Stages of disease development
The pathogenesis of a brain abscess involves four stages of its development:
- Early brain inflammation (1-3 days). The patient develops encephalitis, a limited inflammation of brain tissue. The important thing is that at this stage it is still quite possible to reverse the disease. The inflammatory process can end spontaneously or upon completion of antibacterial therapy.
- Late stage (4-9 days). This stage occurs when the protective functions of the patient’s body are weakened or due to incorrectly chosen treatment tactics. Therefore, the inflammation begins to progress - the cavity filled with pus begins to increase in size.
- Early encapsulation (10-13 days). This stage of inflammation is characterized by necrosis of the central part of the brain, as well as the formation of a capsule that limits the further spread of pus.
- Late encapsulation (starting from day 14). Starting from the second week after activation of the inflammatory process, the patient is diagnosed with a clear collagen capsule filled with pus and surrounded by a zone of gliosis. The further development of inflammation depends on the reactivity of the patient’s body, the virulence of the flora, and proper treatment. Often at this stage there is an increase in the volume of purulent content and the formation of new foci of inflammation.
General cerebral symptoms
General cerebral symptoms arise due to sudden jumps in intracranial pressure. The most common symptom of the pathology is headache accompanied by vomiting. The patient may experience problems with vision: often, against the background of an abscess, optic neuritis develops, and congestive discs appear in the fundus. The clinical picture of the disease also includes mental disorders, inhibition of thought processes, lethargy, weakness, and apathy. In the case of intracranial hypertension, epileptic seizures may occur. Most patients also experience persistent drowsiness, and in the most severe cases, coma may occur.
Course of a brain abscess
As for the course of the disease, it often has a very violent and acute onset, which is characterized by focal and hypertensive manifestations. The inflammatory process almost always develops against a background of elevated temperature. In rare cases, the onset of the disease may be less pronounced and resemble the clinical picture of meningitis. However, with minimal symptoms and normal temperature, the first stage of the disease is extremely rare.
After 5-30 days, the disease passes into the next, latent, stage, which is characterized by either a complete absence of any symptoms, or minimally expressed signs of the disease. The patient may complain of severe and regular headaches, mental retardation and vomiting. The duration of this stage varies: in some patients it lasts a couple of days, while in others it lasts several years. Then, due to the influence of some factor (for example, infection), this stage ends and the patient’s symptoms begin to actively progress. The most severe and life-threatening consequence of a brain abscess is its rupture, which usually leads to death.
Clinical picture
The disease begins acutely and is manifested by signs of intoxication syndrome, focal and cerebral symptoms.
Patients experience increased body temperature, headache, chills, hyperhidrosis, pale skin, weakness, lack of appetite, dry mouth, leukocytosis in the blood, increased ESR. These are signs of severe intoxication.
The following symptoms are general cerebral:
- unbearable headache,
- nausea and vomiting that does not bring relief,
- bradycardia,
- lacrimation and photophobia,
- tension and spasm of the neck muscles,
- psychoses,
- lethargy and apathy,
- drowsiness,
- dizziness,
- loss of consciousness,
- causeless mood swings,
- seizures,
- coma.
Focal neurological symptoms
allows you to diagnose pathology based on its clinical signs.
The clinical picture of a brain abscess is determined by its location:
- Localization of the lesion in the right hemisphere is manifested by paresis and paralysis of the left half of the body.
- Symptoms of abscess of the temporal lobe of the brain are visual dysfunction, dysphonia or aphonia, convulsions of the whole body and limbs. The patient develops sensory aphasia, speech becomes meaningless, he cannot read and write, and does not understand what others are saying. Mental disorders are manifested by euphoria or depression, decreased criticism.
- Abscess of the frontal lobe - foolish and high spirits, euphoria, slurred speech, increased talkativeness, decreased intelligence, delirium, mood swings from joy to sadness.
- Damage to the cerebellum is manifested by nystagmus, incoordination of movements, ataxia, hypertension syndrome, and muscle hypotonia. The movements of patients become sweeping and unclear, their gait is unsteady with falls, their eyes “run” from side to side.
- Abscess of the base of the brain - dysfunction of the oculomotor system, development of strabismus, loss of vision, convulsions, paralysis of the limbs.
Clinical signs associated with stroke and cerebral edema may appear. The close location of the abscess to the meninges is manifested by meningeal symptoms and signs - stiff neck, gundog posture, increased sensitivity to touch.
Complications of a brain abscess are: herniation of an abscess, its breakthrough into the ventricles of the brain, relapses, secondary infection of a postoperative wound, inflammation of the skull bones - osteomyelitis, the occurrence of repeated epileptic seizures. Clinically, these processes are manifested by paralysis and paresis, loss of vision and hearing, memory impairment, decreased intelligence and other dysfunctions of the central nervous system.
Diagnosis of brain abscess
Timely comprehensive diagnosis of brain abscess is important in its further treatment. To make a diagnosis, a neurologist uses medical history and examination results of the patient, as well as information obtained during instrumental and laboratory tests. The following methods are used to diagnose the disease:
- General blood analysis. The disease is usually indicated by test results such as an increase in ESR and pronounced leukocytosis. At the stage of capsule formation around the abscess, a normal or slightly increased number of leukocytes is observed in the patient’s blood.
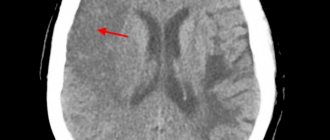
- CT scan. The accuracy of detecting an abscess using this technique depends on the stage of the pathology. In the early stages, an abscess is very difficult to detect. At the stage of encephalitis, CT may reveal an area of reduced density that has an uneven shape. At this stage, the contrast agent accumulates unevenly - often only in the peripheral areas. It is much more accurate to diagnose the disease at a late stage in the development of encephalitis.
- Magnetic resonance imaging. This is a more accurate and effective method of diagnosing an abscess, which allows it to be detected at an early stage. Since the technique is considered the most informative, treatment can be prescribed based on its results even without bacteriological tests.
- Echoencephaloscopy. This diagnostic method is usually prescribed if for some reason MRI and CT cannot be performed. Using this study, it is possible to detect displacement of brain structures, which indicates compression of its tissues by an abscess.
- Bacteriological research. This technique involves taking a puncture of pus from the abscess for examination. A detailed examination of the pus helps to identify the causative agent of inflammation, which then makes it possible to select the most appropriate tactics of drug therapy.
- X-ray of the skull. This technique is used to detect the source of infection that caused the abscess.
- Craniography. Prescribed to detect symptoms of intracranial hypertension.
Diagnostics
In order to accurately diagnose the location of the brain and cerebellum abscess, computed tomography and magnetic resonance imaging of the brain are performed.
When performing a computed tomography scan, a thin, smooth wall of the abscess is revealed, which has regular contours. Magnetic resonance imaging can also determine the abscess capsule. If it is not possible to carry out the above types of research, pneumoencephalography or radioisotope scintigraphy of the brain can be performed. Abscess of the brain and cerebellum should be distinguished from purulent meningitis, non-purulent local encephalitis, serous leptomeningitis (arachnoiditis), purulent labyrinthitis. With meningitis, there is a high temperature and tachycardia (increased heart rate), and with an abscess, the body temperature is low-grade and there is severe bradycardia. Patients with meningitis are excited, and with an abscess they are drowsy and lethargic; there is a characteristic “congestive nipple” in the fundus. You can distinguish between meningitis and an abscess by examining the cerebrospinal fluid: with meningitis there will be high pleocytosis, and with an abscess there will be moderate pleocytosis and an increase in the amount of protein. With arachnoiditis, there are no changes in the cerebrospinal fluid. Unlike encephalitis, with a brain abscess there are no symptoms of intoxication.
Differential diagnosis of brain abscess
Since the majority of symptoms of brain abscess are not specific, differential diagnosis plays an important role. If the doctor has doubts during diagnosis, he may prescribe MR spectroscopy. This technique is carried out in order to differentiate a brain abscess from tumors of the cerebral hemispheres. It is based on different contents of lactate and amino acids in tumors and purulent accumulations.
As for other diagnostic methods, they are considered less informative. For example, signs such as an increase in C-reactive protein in the blood, chills, an increase in ESR, and leukocytosis may indicate a variety of inflammatory processes. Blood cultures from an abscess are often sterile.
Treatment of brain abscess
Treatment for a brain abscess usually involves both drug therapy and surgery. Doctors select the most optimal treatment tactics based on the results of diagnosing the disease, as well as the general health of the patient. The stage of the disease is also taken into account. For example, in the early stages of abscess formation, conservative treatment can be used. If an abscess has already formed, and a dense capsule has formed around it, neurosurgical intervention cannot be avoided.
- Drug treatment
- Surgery
Drug treatment of brain abscess involves the prescription of antibiotics, decongestants and anticonvulsants. Since the inflammatory process is provoked by bacteria, treatment of the disease necessarily involves their destruction. The combination of penicillin and chloramphenicol has been considered the most standard and commonly used treatment regimen for brain abscess for decades.
Penicillin was prescribed to treat the disease because it can kill streptococci and most other bacteria that can cause brain abscess. Chloramphenicol was used because of its ability to easily dissolve in adipose tissue and destroy anaerobic bacteria.
Today doctors are slightly adjusting this scheme. For example, cefotaxime is prescribed instead of penicillin, and metronidazole is prescribed instead of chloramphenicol. Typically, the doctor prescribes antibiotic therapy several weeks before surgery. The duration of taking antibiotics can be about 6-8 weeks.
Patients whose brain abscess occurs due to immunodeficiency are also prescribed amphoreticin. If the abscess has resolved, the patient will need to take a course of fluconazole for ten weeks. Drugs such as sulfadiazine and pyrimethamine are commonly included in the treatment regimen of patients with HIV.
Of great importance in the treatment of the disease is the correct identification of the causative agent of infection using an antibiogram. However, there are cases when the culture turns out to be completely sterile. Therefore, in such situations, empirical antibiotic therapy is prescribed.
In addition to antibiotics, medications are also prescribed to help reduce swelling. For example, glucocorticoids are used for this purpose. However, the prescription of these drugs is indicated only in case of a positive result from antibacterial therapy. They can reduce the severity of a brain abscess and reverse the development of the capsule around it. However, the opposite effect is also possible, when glucocorticoids activate the spread of inflammation beyond the boundaries of the lesion. To eliminate convulsive manifestations, phenytoin is usually prescribed.
If a brain abscess is diagnosed in the late stages, and a dense capsule has already formed around it, it is impossible to do without surgery. To treat the disease, puncture aspiration and removal of the abscess are most often used.
As for puncture aspiration, it is advisable to prescribe it in the early stages of the pathology. In this case, antibacterial therapy should be carried out simultaneously. Indications for this procedure may also include multiple abscesses, a deep location of the abscess, the stage of cerebritis and a stable neurological condition of the patient. To ensure that the procedure is performed as accurately as possible, the doctor resorts to stereotactic biopsy and intraoperative ultrasound.
Needle aspiration has one important drawback - in most cases, a repeat procedure may be required after it is performed. In difficult cases, complete removal of the abscess is prescribed. This technique is also prescribed if they want to avoid a possible relapse of the disease. It is advisable to remove an abscess for the following indications: if antibacterial therapy or puncture aspiration are not effective, with a superficial abscess and a well-formed capsule around it.
If multiple abscesses were discovered in a patient during diagnosis, then first you need to drain the inflammation to prevent pus from breaking into the ventricular system of the brain. If neurological disorders increase or there is no positive dynamics on MRI and CT, a repeat operation may be prescribed.
Treatment
Treatment of a brain abscess is aimed at destroying infectious agents and signs of inflammation, improving microcirculation in the affected area, eliminating the main clinical signs and strengthening the body as a whole. Treatment is carried out in a neurosurgical hospital.
Depending on the stage of the disease, the location of the abscess and its size, conservative or surgical therapy is carried out.
Drug treatment
Conservative therapy is carried out at the initial stage of the pathology, and also when the size of the abscess does not exceed three centimeters in diameter.
- Antibacterial therapy - the use of broad-spectrum antibiotics from the group of cephalosporins, macrolides, fluoroquinolones, protected penicillins, antifungal drugs. Patients are prescribed Ceftriaxone, Metronidazole, Vancomycin, Levomycetin, Amphotericin, Fluconazole. After receiving the results of an analysis of the sensitivity of the isolated microbe to antibiotics, treatment must be adjusted.
- Glucocorticoids are prescribed in cases where antibiotic treatment does not produce positive results. Glucocorticosteroids reduce the severity of inflammation and reverse the development of the abscess capsule. Prednisolone and Dexamethasone are usually prescribed.
- Drugs that improve cerebral circulation - Vinpocetine, Cerebrolysin, Piracetam, Actovegin.
- Medicines that prevent seizures - “Difenin”, “Alepsin”, “Sodanton”.
- Diuretics and decongestants - Mannitol, Furosemide, Lysix.
- Anti-inflammatory and antipyretic drugs - Paracetamol, Ibuprofen.
- General strengthening therapy - B vitamins, adaptogens, antihypoxants.
Surgery
After stabilization of the patient's general condition, the abscess is opened and drained. The purulent cavity is irrigated with an antibacterial solution. After the operation, the patient spends some time in the intensive care unit, and then he is transferred to the ward to a neurological bed. After such surgery, a long rehabilitation period is required.
surgery
Indications for surgery:
- Localization of the abscess in the ventricular zone of the brain,
- Abscess causing hypertension syndrome
- Abscess resulting from traumatic brain injury
- Abscess of fungal origin.
Contraindications:
- The initial stage of the pathology is encephalitis,
- The location of the abscess in the immediate vicinity of vital centers,
- Multiple inoperable abscessive lesions of the brain,
- Comatose state of patients.
The prognosis of the disease is very serious, but in most cases it is still favorable. Mortality from brain abscess is up to 30%, and disability is up to 50%. Even after recovery, almost half of the patients still have neurological symptoms – seizures. Some people lose various functions of the body.
Measures to prevent the formation of an abscess in the brain:
- Wound disinfection for TBI,
- Timely identification and sanitation of foci of chronic infection,
- Stimulates the immune system and increases the body's resistance to infections,
- Balanced and proper nutrition,
- Taking multivitamins and mineral complexes.
A brain abscess is a serious pathology that occurs against the background of existing diseases in the body. In order to detect the disease in a timely manner and begin treatment immediately, it is necessary to know the first clinical symptoms and be able to apply additional research methods. Early and adequate therapy can reduce the risk of developing life-threatening complications and minimize the negative consequences for the body.
Prognosis for brain abscess
The outcome of the disease depends on whether the doctor was able to identify the causative agent of the abscess from culture. It is extremely important to do this, since then it will be possible to determine the sensitivity of bacteria to antibiotics and select the most appropriate treatment regimen. The prognosis for the health of a patient with a brain abscess also depends on the number of purulent accumulations, the patient’s health status, and the correct treatment tactics.
The risk of various complications with a brain abscess is very high. Namely, about 10% of all cases of the disease end in death, and 50% result in disability. In addition, most patients may develop epileptic syndrome after treatment, a condition characterized by the occurrence of epileptic seizures.
Doctors give less favorable prognoses to patients who have been diagnosed with subdural empyema. In this case, the patient does not have a clear boundary of the purulent focus due to the high activity of the infectious agent or the body’s insufficient resistance to it. Lethal cases with subdural empyema reach 50%.
The most dangerous form of brain abscess is considered to be fungal empyema, which is accompanied by immunodeficiency. This disease has practically no cure, and the number of deaths with it is about 95%. In turn, epidural empyemas have a more favorable prognosis and are almost never accompanied by complications.
Prevention of brain abscess
There are no effective methods for preventing brain abscess. However, with the help of several preventive measures, the risk of the disease can be significantly reduced. In particular, in the case of traumatic brain injury, the patient must receive adequate surgical care.
The disease can also be prevented by timely elimination of foci of infection (pneumonia, boils), treatment of purulent processes in the inner and middle ear, as well as the paranasal sinuses. Good nutrition also plays a great role in the prevention of brain abscess.
Brain abscess
Brain abscess is a limited purulent-inflammatory process in brain tissue. Clinically, there is a combination of symptoms of a brain space-occupying lesion and an inflammatory process. Less common are epidural and subdural abscesses. A brain abscess is a limited cavity in the thickness of the brain tissue filled with pus. For abscesses to occur, it is necessary that a pyogenic microbe (streptococcus, staphylococcus, E. coli) enter the brain tissue.
Typically implemented in three main ways.
Firstly, with hidden injuries to the skull (trauma and surgery), the infection can enter the brain directly with hair, pieces of clothing, and bone fragments.
Secondly, the microbe can be brought with the blood or lymph flow if there is some kind of purulent inflammatory process in the body (pneumonia, erysipelas on the skin, furunculosis, sore throat, sore tooth).
Thirdly, the infection can enter the brain from the paranasal sinuses (sinusitis, sinusitis) or from the cavity of the inner ear (otitis media) through a thin bony septum separating them from the cranial cavity.
The peculiarity of a brain abscess is that under certain circumstances (use of strong antibiotics) the source of infection can become encysted, i.e. a fencing shaft is formed around it. Behind this barrier, an infection can remain silent for a long time, but when the vital forces of the body decrease (colds, stress, hunger, old age), an abscess can begin to develop again.
Symptoms and course:
Brain abscess is manifested by general infectious, cerebral and local (focal) symptoms. The latter characterize the localization of the abscess.
General infectious symptoms: fever (sometimes intermittent), chills, blood leukocytosis, increased ESR, signs of a chronic infectious process (pallor, weakness, weight loss).
General cerebral symptoms appear due to increased intracranial pressure caused by an abscess. The most consistent symptom is headache, often with vomiting. In the fundus there are congestive discs or optic neuritis. Bradycardia up to 40-50 beats per minute and mental disorders are periodically detected. Noteworthy is the patient's lethargy and apathy, and the slowness of his thinking. Stupefaction and drowsiness gradually develop; in severe cases without treatment - coma. As a consequence of intracranial hypertension, general epileptic seizures may occur.
Focal symptoms depend on the location of the abscess in the frontal, temporal lobes, and cerebellum. Abscesses located deep in the hemispheres outside the motor zone may occur without conduction symptoms. Otogenic abscesses sometimes form not on the side of otitis media, but on the opposite side, giving the corresponding clinic. Along with focal symptoms, symptoms associated with swelling and compression and dislocation of brain tissue may be observed. When the abscess is close to the membranes and with a cerebellar abscess, meningeal symptoms are detected.
In the cerebrospinal fluid, pleocytosis (25-300 cells), consisting of lymphocytes and polynuclear cells, increased protein levels (0.75-3 g/l) and increased pressure are detected. However, often the cerebrospinal fluid is normal
Recognition:
Making a diagnosis can be difficult, so you should know that diseases of the ENT organs, teeth, pneumonia, head injuries, boils, can lead to brain abscesses. A headache lasting more than 12 hours is a cause for serious concern, and accompanied by an increase in temperature, mental changes, and depression of consciousness is a direct indication for calling an ambulance.
Treatment:
Treatment is medicinal with the use of various antibiotics, vitamins (Supradin, Neuromultivit, Complivit) and nootropic drugs (Nootropil, Piracetam, Pirabene) and neurosurgical, which consists of removing the abscess. The prognosis is usually favorable. The mortality rate is below 10%.