivatives (N05BB): Hydroxyzine, Captodiam, Hydroxyzine in combination with other drugs;
- carbamates (N05BC): Meprobamate, Emilkamate, Mebutamate, Meprobamate in combination with other drugs;
- dibenzo-bicyclo-octadiene derivatives (N05BD): Benzoctamine;
- Azaspirodecanedione derivatives (N05BE): Buspirone;
- other anxiolytics (N05BX): Mefenoxalone, Gedocarnil, Etifoxine, Fabomotizol.
Below we present two lists of tranquilizers that can be prescribed for neuroses and neurosis-like mental disorders based on elements of the leading symptoms.
Rice. 1. Formula of the first tranquilizer.
Target - elements of agitation
Mild and borderline mental disorders may be accompanied by elements of agitation: anxiety, panic, fear, overvalued thoughts of fear, obsessive fears, irritability, dysphoria, difficulty going to bed, decreased sleep duration, vegetative lability, vegetative crises. Elements of agitation are the target of the following tranquilizers:
- Diazepam;
- Alprolasam;
- Phenazepam;
- Lorazepam;
- Clonazepam;
- Flurazepam;
- Medazepam;
- Oxazepam;
- Triazolam;
- Bratizolam;
- Tetrazepam;
- Clobazam;
- Gidazepam;
- Nitrazepam;
- Flunitrazepam.
Target - elements of asthenia
Elements of agitation in reversible mental disorders include: mental and physical asthenia, chronic fatigue syndrome, hypochondria, impaired attention and memory, decreased intellectual activity, weakness, fatigue, lethargy, apathy, exhaustion, irritable weakness, autonomic lability, lack of vigor after sleep, anxiety . If such symptoms are present, the following tranquilizers are effective:
- Adaptol;
- Noofen;
- Trioxazine;
- Tofisopam;
- Buspirone.
The choice of a particular tranquilizer depends on the therapeutic goals, the nature of the disease and the individual characteristics of the patient’s health condition. The same applies to the dosage and timing of taking drugs in this group. Refusal of the doctor’s recommendations for taking an anxiolytic (frequency of dosage, recommended dosage, timing of treatment) is unacceptable.
Features of the treatment of neuroses
When selecting a dose of tranquilizers, they are guided by the rule of the minimum sufficient dose. When choosing an initial dose, it must be remembered that patients suffering from any type of anxiety disorder have a significantly lower sensitivity to tranquilizers than healthy people experiencing a severe stressful situation. If effectiveness is insufficient, the dose should be gradually increased, adding a dose equal to the minimum every 3 days. Typically, panic attacks require higher doses than anxiety disorders. Throughout the entire period of treatment, attempts are constantly made to reduce the dose if the patient's condition allows it.
Due to rapid and complete absorption in the gastrointestinal tract, tranquilizers are convenient to use orally. However, if it is necessary to achieve a particularly rapid tranquilizing effect, the medicine can be administered intramuscularly, intravenously, intravenously by drip or rectally. The duration of treatment with this administration should not exceed 3–5 days, after which, if necessary, they switch to taking the drug orally (orally).
Due to the risk of withdrawal syndrome (return of anxiety after abruptly stopping the drug), tranquilizers are discontinued gradually, in the same mode in which the dose was increased.
Tranquilizers can cause mental, physical dependence and addiction (reduced effect of the drug in the initial dose). In this case, it will be necessary to constantly increase the dose, which increases the risk of side effects.
List of used literature
1. Usov L.A., Sufianova G.Z., Minakina L.N. "Pharmacology of the central nervous system."
2. Samarenko V.Ya. "Chemical technology of medicinal substances."
3. Bakumov P.A., Evseev A.V. "The use of tranquilizers in therapeutic practice."
4. Murashko N.K. "Psychopharmacotherapy of cardioneurological patients."
5. Serov V.N., Baranov I.I. "Tranquilizers in obstetric and gynecological practice."
6. Verbenko V.A., Verbenko N.V. "Psychotropic drugs in therapeutic practice."
7. Malin D.I. "Critical illness therapy in psychiatry"
8. Drobizhev M.Yu., Ovchinnikov A.A. "Pathogenetic psychopharmacotherapy of anxiety disorders."
9. Ivashchenko D.V. "Safety of the use of tranquilizers from the group of benzodiazepines in alcohol withdrawal syndrome: pharmacoepidemiology and pharmacogenetics."
Share
Share
Use of tranquilizers
The main indications for taking these drugs are mild mental disorders and behavioral disorders:
- Neuroses. Neurosis-like conditions.
- Personality disorders.
- Anxiety disorders: panic attacks, phobias, generalized anxiety disorder, mixed anxiety and depressive disorder.
- Withdrawal state (withdrawal syndrome) with alcohol, nicotine, drug addiction, substance abuse and polydrug addiction.
- Depression with anxiety.
- Schizotypal disorder.
- Acute psychoses (in combination with other drugs).
- Consequences of organic damage to the central nervous system with mental disorders
- Behavioral disorders in children and adolescents.
- Insomnia.
- Eating disorders (anorexia, bulimia).
- Psychosomatic diseases: eczema, irritable bowel syndrome, “neurogenic bladder”, asthma attacks, hypertension and arrhythmia.
In addition, they are widely used in neurological practice: consequences of traumatic brain injuries, strokes with increased muscle tone, epilepsy, spinal osteochondrosis, etc. In therapeutic practice: functional disorders in the gastrointestinal tract, cardiovascular, urinary and other body systems.
Is it possible to take tranquilizers on your own without a doctor?
No. These are psychotropic drugs that have their own contraindications and limitations. Self-administration is life-threatening.
Can you buy tranquilizers without a prescription?
No. They are prescribed only on prescription by a doctor who has grounds for prescribing this drug. Two tranquilizers are prescribed on special strict reporting prescription forms (form 148 - 1/u - 88), these are sibazon and alprazolam.
What are the most powerful tranquilizers?
Sibazon and alprazolam.
What are daytime tranquilizers?
Since most tranquilizers tend to cause daytime sleepiness, drugs have been synthesized without this side effect. These include: gidazepam, clorazepate, tofisopam, hydroxyzine, mebicar.
What is the difference between tranquilizers and antidepressants? Do they have anything in common?
The difference between them is in the mechanisms of action (they act on different types of receptors). They have different therapeutic effects (anti-anxiety and antidepressant, respectively). Tranquilizers are often prescribed once or in short courses, antidepressants are prescribed for a long time, several months.
What they have in common is that they are all psychotropic drugs. Some drugs from these groups can give a hypnotic, sedative and anti-aggressive effect.
Cost of treatment in our clinic
| Service | Price | |
| Ambulatory treatment | ||
| Psychiatrist consultation | 4 500 ₽ | |
| Consultation with a psychotherapist | 4 500 ₽ | |
| Psychodiagnostics extended | 7 000 ₽ | |
| Consultation with a psychiatrist at home | 6 000 ₽ | |
| Treatment in hospital | ||
| Delivery to hospital | For free | |
| Standard room | 7 700 ₽ | |
| 3-bed superior room | 10 600 ₽ | |
| 2-bed superior room | 13 700 ₽ | |
| 1 local VIP chamber | 19 000 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Basics of treatment of neuroses
In psychiatry, tranquilizers are used for anxiety disorders, anxiety disorder with panic attacks, phobias, and to relieve stress-induced mental reactions, such as grief.
Tranquilizers are used occasionally, mainly to relieve episodes of panic or when anxiety increases to a degree that disrupts the patient's behavior.
To reduce the risk of developing addiction, tranquilizers should be used in short courses (from two weeks to a month). If it is impossible to complete treatment after 4 weeks, it is recommended to take short breaks of 2-3 days during the week. Thus, anxiolytics can be used quite safely for up to several months.
Usually the drugs are used in the evening, before bedtime, given the hypnotic effect of most tranquilizers. The exception is “daytime” tranquilizers (gidazepam), which can be used at any time of the day.